-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1278-1280
doi:10.5923/j.ajmms.20241405.26
Received: Apr. 1, 2024; Accepted: May 3, 2024; Published: May 14, 2024

Clinical and Epidemiologic Characteristics of Patients with Myasthenia Gravis in the Fergana Region
Maksudova H. N., Magsumova R. A., Umarova D. B.
Tashkent Pediatrics Medical Institute, NBF Clinic, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Myasthenia gravis is a classic autoimmune disease that manifests muscle weakness and fatigue due to auto aggression and antibody formation to various antigens of the peripheral neuromuscular apparatus. Currently, there is an increase in the incidence of myasthenia gravis and its combination with other diseases, not only autoimmune diseases. In this study we studied the clinical and neurological features and diagnostic methods.
Keywords: Myasthenia gravis, Forms, Diagnosis, Proserpine test
Cite this paper: Maksudova H. N., Magsumova R. A., Umarova D. B., Clinical and Epidemiologic Characteristics of Patients with Myasthenia Gravis in the Fergana Region, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1278-1280. doi: 10.5923/j.ajmms.20241405.26.
Article Outline
1. Relevance
- The relevance of the problem is determined by the fact that recently there has been a tendency to increase the incidence of myasthenia gravis, as well as its combination with other, not only autoimmune, diseases. The frequency of the disease has now increased and ranges from 1 to 24 cases per 100000 population, despite the undoubted progress in understanding the mechanisms of myasthenia gravis development, improvement of methods of its diagnosis and treatment. [1,2,6] However, it is known that the main damaged link in myasthenia gravis is the acetylcholine receptor (AChR) of the postsynaptic membrane of the neuromuscular junction. Increased levels of autoantibodies to AChR are detected in most patients with the generalized form of the disease and account for almost 85% of all cases. [3] However, a lot of studies have shown that there is no correlation between the concentration of AT to AChR and the severity of the clinical picture in patients with myasthenia gravis. As a result of recent studies in the literature, it has been reported that the borderline of expected clinical improvement is the reduction of autoantibodies by more than 20%, and the reduction of AT levels by 50% or more is accompanied in most cases by a clear positive clinical effect. [4,5]Objective of the study. To study clinical and neurological features of myasthenia gravis.
2. Materials and Methods of the Study
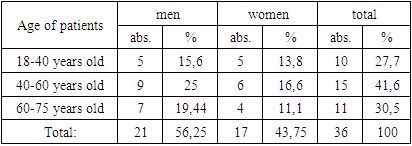
- 36 patients with myasthenia gravis were included in the study. Anamnesis of the disease, forms of myasthenia gravis, neurostatuses were studied. Clinical and instrumental examination included ENMG and MRI. Proserine test was also one of the diagnostic criteria of the study.The average age of patients at the time of examination was 49±15 years (from 18 to 70 years), men - 11 (52.4%), women - 10 (47.65). The data on the sex and age composition of the examined patients are presented in Table 1.
|
3. Examination Findings
- In typical cases of the disease, the first signs are disorders in the eye muscles, in which patients may experience drooping eyelids, double objects. Neurological examination reveals ptosis, often asymmetrical. The intensity of ptosis varies throughout the day, depending on physical activity. Usually, ptosis increases in the evening, sometimes manifests itself when fixing the gaze. Lesion of the bulbar muscles leads to dysfunction of the soft palate and epiglottis, which is manifested in difficulty swallowing, changes in the sound of the voice ("nasal" tinge, "fading") and fatigue when talking. In patients with generalized form of myasthenia gravis, one of the most serious manifestations is weakening of the respiratory muscles. This leads to dyspnea on physical exertion and sometimes even at rest.Ocular form of myasthenia gravis, 1 (3%) bulbar form, and 31 (86%) generalized form were detected in 4 (11%) patients. (Figure 1)
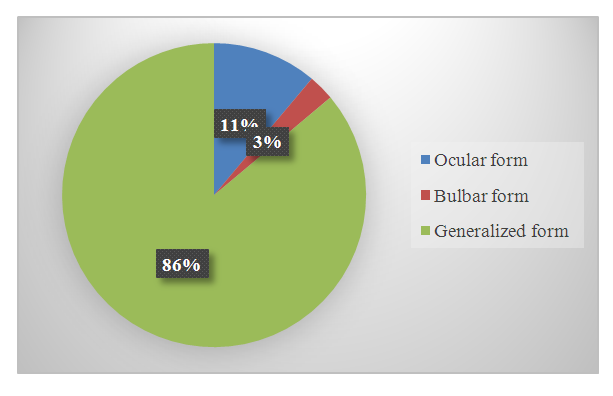 | Figure 1. Forms of myasthenia gravis |
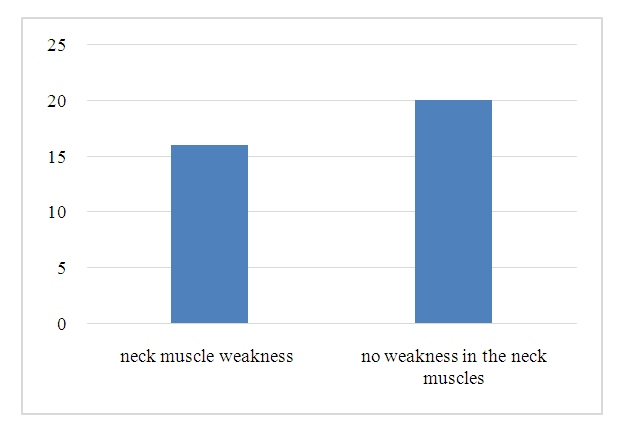 | Figure 2. Presence of neck muscle weakness |
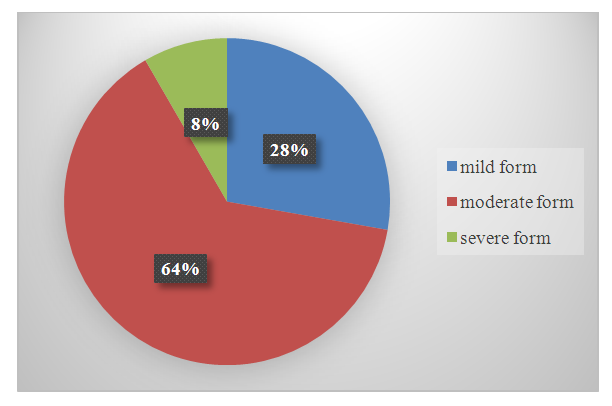 | Figure 3. Degrees of severity of myasthenia gravis |
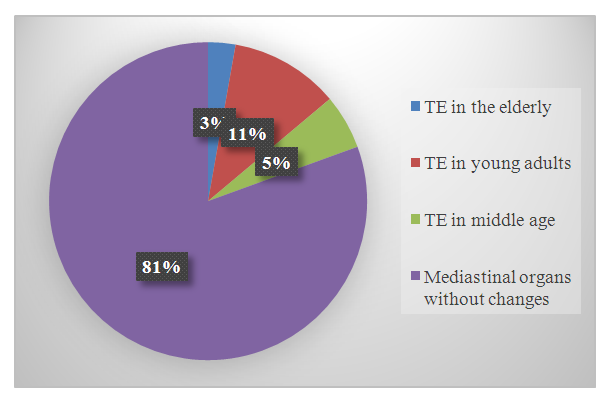 | Figure 4. History of TE |
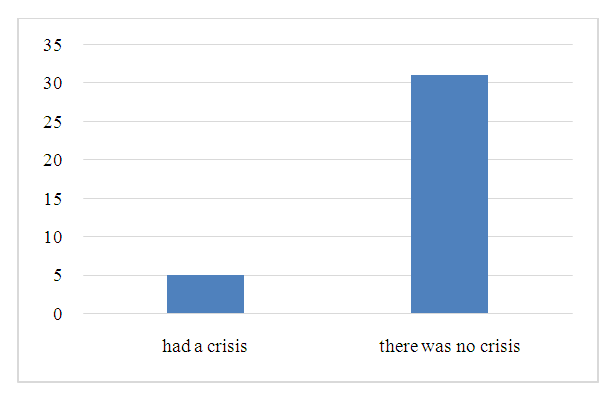 | Figure 5. Presence of a history of myasthenic crisis |
4. Conclusions
- Thus, the generalized form of myasthenia gravis was mainly observed in 31 (86%) patients, ocular form of myasthenia gravis was detected in 4 (11%) patients, and bulbar form was detected in 1 (3%). Patients with mild 10 (27,7%), with moderate 23 (63,88%), and only 3 (8,3%) had severe myasthenia gravis were more frequent. Progress in the study of the causes and treatment of myasthenia gravis in recent years has led to a decrease in mortality and improved quality of life of patients with this disease. Modern research methods allow not only to detect the disease, but also to predict its nature.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML