-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1205-1207
doi:10.5923/j.ajmms.20241405.13
Received: Apr. 17, 2024; Accepted: May 6, 2024; Published: May 9, 2024

Human Papilloma Virus Detection Rate and Risk Factors in Males
Akhmedova Sh. Kh.1, Rakhimov R. A.1, Israilov Kh. T.2, Mannobzhonov P. B.3
1Research Institute of Virology of the Republican Specialized Scientific and Practical Center for Epidemiology, Microbiology, Infectious and Parasitic Diseases, Tashkent, Uzbekistan
2Republican Specialized Scientific and Practical Medical Center of Dermatovenereology and Cosmetology, Uzbekistan
3Master of the Tashkent Medical Academy in the Specialty “Bacteriology and Virology”, Uzbekistan
Correspondence to: Akhmedova Sh. Kh., Research Institute of Virology of the Republican Specialized Scientific and Practical Center for Epidemiology, Microbiology, Infectious and Parasitic Diseases, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

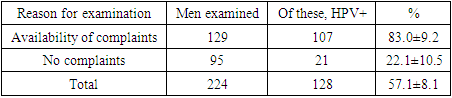
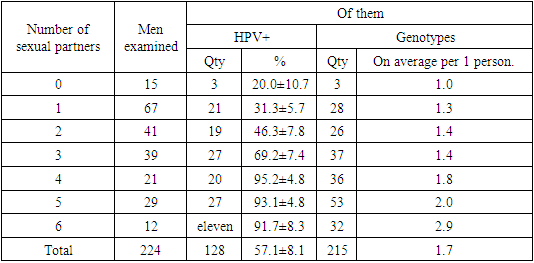
In Tashkent, smears from the ejaculate of 224 men were examined for the presence of genetic markers of HPV. The smears were examined using the AmliSens DNA Sorb AM test system to extract virus DNA. Quantitative determination of HPV DNA of 14 types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68) of high carcinogenic risk was carried out using the polymerase chain reaction method AmpliSens HPV HCR screen titer -14-FL.” To differentiate HPV HPV DNA of 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 genotypes in the collected material, the reagent “ AmpliSens HPV HCR genotype-titer-FL” (FBUN) was used Central Research Institute of Epidemiology of Rospotrebnadzor, Russian Federation). In 128 examined men (57.1±3.3%), genetic markers of HPV were identified. In men with complaints of itching and pain during urination, the frequency of HPV detection (83.0%) was 3.8 times higher (p <0.001) than in men who did not have such complaints (22.1%). Among all identified HPV genotypes, genotype 16 was dominant (21.4%). Viruses with an average level of distribution (18, 39, 66, 33, 68 genotypes) amounted to a total of 36.8%. Viruses of lower prevalence (35, 45, 51, 52, 56, 58 and 59 genotypes) accounted for a total of 41.8%. A total of 215 genotypes were identified. Of these, 50.8% have 1 strain, 32.8% have 2 strains, 14.8% have 3 strains and 1.6% have 4 strains. A direct strong correlation was identified between the number of sexual partners and the level of HPV infection (r=0.95), and the average number of HPV genotypes per 1 infected man (r=0.91).
Keywords: Human papillomavirus, Genotypes, Men
Cite this paper: Akhmedova Sh. Kh., Rakhimov R. A., Israilov Kh. T., Mannobzhonov P. B., Human Papilloma Virus Detection Rate and Risk Factors in Males, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1205-1207. doi: 10.5923/j.ajmms.20241405.13.
Article Outline
1. Actuality
- In recent years, the main focus of researchers has been on studying the prevalence and prevention of HPV in women [2,3,5,8]. In many countries of the world, including Uzbekistan, a high level of HPV prevalence has been revealed [1,4]. However, HPV is not sex-selective. Therefore, both women and men must participate in the process of spreading HPV. Moreover, the prevalence of sexual transmission of HPV has been proven [6,7].
2. Objective
- Determination of the level of HPV prevalence in males and identification of risk factors.
3. Methods And Techniques
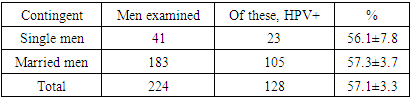
- In Tashkent, on conditions of anonymity and voluntary participation, 41 single men, aged 17-29 years, and 183 married men, aged 23-68 years, were interviewed and examined, a total of 224 men. Of these, 129 people. (57.6%) contacted the anonymous office of the Republican Specialized Scientific and Practical Medical Center of Dermatology and Venereology with complaints of itching and pain when urinating (suspicion of a genitourinary infection). The remaining 95 people. (42.4%) were examined for other reasons not related to complaints of damage to the genitourinary system. The survey was conducted to establish details of sexual life and identify possible risk factors for HPV infection. All men had urethral swabs screened for the presence of genetic markers of HPV. The smears were examined in the reference laboratory of the Research Institute of Virology of the Republican Specialized Scientific and Practical Medical Center for Epidemiology, Microbiology, Infectious and Parasitic Diseases of the Ministry of Health of the Republic of Uzbekistan , using the “ AmliSens ” “DNA Sorb AM” test system to extract viral DNA. Quantitative determination of HPV DNA of 14 types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68) of high carcinogenic risk was carried out using the polymerase chain reaction method "AmpliSens HPV HCR screen titer -14- FL". To differentiate HPV HPV DNA of 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 genotypes in the collected material, the reagent “ AmpliSens HPV HCR genotype-titer- FL” (FBUN) was used Central Research Institute of Epidemiology of Rospotrebnadzor, Russian Federation) [4,8].
4. Results and Discussion
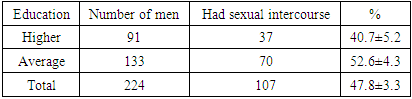
- The survey found that of all the men surveyed, 107 had premarital sexual relations. (47.8±3.3%). A tendency (p>0.5) was revealed for men with secondary education to have more frequent sexual relations before marriage (1.3 times more often) compared to men with higher education (Table 1).
|
|
|
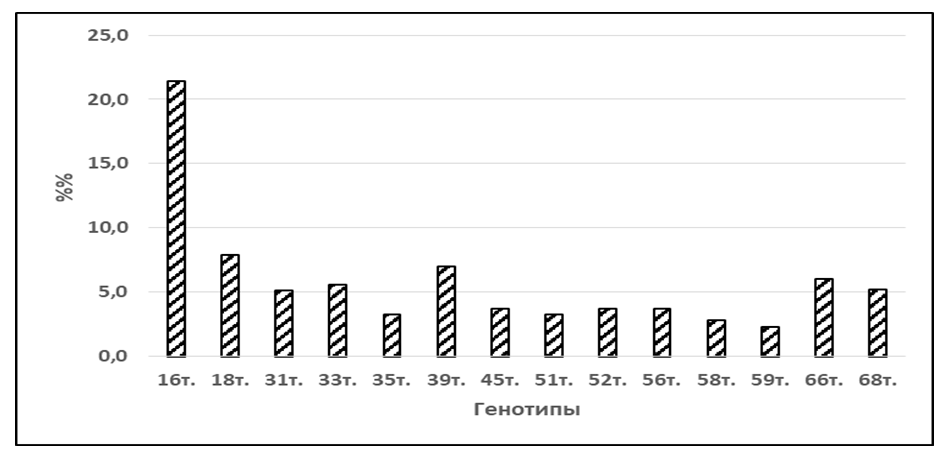 | Figure 1. Frequency of detection of HPV genotypes in men |
|
5. Conclusions
- 1. It has been shown that in Uzbekistan there is a high risk of infection of men with 14 HPV genotypes of high oncogenic risk.2. A significantly higher rate of HPV infection was found in men with symptoms of urethral irritation.3. A high level of infection and an active sexual lifestyle determines men as a significant source of the spread of HPV.4. Measures to reduce the prevalence of HPV in men should be an integral part of HPV prevention measures in the country.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML