Tagaev Ilhom Ulashevich, Shamsiev Jamshid Azamatovich, Maxmudov Zafar Mamadjanovich
Samarkand State Medical University Uzbekistan, Samarkand, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Intussusception is a serious condition, especially in children, and requires a quick and accurate diagnosis, as well as effective treatment to prevent complications. This article discusses modern approaches to the diagnosis and treatment of intussusception in children, as well as presents innovative methods aimed at improving the accuracy of diagnosis and the effectiveness of treatment.
Keywords:
Intussusception, Children, Diagnostics, X-ray, Ultrasound, Hydroechocolonography, Conservative treatment
Cite this paper: Tagaev Ilhom Ulashevich, Shamsiev Jamshid Azamatovich, Maxmudov Zafar Mamadjanovich, Improving Diagnosis and Treatment Intussusception in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1300-1303. doi: 10.5923/j.ajmms.20241405.31.
1. Introduction
Intussusception (IC), or telescopic bowel, is a condition in which one section of the intestine is retracted into another [5,7]. In children, this condition often occurs as a result of infections or hyperplasia of the lymph nodes. Rapid and accurate diagnosis of intussusception is critical, as delayed treatment can lead to serious complications such as tissue necrosis and peritonitis [1,3,4,9].Among acute surgical diseases of the abdominal organs in children, acute intestinal obstruction (ACN) is 1.2 - 9.4%, ranking second after acute appendicitis, but, at the same time, the incidence of adverse outcomes is much higher than in other forms of acute abdominal pathology. Intussusception is the most common type of acquired intestinal obstruction in children, ranking second among urgent pathologies of the abdominal organs after acute appendicitis [1,2,13]. The urgency of the problem is also determined by the high frequency of diagnostic errors, both at the pre-hospital and inpatient stages, which do not tend to decrease. At the pre-hospital stage, the frequency of diagnostic errors reaches 75-85%. Currently, the mortality rate for intussusception ranges from 0.5 to 1%, reaching from 6 to 14.5% in complicated forms [6,8,10,11,12]. The objective difficulties in the diagnosis and treatment of IC are largely associated with the inconsistency of anamnestic data, the presence of intercurrent diseases, the limited possibilities of traditional X-ray diagnostics, as well as the persistence of disagreements in the choice of conservative or surgical methods of treatment and their timing.Research objective: Improving the results of treatment of intussusception in children by improving diagnostics and optimizing treatment tactics.
2. Materials and Methods of Research
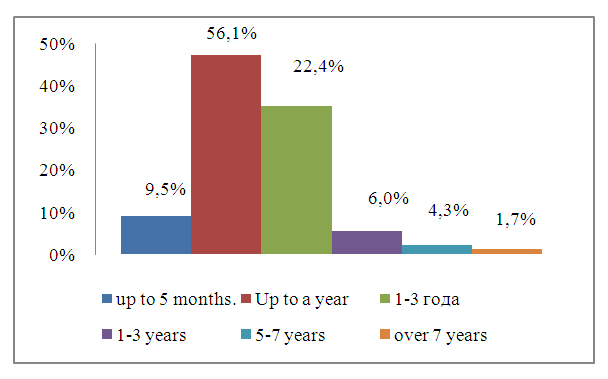
Over the past 20 years, 237 children aged 3 months to 12 years have been hospitalized in the Emergency Surgery Department of the Specialized Pediatric Surgical Clinic of Samara State Medical University with a diagnosis of intussusception, of which this diagnosis was confirmed in 116 during the clinical examination. In the remaining 125 patients, IC was excluded. Boys – 85 (73.3%), 31 (26.7%) girls. There were 76 (65.5%) patients under 1 year of age, 26 (22.4%) patients under 3 years of age, and 14 (12.1%) patients over 3 years of age. Intussusception was most common between the ages of 6 months and 1 year (76 people (65.5%) (Fig. 1).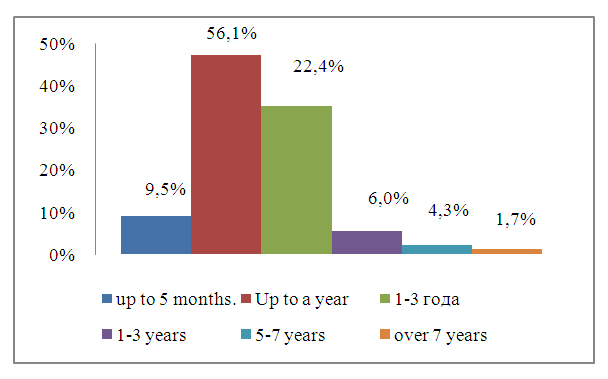 | Figure 1. Distribution of subjects by age |
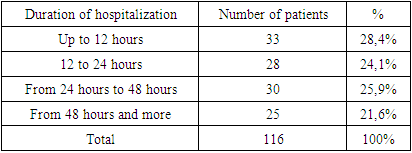
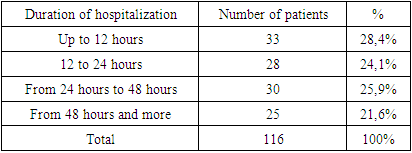
33 children (28.4%) were admitted within 12 hours from the onset of the disease, 28 (24.1%) within 12 to 24 hours, 30 (25.9%) within 25 to 48 hours, and 25 (21.6%) within more than 48 hours (Table 1).Table 1. Terms of admission of patients to the hospital
 |
| |
|
The complex of examinations included anamnesis, examination, palpation of the abdomen under medicated sleep, digital rectal examination, laboratory examination, radiography, pneumoirrigoscopy and ultrasound examination (ultrasound).Depending on the therapeutic and tactical approaches used, all examined patients with IC were divided into 2 groups. The first group (comparison group) consisted of 43 patients treated in the period from 2008 to 2013. In this group, diagnosis was based on R-graphy and pneumoirrigoscopy under fluoroscopy. The second group (the main group) consisted of 73 patients with IC treated from 2014 to the present. In this group, diagnosis and conservative diagnosis is based on the technique of hydroechocolonographic disinsusception (HEG) of 1.5% sodium chloride under ultrasound control.
3. Results of the Study and Their Discussion
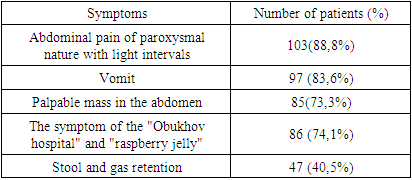
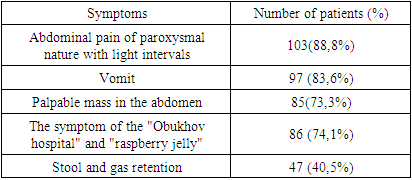
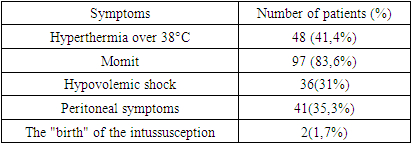
The most common factors in the development of the disease were intestinal disorders (31%), the introduction of new foods into the diet (27%), and dietary errors (24%). IC occurred in 4 (3.5%) children with acute respiratory infection.The main clinical manifestations of typical ileocecal intussusception were the so-called classical Mondor triad: ü the appearance of sudden attacks of anxiety in the child with "light intervals" due to ischemic cramping pain in the abdomen;ü bloody discharge from the anus in the form of raspberry jelly;ü palpable mass in the abdominal cavity.Table 2 presents the incidence of clinical symptoms in IC: the main symptoms were cramping abdominal pain (88.8%), vomiting (83.6%), and palpable intussusception in the abdominal cavity (73.3%).Table 2. Symptom Frequency in IC in Study Patients
 |
| |
|
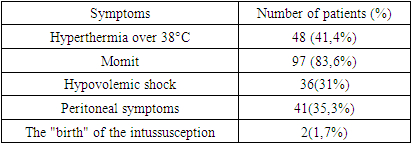
Clinical signs of a complicated course of IC were observed in patients with a period of admission of more than 3 days - hyperthermia over 38°C - in 41.4% of patients, vomiting in 83.6%, in 49% - peritoneal symptoms. In 2 cases, the phenomenon of "birth" of intussusception from the anus, very similar to rectal prolapse, was observed on admission (Table 3).Table 3. Clinical signs of complicated IC
 |
| |
|
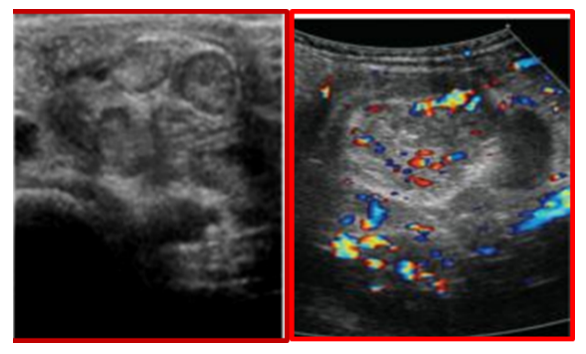
On the basis of clinical, instrumental and intraoperative data, the following types of IC were revealed: • ileocecal - 109 (94%)• small intestine – 6 (5.2%)• colon – 1 (0.8%)Until 2014, the main method of examination in the diagnosis of IC was radiologically-guided pneumoirrigoscopy. The invaginate was visualized as a homogeneous oval-shaped shadow with even contours – the head of the invaginate.Significant prospects are associated with the introduction of ultrasound diagnostics of IC into clinical practice. Since 2014, ultrasonogroaphy has been introduced as the main method for diagnosing IC. Ultrasound revealed classic echo symptoms – the "target" symptom and "pseudokidney", which are the gold standard of ultrasound diagnostics of IC (Fig. 2). | Figure 2. Visualization of intussusception on ultrasound |
Late ultrasound signs: localization of the head in the left half of the abdominal cavity, accumulation of fluid between the layers and in the head of the intussusception, absence of peristalsis, the presence of enlarged lymph nodes. Color Doppler Mapping (CDM) can assess the degree of intestinal viability (Fig. 3).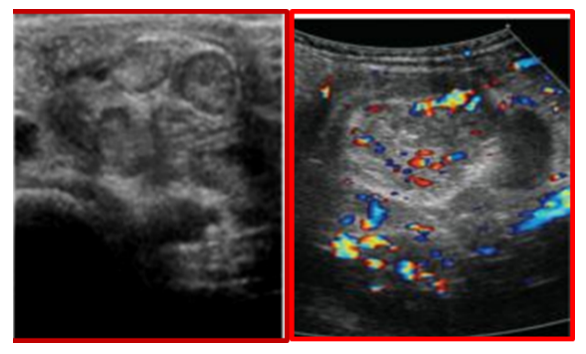 | Figure 3. Visualization of the intussusception on the CDM |
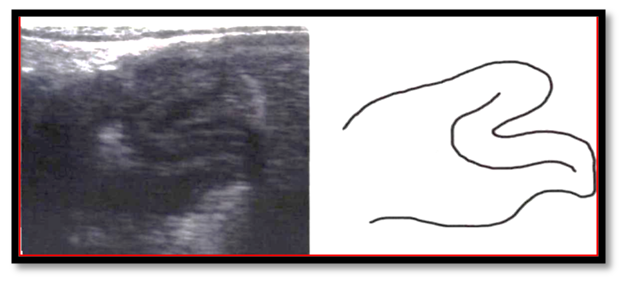
In addition, additional symptoms of IC may be identified. The symptom of "forceps" is the visualization of the head of the invaginate on a longitudinal scan (Fig. 4).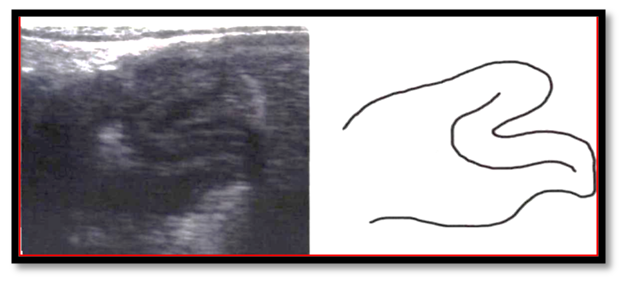 | Figure 4. Diagram and ultrasound image with the symptom of "forceps" in IC |
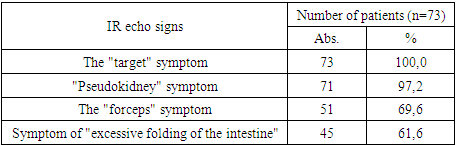
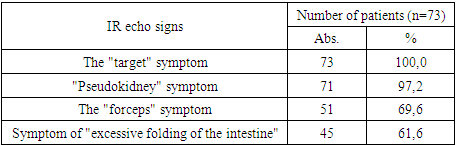
Table 4 shows the frequency of IC echographic symptoms. The symptoms of "target" (100%) and "pseudokidney" (97%) were characterized by the highest diagnostic informativeness. Thus, the use of ultrasound in the diagnosis of intussusception as a screening method makes it possible to bring the effectiveness of complex diagnosis of IC disease closer to 100%.Table 4. Frequency of echo signs in IC
 |
| |
|
Depending on the therapeutic and tactical approaches used, all examined patients with IC were divided into 2 groups.The first group (comparison group) consisted of 43 patients treated in the period from 2000 to 2013. In this group, the diagnosis was based on R-graphy and P-guided pneumoirrigoscopy, and in the treatment plan, 21 patients underwent conservative pneumatic invagussusception under X-ray control, and 22 children underwent surgical intervention. After conservative correction of the IR, x-ray control of the intestinal passage with barium was performed. The technique of pneumatic disinvaginaci under fluoroscopic control for the purpose of conservative rectification of the intussusception was performed in 25 patients. At the same time, successful rectification of intussusception was achieved in 21 patients.The second group (the main group) consisted of 73 patients with IC treated from 2014 to the present. In this group, diagnosis is based on ultrasound, conservative treatment was performed by hydroechocolonographic disinsusception (HEC) of 1.5% sodium chloride solution under ultrasound control in 39 (53.4%) patients, 34 (46.6%) patients were operated on in this group. Ultrasound-guided hydroechocolonography (SEC) for conservative intussusception was performed in 52 patients In the second group, it was possible to straighten the intussusception in 39 (53.4%) patients, and in 7 patients with a disease history of more than 24 hours. After the intussusception is straightened by this method, the passage of the gastrointestinal tract with barium is practically not used, but ultrasound control is carried out in dynamics.Treatment according to this technique is started for all admitted children after ultrasound confirmation of the presence of intussusception, regardless of the age of the disease and the age of the child, in the absence of peritoneal phenomena, shock and echo signs of small intestinal intussusception.Surgical interventions in IC were performed in 56 (48.3%) patients, including 22 (19.0%) patients in the first group and 34 (29.3%) patients in the second (main) group. Manual disinvagination (39), disinvagination and resection followed by anastomosis (14), bowel resection followed by ileostomy (3). A comparative evaluation of methods for the treatment of intussusception has shown that the introduction of ultrasonography in the diagnosis and treatment of IC has significantly improved treatment outcomes.• the number of conservatively cured patients has increased;• the average length of stay in the hospital has been reduced;• Radiation exposure has decreased.
4. Conclusions
Ultrasonography is the main and safe method of IC diagnostics, which allows you to bring the effectiveness of complex diagnostics closer to 100% and is important in the choice of treatment tactics. The duration of the disease in IC in children is not a contraindication to an attempt to use conservative treatment tactics. The only contraindication to the use of conservative treatment is clinical signs of peritonitis.Ultrasound-guided hydroechocolonography (GEC) allows for successful disinsussusception, a sharp reduction in the number of X-ray examinations and, thereby, a reduction in the overall radiation exposure to the patient and staff, as well as a significant increase in the percentage of conservatively cured patients.Further research into the development of new diagnostic methods, also aimed at the early detection of intussusception in children, as well as research to improve surgical techniques, could significantly improve the effectiveness of treatment and reduce the risk of complications.Overall, improving the diagnosis and treatment of intussusception in children is a key aspect of improving patient outcomes and quality of life, requiring further research, development, and innovation in clinical practice.
References
| [1] | Belyaev MK. (2004). Experimental substantiation of the safety of conservative treatment of intussusception in children. Pediatric surgery. 3:11-14. |
| [2] | Digtyar VA, Savenko MV ta in. (2016). Ultrasound diagnostics of intestinal infection in children. Zbirnik naukovikh prats spivrobitnikiv NMAPO im. PL Shupika. 25. Kiev: 141-147. |
| [3] | Dronov AF, Poddubny IV. (2000). Laparoscopy in the diagnosis and treatment of intestinal intussusception. Pediatric surgery.6: 33-38. |
| [4] | Isakov Law School, Razumovsky Law School. (2015). Pediatric surgery. Moscow: 1040. |
| [5] | Kazakov AN, Yusufov AA. (2015). The role of ultrasound in the diagnosis and treatment of intestinal intussusception. Materials of the III interuniversity scientific and practical conference of young scientists. Tver: 128. |
| [6] | Kuzmichev PP, Voronov AV, Kuzmicheva NE. (2017). Abdominal compartment syndrome in children. Khabarovsk: 96.7. |
| [7] | Tailor VM. (1964). Substantiation of the conservative method of treatment of acute intestinal intussusception in children. Dnepropetrovsk: 280. |
| [8] | Rusak PS, Rybalchenko VF, Stakhov VV. (2015). Modern aspects of the diagnosis and treatment of intestinal intussusception in children. Topical issues of pediatric surgery. In the book: A collection of materials of the VII Republican scientific and practical conference with international participation dedicated to the 30th anniversary of the Department of Pediatric Surgery. Grodno: 277-278. |
| [9] | Sushko VI, Krivchenya DU, Degtyar VA. (2014). Surgery for children. Kyiv: 586. |
| [10] | Shamsiev Zh. A., Togaev I. U., Mahmudov Z. M., Shamsiev Sh. Zh., Shamsiev B. M. Optimization of methods of diagnosis and treatment of intestinal intussusception in children. Scientific journal on theoretical and practical problems of biology and medicine "Problems of medicine and Biology". 2021, No. 6.1 (141), pp. 461-465. |
| [11] | Bax KNMA, Georgeson KE, Rothenberg SS, Valla J-S, Yeung CK. (2008). Endoscopic Surgery in Infants and Children. Berlin: SpringerVerlag Berlin and Heidelberg GmbH & Co: 833. |
| [12] | George WH, Patrick JM, Daniel JO. (2014). Ashcraft’s Pediatric Surgery. (6th ed.). London; New York: Saunders: 1192. |
| [13] | Hamilton BD, Chow GK, Inman SR, Stowe NT, Winfield HN. (1998). Increased intra-abdominal pressure during pneumoperitoneum stimulates endothelin release in a canine model. Journal of endourology. 12 (2): 193. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML