-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1317-1320
doi:10.5923/j.ajmms.20241405.35
Received: Apr. 19, 2024; Accepted: May 13, 2024; Published: May 18, 2024

Surgical Treatment of Degenerative Diseases of the Cervical Spine
Yuldashev Ravshan Muslimovich, Shukurov Xumoyuddin Asliddin O’g’li, Ruzimurodov Muhammad Faxritdinovich
Republican Scientific Center of Neurosurgery under the Ministry of Health of the Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background. This article offers an analysis of the various techniques employed in the surgical treatment of cervical spine degenerative diseases. Methods. The results of examination and surgical treatment of 76 patients for the period 2022-2023 at the Republican Scientific Center of Neurosurgery under the Ministry of Health of the Republic of Uzbekistan with degenerative diseases of the cervical spine were analyzed. Of these, 29 were women and 46 were men. The average age of the patients was 53.8 years (range: 28-83 years). All patients underwent a comprehensive neurological examination and instrumental examination (magnetic resonance imaging of the cervical spine, computed tomography of the cervical spine, functional radiography of the cervical spine, electroneuromyography, etc.). Results. The results demonstrated that all patients who underwent surgical intervention for single- and multilevel intervertebral hernias with radicular compression syndrome exhibited favorable outcomes. In the postoperative period and during the follow-up period up to 12 months, a good result was revealed in the form of complete regression of neurological and neurological symptoms. In the case of pronounced stenosis of the spinal canal due to intervertebral herniated disks and hypertrophied yellow ligament with myelopathic symptoms and a possible high risk of worsening of neurological symptoms, a good result was revealed in the form of complete regression of neurological symptoms [1]. The patient presented with neurological symptoms, which were surgically treated in two stages. Conclusion. In patients presenting with myelopathic symptoms, including motor and sensory disturbances and pelvic disturbances, complete recovery of neurological symptoms was observed during follow-up. During the observation period, there was complete regression of neurological symptomatology.
Keywords: Cervical disc herniations, Degenerative neck disease, Cervical stenosis, Laminoplasty, Discogenic myelopathic syndrome
Cite this paper: Yuldashev Ravshan Muslimovich, Shukurov Xumoyuddin Asliddin O’g’li, Ruzimurodov Muhammad Faxritdinovich, Surgical Treatment of Degenerative Diseases of the Cervical Spine, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1317-1320. doi: 10.5923/j.ajmms.20241405.35.
1. Introduction
- Degenerative diseases of the spine are on the rise worldwide, including in Uzbekistan. Cervical spondylosis and intervertebral disc degeneration can lead to radiculopathy or myelopathy due to progressive stenosis of the spinal canal and deformation of the interarticular surfaces. An epidemiologic study conducted over 14 years in Rochester (Minnesota, USA) showed that cervical radiculopathy is 83.2 cases per 100,000 population. Although conservative therapy is effective in the majority of patients with degenerative manifestations or disc herniation, many patients require surgical treatment due to the progression of symptoms or the ineffectiveness of conservative treatment [9]. As is known, the spine is the basis of the musculoskeletal system and, due to upright posture, is regularly subjected to significant statodynamic loads. Due to the above reason, dystrophic pathologies are diagnosed relatively [2] early in the spine. Vascular obliteration of intervertebral discs noted in childhood significantly aggravates degenerative processes. The literature presents data that the genetic determinism of intervertebral disc lesions often manifests in the form of inherited collagen structure disorder. To a large extent, the development of degenerative processes in the spine is caused by injuries, as well as traumatic disorders of statics, manifested in the form of limitation of mobility in joints, diseases, and pathology of knee and hip joints. A recent study shows that 79% of the population aged 18-44 years have smartphones, and practically all the time, the cervical spine is in an involuntary physiologic position. Prolonged use of smartphones and sitting at a computer directly affects the cervical spine. Forward bending of the head is reflected in varying degrees on the load on the spine - when the head is bent forward at 15 degrees, the force of the load on the neck is equal to 12kg, at 30 degrees, 18kg, at 45 degrees 22kg and at 60 degrees up to 27 kg, at 90 degrees the model prediction was not reliable]. Prolonged use of smartphones, prolonged time spent in front of the computer, and a sedentary lifestyle usually cause neck pain and soreness - further, it all leads to degenerative changes in the intervertebral discs. Degenerative changes most often occur in the cartilage structures of intervertebral discs and arch joints, as evidenced by clinical signs of cervical osteochondrosis and deforming spondylosis and spondyloarthritis, often combined [4,6]. The objective of this study is to evaluate and enhance the surgical management of degenerative diseases affecting the cervical spine.
2. Materials and Methods
- The results of the examination and surgical treatment of 76 patients with degenerative diseases of the cervical spine during 2022-2023 in the conditions of the Republican Scientific Center of Neurosurgery under the Ministry of Health of the Republic of Uzbekistan with degenerative diseases of the cervical spine were analyzed. The number of women was 29 patients, and the number of men was 46 patients. The mean age of the patients was 53.8 (28-83) years. The majority of patients were aged 50-60 years. The average hospital stay was 10.36 bed days. According to the number and level of affected vertebral-motor segments, multilevel lesions of vertebral-motor segments prevailed - 41 patients, followed by 20 patients with C5-C6 disc herniation, 11 patients with C6-C7 disc herniation, three patients with C4-C6 herniation and one patient with C3-C4 disc herniation. Neurologic status was evaluated in all patients for motor and sensory impairment, symptoms of nerve root or spinal cord compression, and pelvic organ dysfunction. Changes in the cervical spine were evaluated: fixed deformity, changes in cervical lordosis, and tone of periorbital muscles. All patients underwent radiographic examination with functional loads, CT, and MRI examinations of the cervical spine. Electroneuromyography was performed to detect neurologic deficit and myelopathic syndrome [4].
3. Results and Discussion
- Multilevel compression was detected in 41 patients, and single-level compression in 35 patients. Based on clinical parameters, 47 patients underwent surgical treatment, including discectomy and spondylodesis with cage (Peek cage and Plate anterior fixation system by Double Medical, ChM, and GS Medical) (Figure 1), six patients underwent laminoplasty (laminoplate posterior fixation system by Double Medical) (Figure 2), and 23 patients underwent decompressive laminectomy. The operation of anterior cervical spondylodesis is the "gold" standard of surgical treatment of patients with degenerative disease of cervical intervertebral discs.
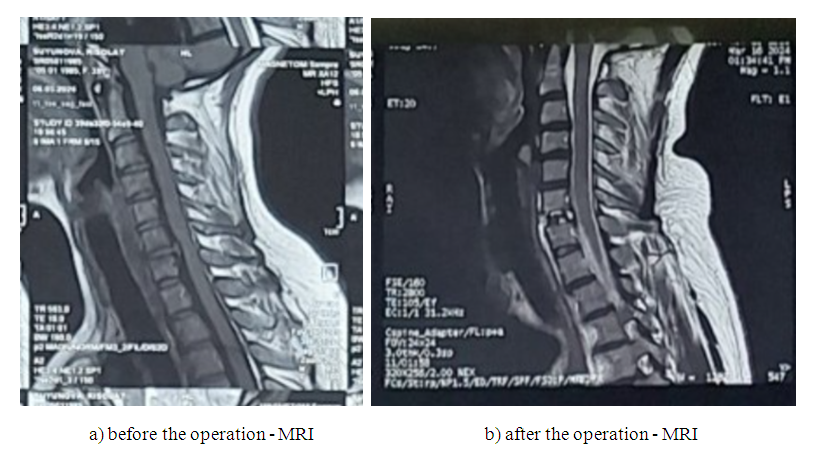 | Figure 1 |
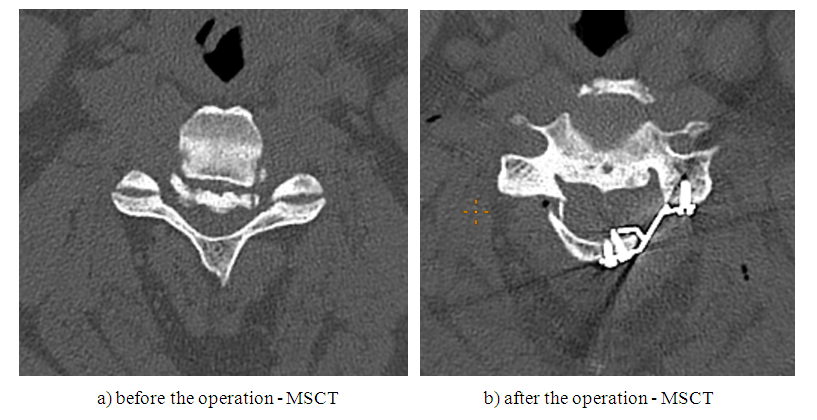 | Figure 2 |
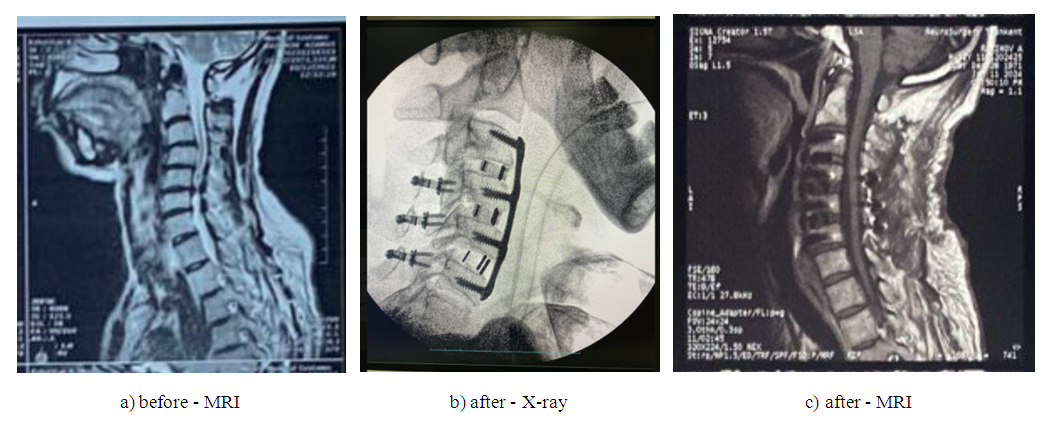 | Figure 3 |
4. Conclusions
- Thus, the indications for surgical treatment of single- and multilevel discogenic compression in the cervical spine include pain syndrome, radiculopathy syndrome, and myelopathy. In case of ineffectiveness of conservative treatment along with conservative treatment, in case of pronounced deforming processes of the cervical spine, surgical treatment significantly reduces disability. It improves the quality of life of patients. It has been established that the primary goal of surgical treatment of patients with discogenic compression of the cervical spinal cord and its manifestations in the form of radicular and myelopathic symptoms is decompression of nerve structures and stabilization of the spinal segment. Myelopathy requires more extensive decompression due to the leading role of the vascular factor in the pathogenesis of its development and the focus of myeloischemia due to compression of the spinal cord by herniation and hypertrophied yellow ligament; such patients should be treated in two stages - posterior decompression laminectomy or laminoplasty and anterior discectomy. The two-stage surgery performed in our clinic with pronounced neurological symptoms showed the best results of surgical treatment in the form of complete recovery of neurological symptoms. Early diagnosis and early surgical treatment in patients with spinal canal stenosis also influence the outcome of surgical treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML