-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1314-1316
doi:10.5923/j.ajmms.20241405.34
Received: Apr. 26, 2024; Accepted: May 15, 2024; Published: May 18, 2024

Features of Humoral Immunity in Patients with Zoonotic Cutaneous Leischmaniasis
Makhmudov Farkhod Akhmedovich1, Khaitov Kakhramon Nazhmitdinovich2
1Bukhara State Medical Institute, Uzbekistan
2Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Cutaneous leishmaniasis (CL), the most commonly reported form of the disease, is identified by ulcerative skin lesions. It is caused by Leishmania major transmitted by Phlebotomus papatasi, and rodent species Psammomys obesus, Meriones libycus, Nesokia indica and Rhombomys opimus serve as non-human reservoirs. Visceral leishmaniasis (VL) is the most severe form of the disease, in which the pathogen disseminates to internal organs such as the liver, spleen, and bone marrow [2,3].
Keywords: Visceral leishmaniasis, Leishmanial RNA virus, Pharynx, Larynx, Trachea
Cite this paper: Makhmudov Farkhod Akhmedovich, Khaitov Kakhramon Nazhmitdinovich, Features of Humoral Immunity in Patients with Zoonotic Cutaneous Leischmaniasis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1314-1316. doi: 10.5923/j.ajmms.20241405.34.
Article Outline
1. Introduction
- Leishmaniasis occurs in 98 countries around the world. 72 countries of these are developing countries, furthermore, 13 of which are the poorest in the world. Unfortunately, the infection is poorly differentiated and diagnosed, so many cases remain unrecognized. Studies conducted by foreign specialists indicate that the etiological factor of the disease may not be leishmania itself, but the virus contained in it (LRV - leishmanial RNA virus). It was first discovered in 1988 in a patient infected with L. guyanensis [1,4,8].Cutaneous form (CL) is characterized by the appearance of leishmaniomas on the skin as specific granulomas lesions consisting of plasma cells, neutrophils, lymphoid cells, passing through the stages of tubercle-ulcer-scar [9,10,11]. Mucocutaneous leishmaniasis is accompanied by damage to the mucous membranes of the mouth, nose, pharynx, larynx, trachea, spreading to the soft tissue of the lips and cartilage tissue (REF). Diffuse CL manifests itself as multiple infiltrates, papules and nodules on the skin [5,6,9].
2. Purpose of the Study
- To identify the characteristics of humoral immunity in patients with zoonotic CL.
3. Materials and Methods
- 70 patients hospitalized with zoonotic CL from different districts of the Bukhara region Uzbekistan were selected for observation. The diagnosis of zoonotic CL was established at the initial visit based on the medical history, clinical pictures, physical examination, and analysis of laboratory parameters (What are they?). All studied patients underwent examination and treatment at the regional dermatovenerological dispensary (REF).Cutaneous leishmaniasis was diagnosed based on skin scraping material (REF). Before sampling, it is necessary to ensure good homeostasis to prevent blood from entering the sample, which is achieved by squeezing the element. The best sampling location is in the immediate vicinity of the ulcer or its active border (REF). Using a sharp scalpel, a superficial incision is made 1-2 mm deep, 5-8 mm long, and the tissue elements and tissue fluid are scraped off with the end of the scalpel (REF). Stained according to Romanovsky-Giemsa (REF).To identify features in the indicators of humoral immunity before and after treatment, all 70 patients were divided into two groups depending on the method of therapy received: From Bukhara city.Group I - 35 patients with PCL (Full name) who received standard treatment, which included antiparasitic (scientific name and dose), antimycotic (scientific name and dose), immunomodulators (scientific name and dose), non-steroidal anti-inflammatory drugs (scientific name and dose), as well as local treatment with ointments (scientific name and dose) for 10 days.Group II – 35 patients with PCL who; in addition to standard treatment, were prescribed a bioactive supplement - L-arginine powder (Source). Children under 10 years old were prescribed L-arginine 250 mg/what? twice a day for 10 days (REF), and over 10 years old 500 mg/what? twice a day for 10 days (REF). These groups were representative in terms of age, clinical forms, and duration of the disease, which made it possible to obtain objective and reliable results.Statistical processing of the obtained results was carried out using the methods of variation statistics by the application package Statistica for Windows (REF). Digital data was processed on a personal computer using the memory of Microsoft Excel application programs (REF).
4. Results and Discussions
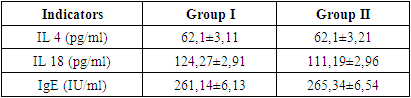
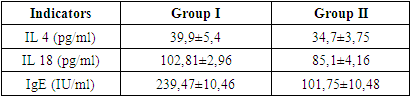
- An immunological study (included what parameters) was carried out on the first day after admission to the hospital before the start of treatment and the analysis of the data is shown in Table 1.
|
|
5. Conclusions
- Zoonotic cutaneous leishmaniasis is expressed by an increase in the content of the anti-inflammatory cytokine IL-4 and the proinflammatory cytokine IL-18, as well as IgE, which are directly dependent on the clinical form and duration of the disease. In patients with PCL before treatment, there was an increase in the concentration of the cytokine IL-4, both in group I and group II by 2.48 times compared to normal values, IL-18 by 1.77 and 1.58 times, IgE by 2.61 and 2.65 times, respectively.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML