Nurkhanova Nilufar Odilovna
Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Nurkhanova Nilufar Odilovna, Bukhara State Medical Institute, Bukhara, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Currently, proliferative diseases of the endometrium are a known background for the development of endometrial cancer. In this regard, improving diagnostics, studying additional risk factors and predictors of endometrial hyperplasia, as well as methods for preventing this disease are important aspects of the prevention of cancer. This article presents our own results of the research.
Keywords:
Perimenopause, Endometrial hyperplasia, Obesity, Vitamin D
Cite this paper: Nurkhanova Nilufar Odilovna, Vitamin D Level and Metabolic Disorders in Patients with Endometrial Hyperplasia in the Perimenopausal Period, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1365-1368. doi: 10.5923/j.ajmms.20241405.47.
1. Introduction
Enometrial hyperplasia is the most pressing problem in the structure of gynecological diseases due to the high probability of recurrence, as well as the risk of degeneration into a malignant neoplasm, in the absence of control and management of the patient [1,5,8,11]. Recently, it has been proven that vitamin D has antiproliferative activity and plays a role in the differentiation of various cell types [4,6,12]. Metabolic syndrome, which often accompanies obesity, also contributes to the increase in the number of proliferative processes in the endometrium [1,2,11]. According to recent studies, hypertension and type 2 diabetes mellitus (DM) are independent risk factors for proliferative endometrial diseases [3,7,10]. Currently, the data available in the literature on vitamin D status in proliferative diseases of the female genital organs are scarce and contradictory [4,9,12]. Therefore, it is relevant to study additional risk factors that can cause the malignancy of GPE.Purpose of the study. To assess vitamin D levels and metabolic disorders in patients with endometrial hyperplasia in the perimenopausal period.
2. Materials and Methods of Research
This study involved 114 women in the perimenopausal period, of which three groups were formulated: group I consisted of 36 women with a physiological course of the perimenopausal period, group II included 40 women with GE, group III included 38 patients with recurrent GE with transition to PGE. The studies were carried out in antenatal clinics in the city of Bukhara and the gynecological department of the BFRNCEMP in the period from 2022 to 2023. All patients gave written informed consent to the use of their data for research purposes. AUB was defined by the presence of bleeding from the uterine body that was abnormal in volume, regularity, and/or timing, as reported by women. We excluded women with menopausal status (absence of menstruation for at least 12 months after age 40), bleeding in the perimenopausal period with a diagnosis of malignant oncological processes of the genitals, trauma to the female reproductive system, as well as acute infectious diseases of the gastrointestinal tract. The following characteristics of patients were taken into account: age (years), age at menarche (years), parity, body mass index (BMI=weight (kg)/height (m)), presence of arterial hypertension or diabetes, obesity, menstrual cycle phase, presence breast cancer families, current hormonal therapy (progestogen only, combined oral contraceptives and vaginal ring), smoking habit, endometrial thickness (mm), infertility, duration of AUB. All statistical analyzes were performed using Statistica statistical software, using the Fisher-Student method.
3. Research Results
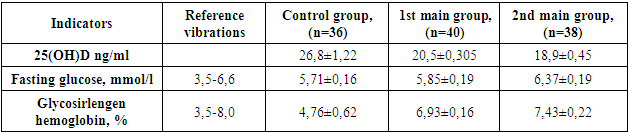
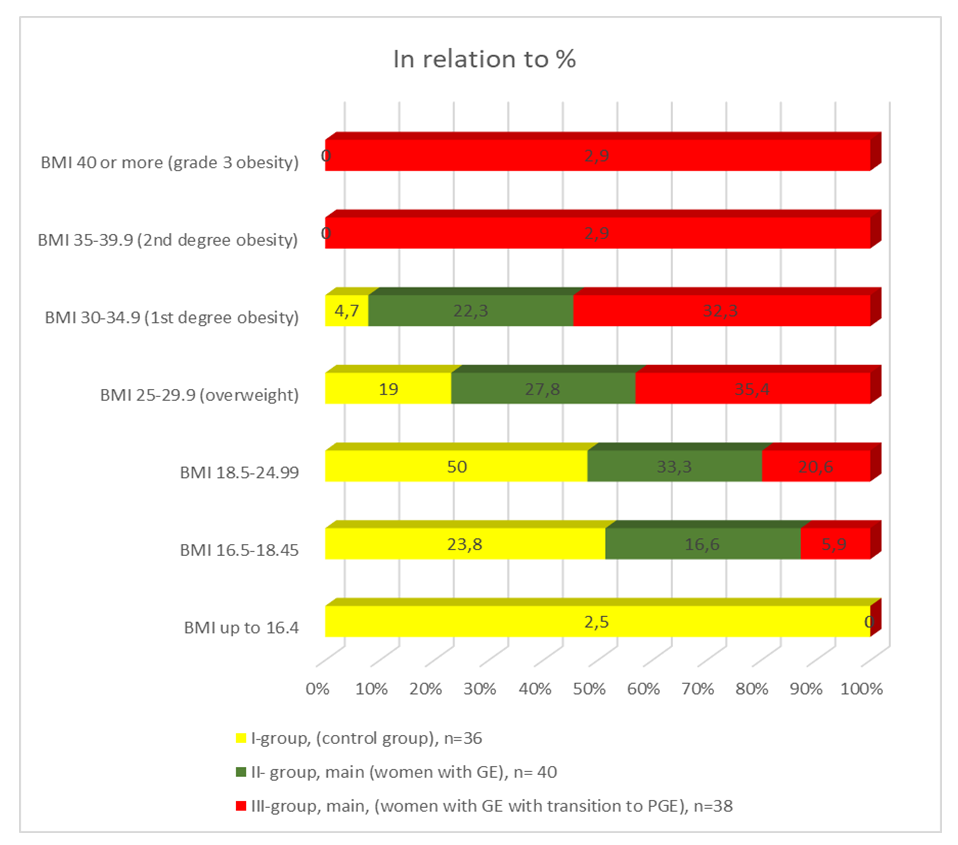
It should be noted that the age of the women in the groups ranged from 45 to 55 years and averaged ±50 years, in the main group from ±48.05 years, in the control group ±49.2 years (p> 0.05). Based on these data, we can say that there is no significant difference between the ages of those examined in the control and main groups. The control group included patients of the same age but without a history of AUB. As a result of examining women in the selected groups, we found that the nature of menstrual function in both groups did not differ significantly. The average age of menarche in the main group was ±14.0 and ±14.5 years, in the control group ±13.2 years (p> 0.05). The duration of the menstrual cycle ranged from 25 to 32 days, on average it was 28-30 days in the main group, 26-27 days in the control group (>0.05). The duration of bleeding did not have significant differences in the groups - 8.2±0.5 and 8.6±0.6 days, and blood loss in all was assessed as significantly heavy.We know from many recent sources that BMI (body mass index) directly affects the course of many diseases, including proliferative endometrial diseases, since obesity leads to unbalanced estrogen stimulation of endometrial cells, which is why we included this criterion in our study. All data is shown in Figure 1. 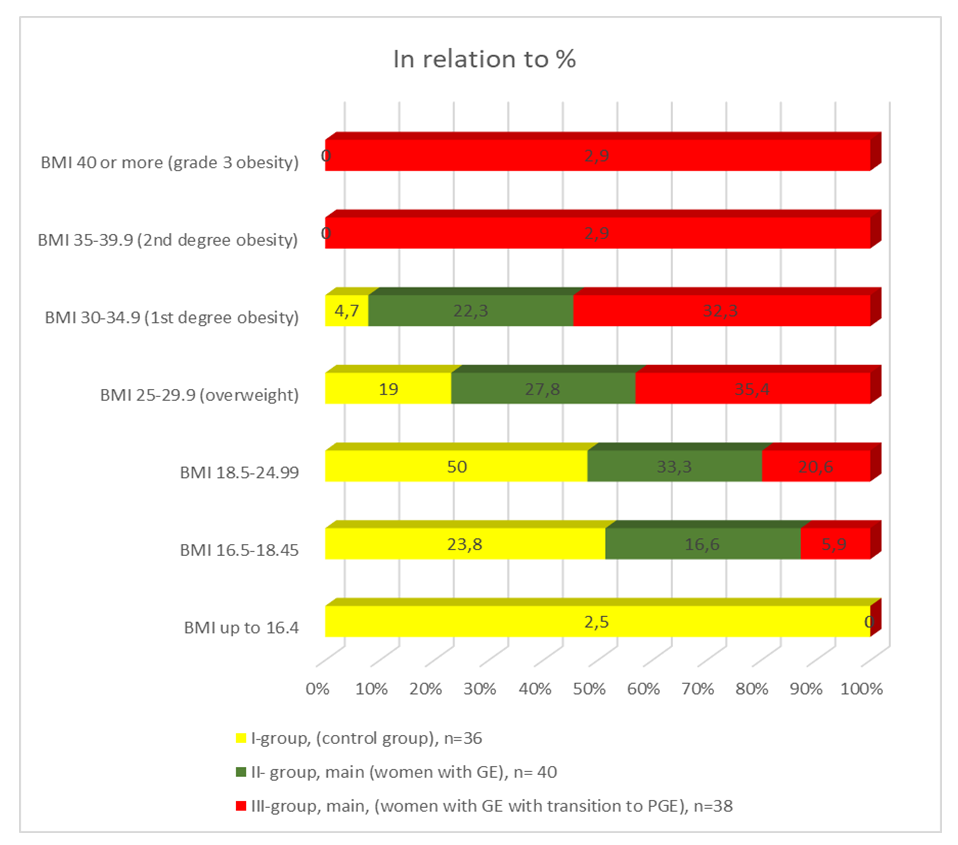 | Figure 1. Comparative BMI indicators by group |
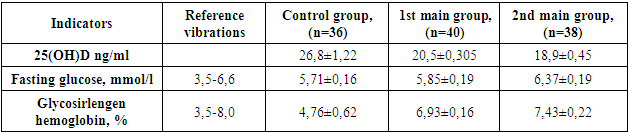
Following the data in the figure, it can be argued that in the two main groups of patients with overweight and obesity there are significantly more patients than in the control group; this criterion can also be considered a risk factor for perimenopausal AUB.In the next stage of our study, we checked in overweight women with OA heredity, where the patients indicated a history of diabetes in their first-degree parents, fasting blood glucose levels and if there were suspicious fluctuations above normal (6.5 mmol/ l) glycated hemoglobin was prescribed to determine the duration of carbohydrate metabolism disorders, and we had 4.76 ± 0.62 such patients in the control group, 6.93 ± 0.16 and 7.43 ± 0.22 in the two main groups, respectively. We decided to check fasting glucose in all women in order to avoid missing any disorders of carbohydrate metabolism in women of perimenopausal age. The data is shown in Table 1.Table 1. Comparative data of specific markers in patients with HPE and healthy women of perimenopausal age
 |
| |
|
For relatively high or high fasting glucose levels, we tested glycosylated hemoglobin, or glycohemoglobin (HbA1c), a biochemical blood marker that reflects the average blood sugar level over a long period (three to four months), as opposed to measuring blood glucose, which gives an idea of the blood glucose level only at the time of the study. Our main goal was to evaluate the diagnostic sensitivity and specificity of glycohemoglobin (HbA1c) determination using direct immunoturbidimetry as a test for identifying cases of diabetes mellitus.In our studies, 4 patients (11.1%) and of them 2 in the control group, in the second group 16 patients (40%) had grade 2 anemia, grade 3 accounted for 7 (15%) ) women with GPE, and in the third group it was diagnosed in 9 (22.5%), 1st degree, 17 (42.5%) 2nd degree, 14 (35.0%) 3rd degree, respectively. In cases where patients with HPE had mild anemia, HbA1c results did not decrease. In case of 1st degree anemia, the diagnostic effectiveness of determining HbA1c in patients with HPE did not change when using the immunoturbidimetric method. In general, in our patients with HPE it averaged 7.2, 3± and 7.0, while in healthy women it varied within 5.4±0.11 and still did not go beyond the normal reference values (3, 5-8.0%).High HbA1c values compared to healthy women were observed in only 18 patients (16.0%), who had severe degrees of anemia with concomitant somatic pathologies such as obesity and high BMI. Clinically, these patients felt dry mouth, frequent urge to urinate, and a tendency to periodic colds, especially in the cold season. We were also able to promptly prescribe to our patients an appropriate strict diet and monitoring for 6 months or more. There were 2 negative cases when patients with HPE did not follow a strict diet of glycohemoglobin and vitamin D3 and changed in the opposite way, the first increased, and the second decreased. From this we can conclude that the indicators of glycohemoglobin and vitamin D3 are oppositely correlated with each other. There is evidence in the literature that many dishormonal processes depend on the concentration of cholecalciferol, vitamin D, in the body, in particular, with hyperplastic processes of the endometrium, the risk of developing endometrial cancer, especially during the perimenopausal period, and even with relapses of various forms of hyperplasia increases several times. As is already known, with the existing metabolic syndrome, when there is varying degrees of obesity, glucose tolerance or insulin resistance of the body begins to form, especially in the perimenopausal age, when hormonal changes occur to varying degrees and one of the preventive measures, in our opinion, is the timely determination of vitamin D3 levels, glucose on an empty stomach, and if any abnormalities are detected, it is normal or hemoglobin. The purpose of our study was to determine, in a comparative aspect, the vitamin D content in both patients with HPE and healthy controls. The problem is that adding vitamin D deficiency to the diet will not always reduce blood sugar. Studies by Indian scientists have proven over a 6-month period of studying patients with diabetes or prediabetes that long-term addition of Dz to the diet in a dose of at least 5000 IU leads to normalization of hyperglycemia, but with normal blood pressure and normocoagulation values. Based on these considerations, we recommended that women with HPE check the concentration of vitamin D3 in the blood; in the second group it was found to be 20.5 ± 0.305 ng/ml, in the third group 18.9 ± 0.45 ng/ml, while in healthy people it was 26.8 ±1.22, it is 6.7 or 7.3 reliably lower. Reference values for cholecalciferol levels ranged from 21.9 to 54.6 ng/ml. This means that healthy women without HPE also had lower levels than in the general population. For example, out of 36 healthy women, 7 had low levels of Vitamin D3, these were healthy overweight women and their levels ranged from 15.8-21.9 ng/ml.Based on this, it should be emphasized that not only patients with HPE may have low levels of cholecalciferol, and therefore all women of perimenopausal age, especially those with HPE, should have their Vitamin D levels checked to avoid missing possible prediabetic conditions.Vitamin D and fasting blood glucose levels showed a significant negative correlation with each other, meaning that they are oppositely correlated. We also established a relationship between the color index (which varied between 0.8-1.0 without anemia) and the level of vitamin D3 were multidirectionally dependent on each other - and with severe hypochromic anemia, the vitamin D3 index sharply decreased. A decrease in this indicator is also observed in iron deficiency and chronic diseases of organs and systems. Lower concentrations of vitamin D3 were observed in patients with HPE with relatively high levels of glucose and glycosylated hemoglobin.There is information in the literature that women tolerate the prescription of a double dose from the moment a vitamin deficiency is detected in doses of 4000-5000 IU, sometimes even up to 10,000 IU, without any side effects. Thus, a lower level of vitamin D is associated with reduced sensitivity to insulin and can subsequently lead to the development of a number of complications in patients with HPE, such as diabetes, deterioration in quality of life, instability of the nervous system, an increase in menopausal symptoms (hot flashes, etc.).In our opinion, it is the initial deficiency of vitamin D in HPE, which was observed in our patients, that can aggravate the disturbance of blood microcirculation or contribute to its further disturbance against the background of already formed hypercoagulation. And if all these changes occur against the background of hypertensive disorders, irreversible processes throughout the body are accelerated and possible expected complications of various kinds increase several times.It is known that vitamin D stimulates the expression of insulin receptors; therefore, vitamin D deficiency, in turn, may be associated with insulin resistance. Our timely prescription of vitamin D to patients with GPE was intended to achieve better glycemic control, and this vitamin can also be used as an appropriate prevention of progressive complications associated with high blood sugar levels.
4. Conclusions
Thus, HPE in perimenopausal women is a multifactorial disease. Diagnosis of the true condition of the woman herself is based on reliable diagnostic tests for GPE to determine the presence of any carbohydrate disorders: glycohemoglobin and fasting glucose levels. We also recommend that patients with various hormonal disorders at any age, and especially in perimenopausal age, determine the level of cholecalciferol before prescribing even prophylactic doses of this vitamin. Timely inclusion of these diagnostic markers will help reduce the expected complications of HPE and subsequent possible complications.Forming risk groups for the development of HPE, which will include women with excess weight (obesity), metabolic syndrome, with OAA, OGA, OSA, or those with a history of ID deficiency, can serve as a prerequisite for the timely stop of carbohydrate metabolism disorders and the development of pathological dyshormonal disorders.
References
| [1] | Dubrovina S.O. Pathogenetic aspects of hyperplastic processes in the endometrium in women with metabolic syndrome / S.O. Dubrovina, N.H. Skachkov, Yu.D. Berlim et al. // Ross, Vestn. obstetrician-gynecologist. 2008. - No. 3. - P. 41-44. |
| [2] | Bochkareva N.V., Kondakova I.V., Kolomiets L.A., Chernyshova A.L. The role of insulin-like growth factors and their binding proteins in the pathogenesis and prognosis of endometrial cancer // Russian Journal of Oncology, No. 3. - 2009. - P. 46-50. |
| [3] | Davydov A.I. Atypical endometrial hyperplasia: issues of morphogenesis, classification, diagnosis and treatment / A.I. Davydov, O.V. Kryzhanovskaya // Issue. gin., obstetrics and perinatol. 2009. - T. 8, No. 3 - P. 93-96. |
| [4] | Zaripova D.Ya., Tuksanova D.I., Negmatullaeva M.N. Features of the perimenopausal transition in obese women. News of dermatovenerology and reproductive health. No. 1-2.2020 pp. 39-42. |
| [5] | Ismailova Z.I. Early diagnosis and prevention of endometrial hyperplastic processes: scientific publication / Z. I. Ismailova // News of dermatovenerology and reproductive health. - Tashkent, 2013. - N3- - P. 127-128. |
| [6] | Kurman RJ, Kaminski PF, Norris HJ. The behavior of endometrial hyperplasia. A long-term study of “untreated” hyperplasia in 170 patients. Cancer. 2015; 56: 403–12. [PubMed] [Google Scholar] |
| [7] | Nurkhanova N.O. Assessment of the risk of endometrial hyperplasia in the perimenopausal period. / International Journal of Advanced Research in Engineering and Applied Sciences, 2022. Vol. 11. No. 6. R. 8-15. https://garph.co.uk/IJAREAS/June2022/2.pdf. |
| [8] | Tavassoli FA. World Health Organization Classification of Tumors: Pathology and Genetics of Tumors of the Breast and Female Genital Organs. Lyon: IARC Press; 2013. [Google Scholar] |
| [9] | Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlander MJ, Horner MJ, et al. Finding Cancer Statistics. Cancer Stat Fact Sheets, Cancer of the Corpus and Uterus, NOS. National Cancer Institute; Bethesda, MD: 2008. pp. 3–31–0008. http://seer.cancer.gov/statfacts/html/corp.html. [Google Scholar] |
| [10] | Shapiro AG. Emergency treatment of menstrual disorders in a nonpregnant woman. Emerg Med Clin North Am. 2017; 5: 559–68. [PubMed] [Google Scholar] |
| [11] | Prip C.M., Stentebjerg M., Bennetsen M.H., Petersen L.K., Bor P. Risk of atypical hyperplasia and endometrial carcinoma after initial diagnosis of non-atypical endometrial hyperplasia: A long-term follow-up study // PLoS ONE. – 2022. – Vol. 17(4). – Art. ID: e0266339. https://doi.org/10.1371/journal.pone.0266339. |
| [12] | Henn M., Martin-Gorgojo V., Martin-Moreno J.M. Vitamin D in cancer prevention: Gaps in current knowledge and room for hope // Nutrients. 2022. Vol. 14, N 21. P. 4512. DOI: https://doi.org/10.3390/nu14214512. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML