-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1321-1324
doi:10.5923/j.ajmms.20241405.36
Received: Apr. 27, 2024; Accepted: May 16, 2024; Published: May 18, 2024

Breast Cancer and the Condition of the Liver
Turaev Umar Rakhimovich
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Turaev Umar Rakhimovich, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chemotherapy is one of the main methods for destroying tumor cells in cancerous diseases. However, there is little information about the effect of this method on healthy cells. In particular, there is a lack of products affecting liver function. Our study is dedicated to the adverse effects of chemotherapy on liver function and their prevention. In the pathogenesis of breast cancer development, a special role is attributed to chronic liver dysfunction caused by viral infection.
Keywords: Breast cancer, Chemotherapy, Metastases, Morphological and biochemical changes in the liver
Cite this paper: Turaev Umar Rakhimovich, Breast Cancer and the Condition of the Liver, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1321-1324. doi: 10.5923/j.ajmms.20241405.36.
Article Outline
1. Introduction
- Breast cancer has an aggressive course, characterized by invasive, very rapid growth, and metastasis. The formation can arise from breast cells or be a metastasis of another (primary) tumor. Metastases in neoplasms most commonly develop from breast cancer. This is associated with the nature of blood circulation, hormone dependence, and the lymphatic function of the breast. Metastases of malignant neoplasms are a severe complication, more dangerous than the primary tumor itself. Metastatic cancer is identified as metastases of a malignant tumor during its primary localization in other organs. The causes and mechanisms of breast cancer (BC) development are still not fully understood. The influence of geographical location, climate, diet, and certain medications has been studied. The tumor and metastatic cells in different fragments are highly heterogeneous formations, with all cells being different, rapidly dividing, and mutating quickly. However, chemotherapy affects all metastases regardless of their location. The exception is metastases in the brain, where not all drugs penetrate. In these cases, special treatment is prescribed, either through special administration of drugs into the spinal canal. There are even tumors where the primary focus cannot be found - meaning that all we see in the body are metastases. Nevertheless, treatment is still prescribed, and in many cases, it is successfully carried out.
2. Materials and Methods
- Chemotherapy is a treatment. And like any treatment, it has side effects. They can occur with any medication, they can occur after surgical procedures. Chemotherapy itself also varies depending on the goal. The main mechanism of action of chemotherapeutic agents is to interfere with the cell division mechanism. Cancer cells divide very rapidly, so by affecting cell division, we stop tumor growth.Preoperative chemotherapy is used before surgical operation to minimize the size of the tumor and make the surgical intervention as sparing as possible. There are also palliative and postoperative chemotherapy. Palliative chemotherapy is used when the tumor is advanced, with multiple metastases, and curing the patient is impossible, but slowing down further progression and attempting to control the tumor are possible. In this case, chemotherapy aims to give the patient time, but typically it accompanies them until the end.After chemotherapy, it is expected that the patient's blood counts will drop. Typically, the peak drop occurs on the seventh to fourteenth day because the chemotherapy has just affected all the cells that were in the peripheral blood, and the bone marrow hasn't had time to produce new ones yet. The drop occurs depending on the drug used; some primarily affect platelets, others affect leukocytes and neutrophils, while others affect red blood cells and hemoglobin.Chemotherapeutic treatment occurs in cycles. Depending on the chemotherapy regimen, a person may receive, for example, three days of chemotherapy infusions, and the next ones will be in 21 days. This interval is called "one cycle," it is given specifically for the patient's body to recover. Before each new chemotherapy session, the patient's condition is monitored, observing what happened to them during this interval - clinical and biochemical blood analyses are performed.Until a person has recovered, a new cycle of treatment does not begin. If besides a decrease in blood counts to a certain level during the interval between "chemos," nothing bad happened — the blood will recover on its own. Excessive reduction in platelets poses a risk of bleeding, so patients with such indicators are given platelet transfusions.If leukocytes, responsible for immunity, have decreased, and a person has contracted an infection, started coughing, sneezing, or developed a fever, antibiotics are immediately prescribed to prevent the infection from spreading. Usually, all these procedures are done on an outpatient basis. Before the very first cycle of chemotherapy, the patient should be explained all possible complications, told about each drug and its effects; and the patient can consult with their oncologist. Weighing the risks is the starting point of chemotherapy.The doctor and the patient weigh between the damage that chemotherapy can cause and the benefit that may follow it - namely, extending life sometimes by decades. Before each new chemotherapy session, the patient's condition is monitored, observing what happened to them during this interval - clinical and biochemical blood analyses are performed. Until a person has recovered, a new cycle of treatment does not begin. If besides a decrease in blood counts to a certain level during the interval between "chemos," nothing bad happened — the blood will recover on its own.Excessive decrease in platelets poses a risk of bleeding; patients with such indicators are given platelet transfusions. If leukocytes, responsible for immunity, have decreased, and a person has contracted an infection, started coughing, sneezing, or developed a fever, antibiotics are immediately prescribed to prevent the infection from spreading. Usually, all these procedures are done on an outpatient basis.During the breaks between chemotherapy courses, the patient is monitored by an oncologist from the district oncology dispensary or polyclinic. This is a key moment in deciding on the necessity of using chemotherapeutic agents: if we understand that the success rate of prescribing a particular medication will be lower than the side effects, there is simply no point in using it.After chemotherapy, it is expected that the patient's blood counts will drop. Typically, the peak drop occurs between the seventh and fourteenth day because the chemotherapy has just affected all the cells that were in the peripheral blood, and the bone marrow hasn't had time to produce new ones yet. The drop occurs depending on the drug used; some primarily affect platelets, others affect leukocytes and neutrophils, while others affect red blood cells and hemoglobin.After chemotherapy, it is expected that the patient's blood counts will drop. Typically, the peak drop occurs between the seventh and fourteenth day because the chemotherapy has just affected all the cells that were in the peripheral blood, and the bone marrow hasn't had time to produce new ones yet. The drop occurs depending on the drug used; some primarily affect platelets, others affect leukocytes and neutrophils, while others affect red blood cells and hemoglobin.If, besides a decrease in blood counts to a certain level during the interval between "chemos," nothing bad happened — the blood will recover on its own. Excessive reduction in platelets poses a risk of bleeding; patients with such indicators are given platelet transfusions. If leukocytes, responsible for immunity, have decreased, and a person has contracted an infection, started coughing, sneezing, or developed a fever, antibiotics are immediately prescribed to prevent the infection from spreading. Usually, all these procedures are done on an outpatient basis.In the intervals between chemotherapy courses, the patient is supervised by an oncologist from the district oncology dispensary or polyclinic. Before the very first cycle of chemotherapy, the patient must be informed about all possible complications, told about each drug and its effects, and the patient may consult with their oncologist.Risk assessment is the starting point of chemotherapy. The doctor and the patient choose between the damage that chemotherapy may cause and the benefit that may follow it - namely, extending life sometimes by decades. This is a key moment in deciding the necessity of using chemotherapy drugs: if we understand that the success rate of prescribing a particular drug will be lower than the side effects, there is simply no point in using it. The reasons for the occurrence of metastases in different tumors are very different, and we still do not know exactly how metastases occur. The only thing we know is that there are no "cancer stem cells. The tumor in its various fragments and metastatic cells is a very heterogeneous formation; all the cells there are different, they divide rapidly, and mutate quickly. But in any case, chemotherapy affects all metastases, wherever they may be. The exception is metastases in the brain, where not all drugs can penetrate. In these cases, special treatment is prescribed, or special administration of drugs - into the spinal canal. There are even tumors for which a primary focus cannot be found - meaning, all we see in the body are metastases. However, treatment is still prescribed, and in many cases, it is successfully carried out. "Alternative remedies" taken by oncology patients, at best, turn out to be harmless herbs with no noticeable effect. Unfortunately, it can be worse. For example, sometimes patients start taking miraculous medicines based on a mixture of different oils, but oil is a very heavy product for the liver. As a result, the patient literally induces liver inflammation, and we cannot start the chemotherapy cycle because "chemo" also affects the liver. And it's good if the patient at least tells us what they have been taking, and we can understand what worsened the situation. But in the end, the treatment is postponed, its effectiveness is reduced. In addition, a number of new drugs for treating, for example, breast cancer, are now based on plant component.Recently, in addition to cytostatic chemotherapy drugs that acted on the entire body, new drugs have emerged. This is a new generation of chemotherapy drugs - targeted drugs and drugs based on a fundamentally different principle of action - immunotherapy drugs. A targeted drug is a medicine that acts not on the entire body but specifically on tumor cells. Importantly, molecules of a specific targeted drug can only attach to receptors of cells of a certain type of tumor.The specific subtype of the tumor is determined by genetic analysis during molecular-genetic research. Immunotherapy drugs affect the immune system of the body and the immune mechanisms of the tumor at its core. As a result, the body's own immunity is activated, which begins to fight against cancer cells. One of the methods is hormone therapy, but here the circle of indications is narrower - the tumor must be hormone-sensitive. Hormone therapy works best for breast and prostate tumors, although hormones can only be used under certain indications even in these cases.But in any case, chemotherapy affects all metastases, wherever they may be. The exception is metastases in the brain, where not all drugs can penetrate. In these cases, special treatment is prescribed, or special administration of drugs - into the spinal canal. There are even tumors for which a primary focus cannot be found - meaning, all we see in the body are metastases. However, treatment is still prescribed, and in many cases, it is successfully carried out.However, for a patient to receive an immunotherapy drug and a targeted drug, the tumor must have specific characteristics; these drugs act not on all tumors but on their specific mutations. The pathologist and molecular geneticist must detail the tumor's profile and specify in the prescription that the patient needs this particular drug. In experimental conditions in the vivarium, we conducted an experiment. Here, for the first time, we used pomegranate oil as both an immunostimulant, antioxidant, and anti-tumor agent.
3. In the Experiment
- • Induction of breast cancer in rats using 7,12-dimethylbenzanthracene in ribade tea and studying the morphology of the mammary gland;• Scientific assessment of the structural and general morphological structure after 10 days of chemotherapy;• Determination of morphological changes in the livers of white rats with the addition of immunocorrection with timalin to traditional (standard) treatment after chemotherapy;• Determination of morphological changes in the livers of white rats after chemotherapy only with pomegranate seed oil correction.
4. Research Object
- As research subjects, 26 white mongrel female rats were used under standard vivarium conditions for 6 months. In accordance with the research objective, all experimental animals were divided into 4 comparable groups: a control group and 3 experimental groups called breast cancer. Research Object. As research subjects, 26 white mongrel female rats were used under standard vivarium conditions for 6 months.
5. Scientific Novelty of the Research
- • Study the morphogenesis of breast cancer;• Study the structural-morphological changes in the liver with breast cancer in rats;• For comparative study of liver morphogenesis during chemotherapy, information on the regularities of liver structure and features of rat liver components was obtained;• Morphofunctional changes in liver damage under the influence of chemotherapy were studied in the experiment.• Morphofunctional characteristics of the influence of traditional conservative treatment after chemotherapy on liver structure parameters were studied and evaluated.• Comparative characteristics of thymalin and pomegranate oil were studied. On the 21st day, all experimental animals were divided into 6 groups: 1- Control group; 2- Experimental group BC (breast cancer); 3- Experimental group BC + Pantaxil + Thymalin; 4- Experimental group BC + Pantaxil + pomegranate oil.
6. Results
- Group 1: Liver tissue in intact animals appears greenish-blue, and the vessels have a dark shade. In the liver tissue, the triad of liver vessels is well visible. The sinusoids are smooth-walled, often branching cylindrical tubes, with blood flow velocity varying significantly within them.Group 2: Breast Cancer (BC). In experimental animals, the liver appears congested and purplish-red. Upon biomicroscopy, liver enlargement and phenomena of blood congestion are observed, characteristic of venous stasis with vasodilation. Liver venules become engorged. Additionally, there are occasional depleted sinusoids, which alternate with dilated, blood-filled capillaries. Blood flow is slowed. Pre-sinusoidal edema is noted. This phenomenon is particularly pronounced in the center of lobules, which are characterized microscopically by blurred vessel boundaries. Central collecting venules are dilated, blood flow within them is slowed, and aggregation of blood formed elements is observed.
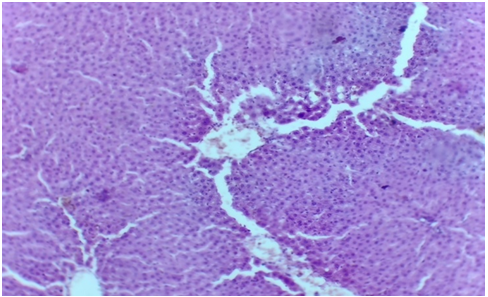 Group 3: BC + Pantaxel + Thymalin. Liver congestion with venous stasis and vasodilation is slightly reduced, and blood flow is slightly accelerated. Perivascular edema is still present. Aggregation of blood formed elements is preserved.Group 4: BC + Pantaxel + pomegranate oil. The liver is morphometrically reduced in size, and perivascular edema is reduced. Depleted sinusoids are filled, and blood flow is noticeably accelerated.
Group 3: BC + Pantaxel + Thymalin. Liver congestion with venous stasis and vasodilation is slightly reduced, and blood flow is slightly accelerated. Perivascular edema is still present. Aggregation of blood formed elements is preserved.Group 4: BC + Pantaxel + pomegranate oil. The liver is morphometrically reduced in size, and perivascular edema is reduced. Depleted sinusoids are filled, and blood flow is noticeably accelerated.7. Conclusions
- (Pomegranate oil has been used in folk medicine for over 1000 years. According to literary data, it is considered an effective immunostimulant, antioxidant, and anti-tumor agent. Initially, it was extracted from a special variety of pomegranate in Yemen). The improvement in the condition and indicators of the experimental animals is visibly evident. Pomegranate oil triggers the mechanism of self-destruction of cancer cells, inhibiting the growth of new formations and breast tumors. We propose that alongside traditional chemotherapy methods, folk remedies such as pomegranate oil be widely used.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML