-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1267-1272
doi:10.5923/j.ajmms.20241405.24
Received: Apr. 19, 2024; Accepted: May 7, 2024; Published: May 13, 2024

Exploring the Capabilities and Future Outlook of Ultrasound in Rheumatology
Ametova Alie Servetovna
Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Ametova Alie Servetovna, Samarkand State Medical University, Samarkand, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Currently, ultrasound examination (US) is one of the most informative methods of imaging examination. Due to its portability, accessibility, speed of implementation, relatively low cost and almost complete absence of contraindications, ultrasound appears to be an effective method not only for diagnosis, but also for assessing the quality of treatment. This method is highly informative in visualizing the tendon-ligament apparatus, hyaline cartilage, cortical bone and para-articular soft tissue, which significantly expands the diagnostic and treatment capabilities of a rheumatologist and allows monitoring the effectiveness of treatment. This review discusses the possibilities of using ultrasound in the diagnosis of a number of rheumatological diseases, such as rheumatoid arthritis, osteoarthritis, spondyloarthritis, gout, and tendon lesions due to hypercholesterolemia. The possibilities of using sonoelastography (a method that allows you to determine the elasticity of soft tissue structures) in the diagnosis of rheumatic diseases are also considered. According to the authors, sonoelastography may soon become firmly established in clinical practice as a first-line diagnostic method for identifying biomechanical changes in tendons, muscles, and ligaments, as well as assessing the effectiveness of treatment. Conducting an ultrasound of the musculoskeletal system significantly increases the diagnostic and therapeutic capabilities of the clinician.
Keywords: Rheumatic diseases, Ultrasound examination of the musculoskeletal system, Osteoarthritis, Spondyloarthritis, Rheumatoid arthritis, Gout, Sonoelastography
Cite this paper: Ametova Alie Servetovna, Exploring the Capabilities and Future Outlook of Ultrasound in Rheumatology, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1267-1272. doi: 10.5923/j.ajmms.20241405.24.
Article Outline
1. Introduction
- The problem of joint diseases remains complex and requires an integrated approach to diagnosis and treatment with the involvement of specialists in various fields: radiation diagnosticians, orthopedic traumatologists, rheumatologists, rehabilitation specialists, physiotherapists, etc.As of 2013, the prevalence of diseases of the musculoskeletal system in Russia was 14,247 per 100 thousand population [1]. According to E.A. Galushko and E.L. Nasonova, the true prevalence of rheumatic diseases, obtained during an epidemiological study, exceeds official statistics by 2.5 times for rheumatoid arthritis (RA), 5 times for osteoarthritis (OA), 3.5 times for spondyloarthritis and 3 times - for systemic connective tissue diseases [2].The incidence of almost all age groups of the population, the tendency to become chronic and the steady progression of rheumatic diseases determine the importance of their early diagnosis. Detection of the disease at an early stage makes it possible to prevent permanent disability, a pronounced decrease in the quality of life and a significant increase in the cost of treatment.Modern ultrasound examination (US) of the musculoskeletal system significantly increases the diagnostic and therapeutic capabilities of the clinician. Interest in expanding the scope of ultrasound in the diagnosis of diseases of the musculoskeletal system is confirmed by the constant increase in the number of publications devoted to the study of this issue [3].Due to its portability, accessibility, speed of implementation, relatively low cost and almost complete absence of contraindications, ultrasound appears to be an effective method not only for diagnosis, but also for assessing the quality of treatment [4].The first works on ultrasound diagnostics of joints, which appeared in the 1970s, were devoted to the study of large joints and the most accessible periarticular soft tissues, in particular the diagnosis of Baker's cyst [5]. In 1972, McDonald and Leopold first made a differential diagnosis between thrombophlebitis and rupture of Baker's cyst [6]. They were the first to propose using the ultrasound scanning method as a screening test in cases of swelling in the popliteal region.At the same time, the first works on the use of ultrasound in rheumatology appeared, mainly devoted to the diagnosis of changes in the knee joints in rheumatoid arthritis [7].Currently, in world practice, ultrasound is one of the most informative methods of visualization of joints due to its high resolution in visualizing the tendon-ligament apparatus, blood vessels, hyaline cartilage and cortical bone.In addition, ultrasound is a direct contact between the researcher and the patient, making it possible to focus on the area of concern directly during the examination. When performing an ultrasound scan of a joint, compression by the sensor serves as a guide in finding the pathological area. Such an examination does not require any special training or bulky equipment and is carried out in a short time [8].Ultrasound data are currently included in the classification criteria for a number of diseases [9]. Thus, the presence of subdeltoid bursitis, biceps tenosynovitis or shoulder synovitis is included in the European League Against Rheumatism (EULAR) classification criteria for polymyalgia rheumatica.Each joint consists of articular surfaces of bones covered with cartilage; the articular cavity and the articular capsule surrounding the joint and strengthened by ligaments. Additional elements of the joint include structures such as menisci, intra-articular ligaments and sesamoid bones [10]. The bones that form the joint completely reflect ultrasound, so their volumetric visualization is impossible. They are located as echogenic linear formations, leaving a wide acoustic shadow. Hyaline cartilage is normally visualized as a narrow hypo- or anechoic strip, the structure and thickness of which can be assessed echographically. The capsule is located only in large joints. Menisci in cross section are visualized as homogeneous triangular echogenic zones. Echography allows you to assess their structure and integrity, as well as identify prolapse into the joint cavity.The ligaments of the joint are visualized as interlacing weakly echogenic lines. Modern high-resolution sensors make it possible to evaluate their structure quite well. The articular cavity is visualized as a narrow anechoic zone. Periarticular soft tissues, changes in which may be associated with joint disease or be a manifestation of independent pathology (tendinitis, myositis, fasciitis), are also easily accessible by ultrasound imaging.The list of indications for ultrasound examination of joints is quite extensive. It should be noted that any changes in the joint area (trauma, pain, limitation of movements, increase in volume, swelling, presence of a palpable formation) [11] require ultrasound for the purpose of primary diagnosis and dynamic monitoring during treatment [8,12,13].The examination of joints is carried out in different sections: longitudinal vertical, transverse and oblique. In addition, to obtain more complete information, the joint is examined in the positions of flexion, extension and rotation [13,14].An ultrasound of the joint involves examining two symmetrical joints, which can be especially important for the differential diagnosis of traumatic joint damage and exacerbation of rheumatic disease provoked by a minor traumatic factor [13,14].The most accessible joints for ultrasound are the shoulder [15,16], elbow, knee [11] and ankle joints. The diagnostic value of ultrasound of a joint such as the hip very much depends on the patient’s physique and is noticeably reduced in people with increased body weight. At the same time, ultrasound of the hip joints in newborns and children in the first year of life is a highly informative method in identifying congenital joint dysplasia [17]. No less important is ultrasound of small joints of the hands, especially in the diagnosis of rheumatoid arthritis [18].
2. Ultrasound in the Diagnosis of Rheumatic Diseases
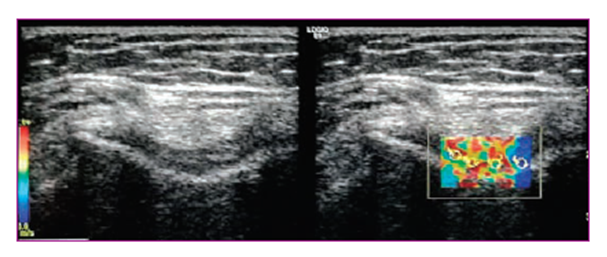
- Rheumatoid arthritisAccording to modern concepts, RA is an autoimmune rheumatic disease of unknown etiology, characterized by chronic erosive arthritis (synovitis) and systemic damage to internal organs [9]. Articular syndrome is the main manifestation of RA. The process involves mainly small joints and periarticular tissues. Early diagnosis of RA ensures rapid initiation of therapy with modern basic anti-inflammatory drugs and the use of genetic engineering biological therapy (GEBT), which allows achieving clinical and laboratory remission with slowing down of inflammatory and destructive phenomena and, ultimately, significantly improving the prognosis of the disease.The pathogenesis of RA is based on the activation of a complex cytokine cascade, leading to inflammatory proliferation of the synovial membrane, the development of severe exudative synovitis, proliferation of a specific pannus with the pathological formation of a vascular network in it, which subsequently leads to the destruction of articular cartilage and subchondral bone. Increased vascularization of the pannus and hypertrophied synovium can serve as an indicator of RA activity, and, conversely, during disease therapy, the vascularization of the pannus and synovium decreases significantly [19]. Ultrasound with color and power Doppler mapping has been shown to be highly sensitive in detecting synovitis in RA. Vascular structures are clearly visualized in places of erosive changes in cartilage and bone.The main criterion for assessing the activity of the inflammatory process is the severity of vascularization of the synovial membrane according to power Doppler mapping (EDC).The leading sign that makes it possible to verify RA is destructive bone damage with the formation of cysts and erosions on the articular surfaces. Bone defects are not always visible in the early stages of RA on X-ray examination.Ultrasound of the hands significantly more often reveals early erosive changes in the joints than radiography [19,20]. Echograms of the joints of patients with RA show significant destruction of the bone structures that form the surface of the joints; erosions are clearly visualized, especially in the area of the heads of the metacarpal bones [20,21].OsteoarthritisUltrasound also plays a significant role in the diagnosis of OA - a heterogeneous group of diseases of various etiologies with similar biological, morphological, clinical manifestations and outcomes, which are based on damage to all components of the joint, primarily cartilage, as well as subchondral bone, synovial membrane, ligaments, capsule, periarticular muscles [9].When performing an ultrasound, thinning of the articular cartilage, the appearance of “fragments” of destroyed cartilage and bone (“articular mice”) in the joint cavity, proliferative changes in the marginal bone articular surfaces (osteophytes), unclear and uneven contours of the articular surfaces, accumulation of fluid in the joint cavity can be visualized, as well as damage to intra-articular structures and the para-articular apparatus in the form of hypo- and dystrophic changes [10,22].Early diagnosis of OA is extremely important, when timely administration of chondroprotectors is effective in influencing still intact articular cartilage. Healthy cartilage is visualized as a smooth, continuous homogeneous anechoic strip of uniform thickness (Fig. 1). With OA, the cartilage becomes unevenly thinned, with unclear contours and an inhomogeneous structure with possible inclusions (Fig. 2) [10,22].
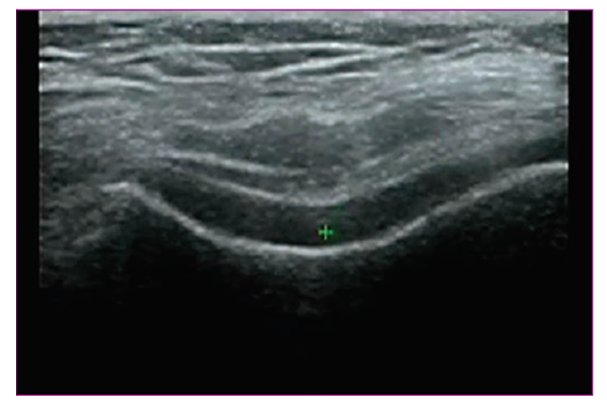 | Figure 1. Normal hyaline cartilage |
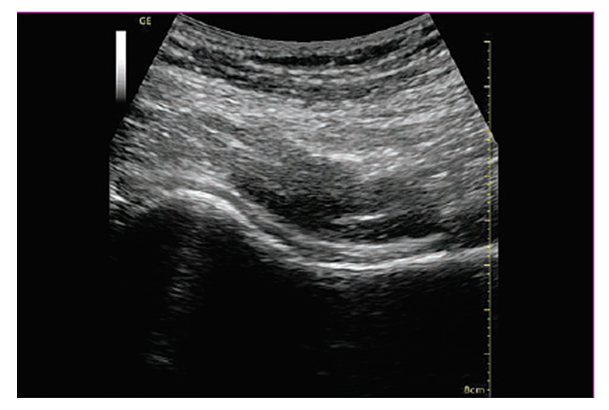 | Figure 2. Hyaline cartilage OA. Reduced thickness, uneven contour, hyperechoic inclusions |
3. Prospects for the Use of Ultrasound in the Diagnosis of Rheumatic Diseases
- Ultrasound diagnostic methods are constantly being improved. New methods are successfully tested and introduced into practice. Thus, a number of studies have shown that when using a contrast agent, the signal from the hypervascularized synovium increases, the color signal intensifies, and synovitis, necrosis or fibrosis in inflammatory joints are more clearly differentiated [26]. Multimodal fusion imaging technology allows ultrasound to be performed with simultaneous display of corresponding CT or MRI slices.With the development of ultrasound methods, it became possible to evaluate the mechanical properties of soft tissues. Thus, sonoelastography allows you to determine the elasticity of soft tissue structures. The method is based on determining the deformability of fabric, which depends on its structure and composition. Elasticity is determined by Young's modulus, which reflects the properties of a material to resist tension or compression during elastic deformation. The main techniques currently used include compression (quasi-static) elastography and shear wave (dynamic) elastography [37–39].The principle of shear wave elastography is based on measuring the velocity distribution of the elastic deformation wave of tissue obtained using an ultrasound pulse. This technique allows not only a qualitative assessment in the form of color elastograms, but also quantitative measurements in kilopascals or centimeters per second [30].It is known that the elasticity of soft tissues such as subcutaneous fat, muscle and connective tissue ranges from approximately 1 to 103 kPa. It was also revealed that malignant neoplasms have greater rigidity compared to normal tissues. This explains the widespread use of the elastography method in the diagnosis of diseases of the liver, mammary, thyroid and prostate glands [30].The elasticity of soft tissue structures of the musculoskeletal system can also be changed under the influence of various pathological processes, such as microdamage, inflammation, fibrosis and calcification.The first publications on the use of elastography to assess the elasticity of skeletal muscles appeared in the mid-1990s. [31]. Since the end of the last decade, separate publications began to appear on the elastographic study of tendons of various locations, primarily the Achilles tendon. A number of publications are devoted to the possibility of obtaining information about tendon stiffness in real time, both normally [22] and with degenerative changes [23], as well as assessing the mechanical properties of the tendon over time during therapy [24]. Interesting, in our opinion, are the findings showing multidirectional changes in density in various ligaments and tendons in tendinopathy. So, B.K. Coombes et al., assessing the density of the Achilles tendon and patellar tendon propria using shear wave elastography, showed an increase in the density of the patellar tendon propria and a decrease in the density of the Achilles tendon in patients with tendinopathy compared with a control group of healthy volunteers [25]. However, some studies show that with Achilles tendon tendinopathy, there is an increase in stiffness in the area of its attachment to the bone (enthesis), most likely due to the formation of enthesophytes and calcification of the tendon [26]. It has also been shown that sonoelastography can detect degenerative changes in the tendons and calcifications in the thickness of the tendons, which are difficult to detect using other research methods [27].Recently, new reports have appeared on the diagnostic capabilities of the elastography method for rheumatological diseases. Thus, E. Cindila et al. a significant difference in the elasticity of the major salivary glands was shown in patients with Sjögren's syndrome [28]. Q. Wang et al. report the use of shear wave elastography to determine the stiffness of soft tissue structures in the region of the first metatarsophalangeal joint during the interictal period and during exacerbation of gout [29]. The possibility of using tendon research techniques for scleroderma and ankylosing spondylitis is being actively studied. Our personal experience shows the possibility of determining the elasticity of hyaline cartilage of the knee joint, which can be used in dynamic assessment of the effectiveness of chondroprotective therapy, but requires further study (Fig. 3, 4).
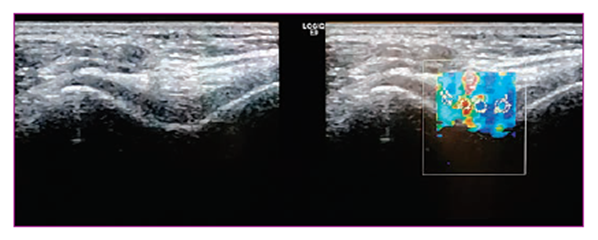 | Figure 3. Hyaline cartilage of a healthy person |
4. Conclusions
- Modern methods of ultrasound of joints, due to their speed, relatively low cost, absence of contraindications and high resolution, significantly expand the diagnostic and treatment capabilities of a rheumatologist and allow monitoring the effectiveness of therapy.Currently, ultrasound for the diagnosis of joint diseases is not yet widely used due to the small number of specialists proficient in this method, although in European countries and the USA ultrasound is an integral part of the examination of the musculoskeletal system. Sonoelastography may soon become firmly established in clinical practice as a first-line diagnostic method for identifying biomechanical changes in tendons, muscles, and ligaments, as well as assessing the effectiveness of treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML