-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1389-1392
doi:10.5923/j.ajmms.20241405.52
Received: May 1, 2024; Accepted: May 20, 2024; Published: May 22, 2024

Pathomorphology of Stroke of the Middle Cerebral Artery in COVID-19
Shakhzod N. Khodjaev, Erkin A. Eshbaev
Republican Pathology Center, Тashkent Medical Аcademy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article examines the morphogenesis and morphology of stroke that developed in the basin of the middlecerebral artery of the brain, complicated by covid-19. Patients who died from COVID-19 complications during 2020-2021 at the Zangiota Infectious Diseases Clinical Hospital were subjected to a retrospective analysis of autopsy materials. The results of the study showed that in COVID-19, the cerebral hemisphere with the basin of the middle cerebral artery, forehead, upper and cheek fragments, there was a focus of ischemia of different sizes on the lateral surface, more in the right hemisphere (57.1%), the rest in the left hemisphere (42.9%). It was noticed that the thrombus that arose in the initial section A1 of the middle cerebral artery passing between the processes of the brain was predominantly fibrin, a red thrombus formed inside the brain tissue, the focus of cerebral infarction differed from atherosclerotic infarction, almost all blood vessels around the focus of ischemia in coronavirus had endotheliitis, microangiopathy.
Keywords: COVID-19, Brain, Arteries, Middlecerebral artery, Endotheliitis, Thrombosis, Ischemic infarction, Stroke
Cite this paper: Shakhzod N. Khodjaev, Erkin A. Eshbaev, Pathomorphology of Stroke of the Middle Cerebral Artery in COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1389-1392. doi: 10.5923/j.ajmms.20241405.52.
Article Outline
1. Introduction
- In COVID-19, damage to blood vessels leads to disruption of important pathophysiological aspects of organs and systems. The SARS-cov2 virus enters the human body by endocytosis. APF-2 then binds to the “Spike protein” of the receptor, which in most cases is expressed in endothelial cells, including cerebral vessels. Endothelial dysfunction leads to a decrease in the amount of free oxide, the release of inflammatory cytokines, increased permeability of the vessel wall, interstitial inflammation and activation of coagulation. Systemic virus damage and cytokine attack, microangiopathy of small vessels, endotheliitis and vasculitis cause hypercoagulation syndrome and are manifested by thrombosis and thromboembolism [1,2,3,4]. These pathophysiological processes can be explained by the presence of risk factors in the body of patients, namely old age, hypertension, atherosclerosis, chronic cardiovascular diseases, cerebrovascular diseases, diabetes mellitus [5,6,7,8].A severe consequence of COVID-19 is considered to be a stroke. It was noted that during the pandemic, the incidence of strokes increased dramatically, which led to bad consequences. The specificity of coagulopathy, especially developed as a result of coronavirus infection, was the development of acute cerebral circulatory disorders, caused by infectious thrombotic occlusion of large arteries not associated with atherothrombosis. It has been observed that ischemic stroke associated with covid-19 is caused by acute inflammatory vasculopathy and thrombosis of large cerebral arteries. In most cases, an ischemic stroke develops in the basin of the middle cerebral artery [9,10,11,12].
2. Materials and Methods
- Patients who died from COVID-19 complications during 2020-2021 at the Zangiota Infectious Diseases Clinical Hospital were subjected to a retrospective examination of the autopsy material. A total of 42 materials were obtained from patients in whom coronavirus infection was determined by PCR of SARS-Cov2 viral RNA by the number of IgM IgG class antibodies. Of these, 23 (54.7%) were men, 19 (45.3%) were women. The average age of the patients was 68.4 years (41-85 years). Almost all patients (93.4%) had from 1 to 3 concomitant diseases. Hypertension was found in 32 (74.5%), diabetes in 15 (35.7%), cerebrovascular diseases in 11 (26.2%), obesity in 10 (23.8%), coronary heart disease in 24 (57.1%), chronic lung diseases in 7 (16.7%).During the autopsy, the entire extracted brain was solidified a day in a 10% formalin solution and placed on a table with the base of the brain down, the frontal part to the right and was cut using Fleksig method. Virchow's knife, immersed in water and soaked 2 fingers wide above the surface of the table, was cut horizontally in both hemispheres of the brain. This incision should pass over the corpus callosum, over the cerebellum worm, and this incision does not violate the topography of the brain, and the third and lateral ventricles open. By placing the hand under the cerebellum, the fourth ventricle opens. To fully explore the hemispheres of the brain, the upper and lower parts of the brain were cut with frontal incisions. The fragments were taken from the regions of the cerebral hemisphere, where all the arteries supplying blood to brain tissue are located, including the initial (A1), middle (A2) and final (A3) branches of the middle cerebral artery. The branches of the middle cerebral artery coincide with the anterior pedicle of the inner capsule, with the lateral surface of the forehead, upper and buccal parts, fragments of brain tissue were taken from these areas.The brain fragments were solidified for 72 hours in a 10% formalin solution with a phosphate buffer. After 4 hours of rinsing in running water, it is dehydrated in high-concentration alcohols and chloroform. Pieces of tissue were soaked in paraffin with wax and blocks were made.Slices 4-5 microns thick were made from paraffin blocks, dewaxed in a thermostat and stained with hematoxylin and eosin. The composition of the tissue was stained with alcyan blue dye for research intermediate changes in the wall of blood vessels and surrounding adventitious tissues under the influence of coronavirus, i.e. the degree of formation of acidic mucopolysaccharides. Qualitative and quantitative changes in elastic fibers, which are important fibrous structures in the vascular wall, were studied by staining using the Weigert method. Histological preparations were studied on 10, 40, 100 microscope objects, and a computer image of the vessels of the microcirculatory bed was made.
3. Research Results and Their Discussion
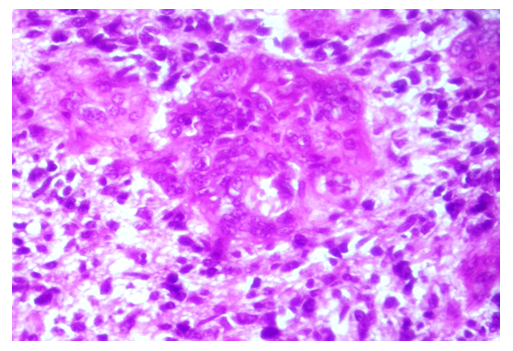
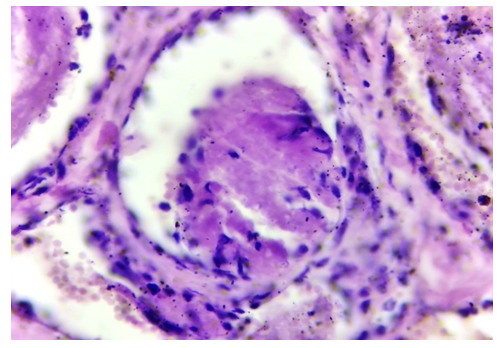
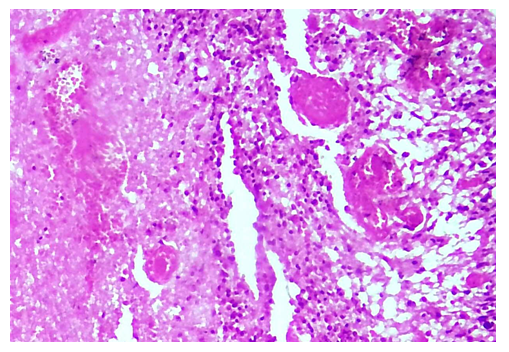
- A macroscopic examination of the brain isolated during the autopsy yielded the following results. There are edema of the soft meninges, the venous sinuses in them are full, the folds on the surface of the hemispheres are slightly flattened, the chins are filled with edematous fluid. When cutting the brain, the middle cerebral artery of the hemisphere with a basin of forehead, upper and cheek fragments on the lateral surface, foci of ischemia of different sizes were found. More in the right hemisphere (57.1%). It was noticed that the rest are located in the left hemisphere (42.9%). It was found that the foci of ischemic infarction in most cases occupy a place in the periventricular region of these sections. In some cases, the focus of ischemia is detected somewhat and the presence of hemorrhages around it.Initially, when examining the middle artery of the brain, it was found that the thrombosis process is localized in the middle part of the artery, and in some cases in its initial part. The branches of the middle cerebral artery coincide with the anterior pedicle of the inner capsule, with the lateral surface of the forehead, upper and buccal parts, fragments of brain tissue were taken from these areas. The thrombus found in the initial section A1 of the middle cerebral artery, passing between the processes of the brain, consists mainly of fibrin (Fig.1), and lymphoid cells are found in its peripheral areas. In the case when one surface of the thrombus adheres to the artery wall, a proliferative infiltrate of lymphoid and histiocytic cells forms in and around this area of the artery wall. It is revealed that other sections of the artery wall are in an expanded and in stretched state, and inflammatory cells are present in some places. It was noticed that the part of the clot formed in the intermediate A2 of the middle artery, adhering to the artery wall, consists of dense lymphoid cells and forms a crescent infiltrate. The rest of the clot consists of a coarse fibrin protein. It is revealed that the endothelial cells of the artery wall are relatively hypertrophied, prone to hyperchromasia, and lymphocytes adhere to the surface of some of them. It is observed that the fibrous structures of the middle and outer adventitious layers of the artery wall undergo fibrous outflow. It turns out that hemorrhages have formed in the brain tissue around this artery.
 | Figure 1. The initial part A1 of the middle cerebral artery contains a fibrin, lymphoid-cell thrombus in the cavity, the artery is dilated, the wall is thinned. Staining: G-E. Magnification: 10x40 |
 | Figure 2. The part A3 of the middle cerebral artery inside the brain tissue, the arteriole cavity is obstructed by an erythrocyte thrombus. Staining: G-E. Magnification: 10x40 |
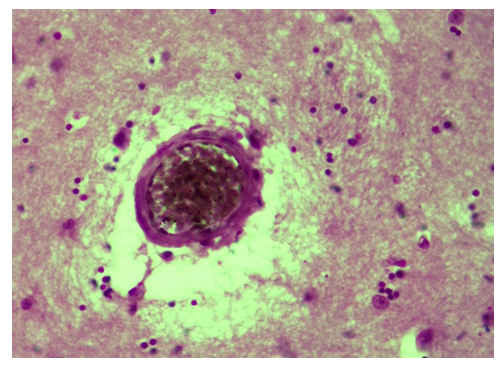
 | Figure 3. A fragment of Figure 5, in the center of which is an infarction, fibrin thrombosis of the surrounding blood vessels. Staining: G-E. Magnification: 10x40 |
4. Conclusions
- In COVID-19, the cerebral hemisphere with the basin of the middle cerebral artery, forehead, upper and cheek fragments, there was a focus of ischemia of different sizes on the lateral surface, more in the right hemisphere (57.1%), the rest in the left hemisphere (42.9%).The thrombus that arose in the initial part A1 of the middle cerebral artery passing between the brain fragments is mainly fibrin. It was found that lymphoid cells are present in its peripheral areas, one surface of the thrombus adheres to the artery wall, a proliferative infiltrate of lymphoid and histiocytic cells forms in this area of the artery wall and around it.The focus of cerebral tissue infarction, which developed as a result of coronavirus, differs from atherosclerotic infarction. The following features were noted in coronavirus: almost all blood vessels around the ischemic focus are affected by endotheliitis, microangiopathy, that fibrin, lymphocytic, erythrocytic thrombi have formed in the cavity of almost all of them, cerebral thrombi have formed in the center of the ischemic focus and has necrosis, encephalomalacia, and transformation into a single structureless formation.It was found that during the second phase of COVID-19 proliferation, the endothelium of the blood vessel wall containing a cellular infiltrate that developed around the ischemic infarction of brain tissue, proliferated pericyte cells, which led to large-scale infiltration of lymphoid and histiocytic cells in and around the artery wall.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML