-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1219-1221
doi:10.5923/j.ajmms.20241405.16
Received: Apr. 10, 2024; Accepted: May 3, 2024; Published: May 9, 2024

Comparative Characterization of Features of Clinical Manifestations of Helicobacter Associated Patients with Parkinson's Disease
Mansurova N. A., Majidova Ya. N., Nazarova J. A., Boymurodov R. R.
Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The pathogenesis of Parkinson's disease (PD) is based on the deposition of large protein complexes in brain neurons that are toxic to nerve cells. Studies show that the protein alpha synuclein found mainly in presynaptic terminals leads to the death of dopaminergic neurons in the brain. Patients with Parkinson's disease often complain of digestive problems years before the onset of motor disorders. Gastrointestinal dysfunction in PD is manifested by a variety of non-motor as well as motor symptoms, and every segment of the gastrointestinal tract is affected.
Keywords: Parkinson's disease, Helicobacter pylori, Levodopa, Movement disorders
Cite this paper: Mansurova N. A., Majidova Ya. N., Nazarova J. A., Boymurodov R. R., Comparative Characterization of Features of Clinical Manifestations of Helicobacter Associated Patients with Parkinson's Disease, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1219-1221. doi: 10.5923/j.ajmms.20241405.16.
Article Outline
- Helicobacter pylori (Helicobacter pylori, hereafter -HP) is one of the most common stomach infections and has long been associated with an increased risk of peptic ulcer formation and gastric cancer. However, recent studies have revealed a link between HP and many other diseases. Although the exact mechanism is unknown, HP may interfere with the absorption of some drugs. This article reports the results of a study on the prevalence of HP and its relationship with the clinical manifestations of Parkinson's disease.
1. Introduction
- Helicobacter pylori (H. pylori) is a gram-negative bacterium that has long been associated with an increased risk of peptic ulcer formation and gastric cancer. Recent studies, shows that gastritis caused by H. pylori increases the risk of developing Parkinson's disease [1]. Currently, there is insufficient evidence for the involvement of H. pylori in the pathophysiology of PD, although its presence may play a role in impaired drug absorption and H. pylori has a negative effect on ghrelin expression which leads to gastric hypokinesia and delayed passage of levodopa into the small intestine [2]. In addition, direct binding of levodopa by adhesin molecules from the bacterial surface as well as production of reactive oxygen species, decreased gastric acidity and gastric mucosal disruption in the presence of H. pylori may contribute to impaired levodopa absorption [3]. The aim of this study was to evaluate the prevalence of H. pylori infection in PD patients and to elucidate the relationship between infection and clinical status of PD.
2. Materials and Methods of the Study
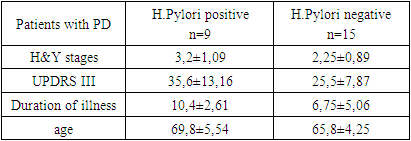
- We examined 36 patients with Parkinsonism. Among this contingent, 24 patients were with Parkinson's disease and 12 with vascular Parkinsonism, including 20 men and 16 women, mean age 67.4±4.98 years, disease duration from 2 to 22 years (9.3±1.42) years. Inclusion criteria for PD patients were as follows: PD diagnosed on the basis of the clinical diagnostic criteria of the Head Brain Bank of the UK PD Society [4], the severity of PD was assessed according to the Hen and Yahr scale.Patients with psychiatric disorders, gastric surgeries, prior intake of anti-H. pylori, history of antibiotic use within the last 6 months, or intake of antacids, H2-receptor antagonists, or proton pump inhibitors were not included. pylori, a history of antibiotic use within the last 6 months, or use of antacids, H2-receptor antagonists, proton pump inhibitors, domperidone, prokinetic drugs, or any drugs potentially affecting peristalsis and gastrointestinal integrity within the last 2 months.Data collection and evaluation. Data were collected through personal interviews and physical and neurological examinations. The Hen and Yahr stage and the motor portion of the Unified Parkinson's Disease Rating Scale (UPDRS)-III were used to assess the motor severity of PD.Urease Respiratory Test (URT). The urease breath test has been used for the presence of H.Pylori, which is based on the ability of urease to degrade urea to HC3- and NH4+. HC3- produces CO2, which, once in the bloodstream, is then transported to the lungs. UDT requires urea labeled with radioactive carbon 13C or 14C. Two background samples of exhaled air were taken in the study. The level of radioactive isotope in exhaled air is determined within 10-30 minutes. The tubes are then sent for mass spectrometry. The result is expressed as an increment of 13CO2 - δ13CO2, its excretion (‰) and is considered positive for values above 5‰.The data obtained in the study were subjected to statistical processing on a Mac personal computer using Microsoft Office Excel-16.13.1, Prism 7 software package including built-in statistical processing functions. Descriptive statistical values (mean ± standard deviation) were calculated for different continuous variables. Mann-Whitney U-test was used to evaluate differences in various parameters between H. pylori positive and negative groups. For all types of statistical analysis, differences were considered statistically significant at the achieved level of significance, p<0.05.
3. Results and Discussion
- We examined 36 patients, including 24 patients with idiopathic Parkinson's disease and 12 patients with vascular Parkinsonism, who constituted the control group. According to anamnesis data, the mean age of disease onset (the moment from which patients began to notice PD symptoms) was 59.1±5.28. According to the classification according to the severity of the disease, Hen and Yara found that patients with stage II - III (stage II 30.8% and stage III 30.7%) predominated significantly. The severity of motor symptoms was assessed by the UPDRS part III. The mean scores of the total severity score of motor manifestations was 29.4±7.96. Analyzing the results of H.Pylori prevalence showed that 37.5% of PD patients were found to be Helicobacter pylori positive compared to 8.3% of patients with vascular parkinsonism, p<0.05 (Figure 1).
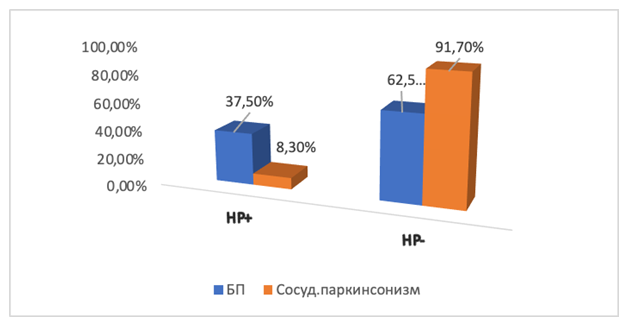 | Figure 1. Frequency of H.Pylori occurrence in the studied groups |
|
4. Conclusions
- The prevalence of HP infection is high among patients with PD. Various studies have shown that H.Pylori has a significant association with disease severity and duration. Thus, patients with PD should be screened for HP infection and eradication treatment can be applied in cases where HP positivity is found. The relationship between H.Pylori and PD should be further clarified by more comprehensive studies in the future.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML