-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1398-1400
doi:10.5923/j.ajmms.20241405.54
Received: Apr. 21, 2024; Accepted: May 17, 2024; Published: May 23, 2024

Impact of Sodium Imbalance on Outcomes in Patients with Severe Traumatic Brain Injuries
Krasnenkova M. B.
Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Krasnenkova M. B., Tashkent Medical Academy, Tashkent, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

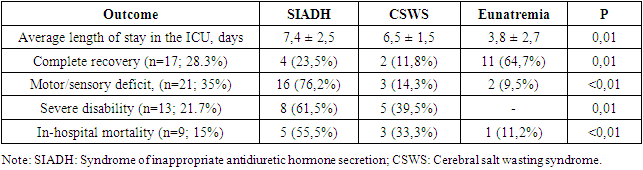
Hyponatremia is the most common electrolyte imbalance in patients with TBI. The role of hyponatremia as a negative prognostic indicator in patients with TBI remains controversial. The purpose of the study was to evaluate the incidence of hyponatremia in patients with STBI and determine its impact on in-hospital outcome of the disease. The article presents the results of a study of electrolyte disturbances identified in 60 patients with severe brain contusions in the first three days after receiving a head injury. Hyponatremia was defined as serum sodium ≤ 130 mmol/L; hypernatremia - serum sodium ≥ 146 mmol/l; The presence of dysnatremia was associated with in-hospital mortality and poor functional outcome. Hypernatremia, acidosis, and hyperglycemia significantly increase the risk of death in the first 24 hours after TBI.
Keywords: Hyponatremia, Severe Traumatic Brain Injury, Prognosis, Cerebral Salt Wasting Syndrome, Syndrome of Inappropriate Antidiuretic Hormone
Cite this paper: Krasnenkova M. B., Impact of Sodium Imbalance on Outcomes in Patients with Severe Traumatic Brain Injuries, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1398-1400. doi: 10.5923/j.ajmms.20241405.54.
Article Outline
1. Introduction
- Hyponatremia (serum sodium <135 mmol/L) is the most common electrolyte imbalance, occurring not only in the general population but also in patients with severe brain injury. [1]. Hyponatremia may result from syndrome of inappropriate antidiuretic hormone (SIADH), diabetes insipidus (DI), or cerebral salt wasting syndrome (CSWS) [2]. These three conditions are the most common causes of dysnatremia and the most difficult to diagnose in neurocritical care patients. [3]. Antidiuretic hormone (ADH) is a pituitary hormone that regulates the amount of water in the body by affecting the kidneys. Physiologically, ADH is secreted in response to a decrease in plasma volume or an increase in serum osmolality. In SIADH, ADH is secreted continuously due to disruption of the negative feedback mechanism, which leads to increased water resorption in the kidneys and, as a consequence, to dilutional hyponatremia [4-6]. Increased ADH release combined with excess fluid administration results in increased extracellular fluid and hyponatremia without clinical fluid overload [7,8]. CSW is a hyponatremic condition characterized by urinary sodium loss and decreased extracellular fluid volume in the setting of critical neurological conditions and normal renal function [9,10]. Hyponatremia in CSWS is caused by large losses of sodium in the urine [11]. Central diabetes insipidus is defined as the inability to retain and maintain adequate levels of free water, which manifests as polyuria (urine volume greater than 40 ml/kg/24 hours) [12,13]. May be caused either by a deficiency of plasma ADH caused by its inadequate synthesis, release or transport from the hypothalamus (central) or by an inadequate renal response (nephrogenic) [14]. Regardless of the etiology, any sodium imbalance is associated with significant morbidity, mortality, and increased length of hospital stay [15]. However, studies examining the association of hyponatremia with mortality in patients with TBI are inconsistent. The purpose of our study is to assess the incidence of hyponatremia in patients with TBI and determine its relationship with early treatment results.
2. Material and Research Methods
- The study included 60 patients with severe traumatic brain injury admitted to the ICU. The average age of the patients was 31±6 years, 49 men and 11 women. Among them, 40 (70%) had a level of consciousness assessed at 8 points on the Glasgow Coma Scale (GCS), 12 (20%) had a GCS score of 6 - 7 points, and 6 (10%) had a GCS score of 4 - 5 points. All patients were operated on for subdural or epidural hematomas of various locations. Of these, 9 (15%) patients died on the first day after injury. Intensive care was provided according to the standard protocols, according to the Trauma Foundation Guidelines (2017). All victims were given artificial pulmonary ventilation (ALV) and vital signs were monitored. Laboratory tests were performed on all patients pre- and postoperatively, including complete blood count and serum electrolyte levels, as well as acid-base and blood gas parameters. During the first 3 days from admission, plasma concentrations of potassium, sodium, magnesium and glucose were assessed. Upon review of biochemical test results, hyponatremia was defined as serum sodium ≤ 130 mmol/L; hypernatremia - serum sodium ≥146 mmol/l; hypokalemia was defined as a serum potassium level <3.5 mmol/L and hyperkalemia was defined as a serum potassium level >5.0 mmol/L. A normal serum magnesium level was considered to be 1.0 to 2.0 mmol/L and a normal serum bicarbonate level to be 22 to 26 mmol/L. Statistical processing of the obtained data was carried out using Microsoft Excel software. The reliability of statistical indicators was assessed based on the criteria standard deviation M±m, t - Student's test, p. The P value ≤0.05 was considered significant.
3. Results and Discussion
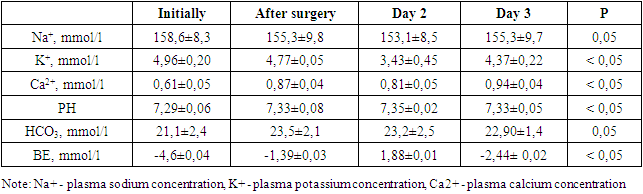
- In patients with TBI, sodium imbalance, particularly hypernatremia, is the most common among all serum electrolytes. However, in our study, before surgery, hypernatremia was noted in 15 (25%) patients, and hyperkalemia in 45 patients (75%). We also found that hypernatremia occurred more frequently in the postoperative period. Combined metabolic and respiratory acidosis were the most common disorders in the preoperative period, which were detected in 28 patients (70%) with STBI. Hypernatremia was also a common condition of electrolyte imbalance after surgery, which was followed by hyponatremia and hypokalemia in 50% of cases. Hyperglycemia in the perioperative period was noted in all patients. Thus, the glucose level fluctuated from 6.5 to 9 mmol/l, against the background of corrective therapy. The results obtained are reflected in the following table 1.
|
|
4. Conclusions
- The risk of developing electrolyte abnormalities in patients with TBI depends on the severity of injury, comorbidities, age, and primary therapeutic strategy. Intensive care methods, such as the choice of the type of infusion solution, the administration of mannitol or hypertonic sodium chloride solutions, the use of diuretics and hyperventilation also affect the water-electrolyte and acid-base composition of the blood of victims. Perioperative hypernatremia, acidosis, and hyperglycemia significantly increase the risk of death in the first 24 hours after TBI.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML