-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1325-1327
doi:10.5923/j.ajmms.20241405.37
Received: Apr. 18, 2024; Accepted: May 15, 2024; Published: May 18, 2024

Dynamics of Myocardial Markers During Intradialysis Physical Load in Patients with Chronic Kidney Disease
G. B. Kasimova , Sh. K. Muminov
Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

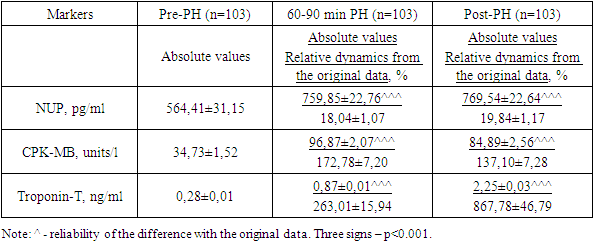
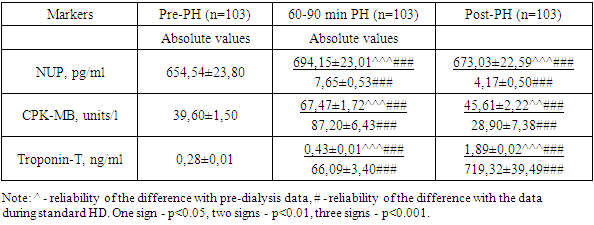
Aim of the study: to study the effect of intradialytic physical activity on myocardial markers in patients with chronic kidney disease. Material and research methods. The study included 103 patients with CKD5d aged 18 to 65 years. In all patients, natriuretic peptide (NUP), myocardial fraction of creatine phosphokinase (CPK-MB), myocardial fraction of troponin (troponin T) were determined in the blood of all patients before the hemodialysis (HD) procedure, at 60-90 minutes of HD and after cessation of HD. The physical activity used was bicycle ergometry (BE) for 30 minutes during the first hour of HD. Results: During the HD procedure, by the 60-90th minute of the procedure, there was a significant increase in the concentration of NUP - by 18.04%, CPK-MB - by 172.78%, and troponin T - by 263.01% Intradialytic physical exercise (PhE) contributes to a significant a decrease in the rate of increase in the concentration of myocardial markers (for NUP: +7.66% versus +18.04%, for CPK-MB: 87.2% versus +172.8% and for troponin T: +66.09% versus +263%, p<0.001 for all three indicators). Conclusion. During the HD procedure, a significant increase in the concentration of markers of myocardial “suffering” is noted. Intradialytic physical exercise helps to reduce these markers of myocardial damage in the blood compared to standard HD and may have a preventive effect on cardiomyocytes.
Keywords: Chronic kidney disease, Hemodialysis, Natriuretic peptide, Creatine phosphokinase, Troponin T, Intradialytic bicycle ergometry
Cite this paper: G. B. Kasimova , Sh. K. Muminov , Dynamics of Myocardial Markers During Intradialysis Physical Load in Patients with Chronic Kidney Disease, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1325-1327. doi: 10.5923/j.ajmms.20241405.37.
Article Outline
1. Introduction
- Hemodialysis (HD) is critical for the survival of patients with CKD. However, each HD session is accompanied by significant sharp hemodynamic and metabolic changes. The circulating blood volume (CBV) decreases significantly, which causes impaired perfusion of organs and tissues, including the myocardium [1,2]. A decrease in blood volume has two main negative effects on the myocardium: a decrease in pressure in the coronary vascular system leads to the development of intradialytic myocardial ischemia, and a decrease in preload is associated with non-ischemic myocardial dysfunction [3,4]. A decrease in systolic blood pressure and ultrafiltration are associated with the development of local myocardial dyskinesis, indicating myocardial stunning [5,6].Dynamic physical activity can help strengthen the body's adaptive abilities and normalize reflex regulatory pathways. The literature provides evidence of the positive effect of intradialytic exercise on quality of life and intradialytic hypotension [7,8].Purpose of the study: to study the effect of intradialytic physical activity on myocardial markers in patients with chronic kidney disease.
2. Material and Research Methods
- The study included 103 patients with CKD5d aged 18 to 65 years. The average HD experience is 8.45±0.57 months. When included in the study, natriuretic peptide (NUP), myocardial fraction of creatine phosphokinase (CPK-MB), myocardial fraction of troponin (troponin T) were determined in the blood of all patients before the hemodialysis procedure, at 60-90 minutes of HD and after cessation of HD. The control group consisted of 20 healthy individuals of the appropriate age.The load used was bicycle ergometry (BE) on an exercise bike, which allows BE to be carried out in foot and hand modes. A low-intensity load was used - without resistance, for 30 minutes during the first hour of HD with the patient lying down or semi-sitting.
3. Research Results and Discussion
- During the HD procedure, by the 60-90th minute of the procedure, a significant increase in the concentration of myocardial markers “suffering” was noted: thus, the concentration of NUP increased by 18.04%, CPK-MB – by 172.78%, and troponin T – by 263.01% (Table 1). An increase in the concentration of NUP is probably associated with a change in loading conditions - a decrease in BCC during HD, a decrease in preload on the myocardium, while an increase in the concentration of both markers of necrosis indicates cell damage, which can be caused by metabolic turbulence and mitochondrial energy deficiency with damage to integrity membranes, and myocardial ischemia due to a decrease in coronary blood flow with a decrease in blood volume and stimulation of coronary vasospasm [11,12]. By the end of the HD procedure, the NUP concentration remained at the level of the middle of the HD (with initial dynamics data of +19.84%), reflecting the persistence of hemodynamic shifts. The concentration of CPK-MB decreased relative to the values achieved during HD, but did not reach the initial values (the dynamics with the initial data was 137.10%), and the concentration of troponin T continued to increase to 867.78% of the initial value. Such multidirectional changes reflect patterns characteristic of markers: CPK-MB is the “fastest” marker, the concentration of which increases from the first minutes of ischemia and also quickly decreases, while the concentration of troponin T increases somewhat delayed and the peak concentration occurs later. Thus, intradialytic dynamics of markers of myocardial condition reflects changes in hemodynamic load and necrosis of cardiomyocytes during the procedure.
|
|
4. Conclusions
- In conclusion, during the HD procedure, a significant increase in the concentration of markers of myocardial “suffering” is observed. Intradialytic physical exercise helps to reduce markers of myocardial damage in the blood compared to standard HD and may have a preventive effect on cardiomyocytes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML