-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1200-1204
doi:10.5923/j.ajmms.20241405.12
Received: Apr. 9, 2024; Accepted: May 6, 2024; Published: May 9, 2024

Influence of Thyroid Function on Lipid Profile in Autoimmune Thyroiditis: Clinical and Experimental Insights
Najmutdinova D. K.1, Nasirova A. K.1, Rasulov A. D.2
1Endocrinology, Department of Internal Diseases №2, Tashkent Medical Academy, Tashkent, Uzbekistan
2Anesthesiology and Resuscitation, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Rasulov A. D., Anesthesiology and Resuscitation, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

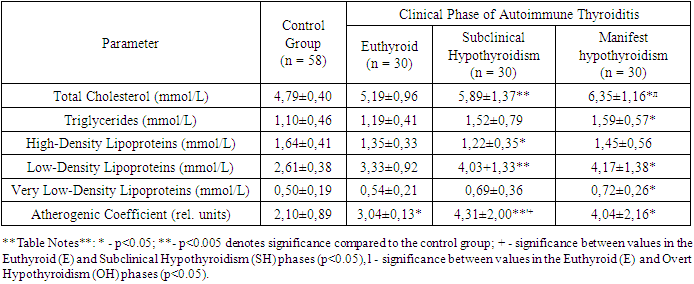
Autoimmune thyroiditis (AIT) is a chronic disorder characterized by gradual onset, nonspecific early symptoms, and slow progression involving destructive processes in the thyroid gland. AIT ranks among the most prevalent thyroid diseases, contributing to 20-50% of thyroid pathology cases. Despite extensive data on thyroid tissue antibody prevalence and hypothyroidism frequency, AIT affects 3-20% of the global population, constituting 70-80% of primary hypothyroidism instances. Hypothyroidism is recognized as an atherogenesis initiator due to significantly elevated cholesterol levels, impeding lipid oxidation, transportation, and elimination, thereby accelerating atherosclerosis. The lipid profile alterations, including increased low-density lipoprotein cholesterol (LDL-C) and triglycerides (TG), along with decreased high-density lipoprotein cholesterol (HDL-C), exacerbate atherogenicity. L-thyroxine therapy in subclinical hypothyroidism mitigates atherogenic lipid changes. Thyroxine levels profoundly impact serum cholesterol and bone mineral density, potentially inhibiting atherosclerosis progression. Dyslipidemia in hypothyroidism involves reduced lipid breakdown, transportation, and bile excretion, alongside diminished LDL receptor quantity and activity. Hypercholesterolemia in hypothyroidism often remains refractory to conventional lipid-lowering therapies but improves with thyroid hormone supplementation. The lipid profile in primary hypothyroidism leans towards atherogenicity, accentuated in severe thyroid hormone deficiency, while anti-atherogenic lipid fractions remain relatively unaffected. Our study aimed to explore the influence of thyroid function on the lipid profile. Evaluating 73 AIT patients' blood samples and 58 healthy donors, we observed elevated thyroid-stimulating hormone levels in manifest and subclinical hypothyroidism phases. Lipid profile analysis revealed significant increases in total cholesterol and triglycerides, along with decreased HDL-C, particularly in overt hypothyroidism. LDL-C levels rose markedly across AIT phases, exacerbating atherogenicity, with overt hypothyroidism displaying the most pronounced effects. Our findings underscore the atherogenic nature of the lipid profile in hypothyroidism, especially in its overt phase, highlighting the importance of thyroid function assessment in managing dyslipidemia and cardiovascular risk in AIT patients.
Keywords: Autoimmune thyroiditis, Hypothyroidism, Lipid profile, Cholesterol, Triglycerides, LDL-C, HDL-C
Cite this paper: Najmutdinova D. K., Nasirova A. K., Rasulov A. D., Influence of Thyroid Function on Lipid Profile in Autoimmune Thyroiditis: Clinical and Experimental Insights, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1200-1204. doi: 10.5923/j.ajmms.20241405.12.
1. Introduction
- AIT (Autoimmune thyroiditis) is a chronic disease with a gradual onset, nonspecific early signs, and slow progression with increasing destructive processes in the thyroid gland. AIT is one of the most common thyroid diseases, accounting for 20 to 50% of thyroid pathology [1]. There is extensive information available on the prevalence of thyroid tissue antibody carriage and the frequency of hypothyroidism in the population. However, according to available data, 3 to 20% of the world's population currently suffers from AIT, which accounts for 70-80% of all cases of primary hypothyroidism [3,5]. In various countries, AIT is encountered with a frequency of 0.1 to 1.2% in children and 6 to 11% among the adult population [3,5,6].According to numerous clinical and experimental studies, hypothyroidism is widely recognized as one of the initiators of atherogenesis, as it has been established that a deficiency of thyroid hormones significantly increases cholesterol levels [2,18,21,23,26]. Additionally, its oxidation slows down, transportation and elimination of triglycerides, low-density lipoproteins (LDL), and very-low-density lipoproteins (VLDL) worsen. Decreased elimination of atherogenic lipids leads to an increase in the atherogenicity coefficient and accelerated development of atherosclerosis, the clinical manifestations of which become predominant and create specific challenges in diagnosing thyroid gland hypofunction [4,9,10].For instance, some authors have presented results of a comparative assessment of the level of lipoprotein A in plasma in patients with hypothyroidism, hyperthyroidism, and euthyroid individuals. According to the researchers, the level of lipoprotein A in patients with hyperthyroidism and euthyroid individuals did not significantly differ. However, a significant decrease in the plasma level of lipoprotein A compared to patients with hyperthyroidism was found in patients with hypothyroidism. Individual analysis of the study results revealed that the level of lipoprotein A exceeding 30 mg/dL was registered in 37.5% of cases in patients with hypothyroidism, in 13.6% of patients with hyperthyroidism, and in 15.3% of euthyroid individuals. Compared to lipid metabolism indicators in euthyroid individuals, patients with hypothyroidism showed decreased levels of high-density lipoprotein cholesterol (HDL-C) and increased levels of total cholesterol, low-density lipoprotein cholesterol (LDL-C), and apolipoprotein B (apoB). In patients with hyperthyroidism, compared to euthyroidism, a decreased level of LDL-C and increased levels of HDL-C and apolipoprotein AI (apoAI) were determined.The influence of L-thyroxine on the levels of various lipoproteins in long-standing subclinical hypothyroidism was also studied. Before treatment, researchers found significantly higher levels of triglycerides, LDL-C, apoB, and lipoprotein A in all patients, correlating with TSH levels. After 6 months of L-thyroxine therapy, only triglyceride and LDL-C levels among all lipid metabolism parameters studied were decreased. Based on the obtained results, it was concluded that atherogenic changes in the lipid profile in subclinical hypothyroidism undergo reversal during L-thyroxine replacement therapy.In the opinion of several researchers, the main factor determining the level of serum cholesterol and bone mineral density is the level of T4. Adequate replacement therapy with thyroid hormones leads to normalization of the average values of basic lipid metabolism indicators, which may contribute to the inhibition of atherosclerosis progression [24,27,28,31].During the studies, an elevated level of low-density lipoprotein cholesterol (LDL-C) and triglycerides (TG) in the blood serum of patients with decreased thyroid function was also identified. Researchers note that the level of high-density lipoproteins (HDL) in these patients remains unchanged or decreases. According to the authors, the mechanism underlying hypercholesterolemia in hypothyroidism involves a decrease in the rate of synthesis and particularly the breakdown of lipids, deterioration of their transportation and excretion with bile, and a decrease in the quantity and activity of LDL receptors.According to some data, in patients with hypothyroidism, the cholesterol level remains elevated despite adequate replacement therapy, necessitating the prescription of a hypocholesterolemic diet alongside hypocholesterolemic therapy. Additionally, M.D. Dáñese et al. argue that hypercholesterolemia detected in hypothyroidism is not responsive to treatment with diet, statins, and other lipid-lowering agents but is effectively corrected only by thyroid hormone preparations.The results of a comparative assessment of the blood lipid spectrum in patients suffering from primary hypothyroidism of varying severity compared to patients with autoimmune thyroiditis and euthyroid individuals are presented in a study by Yu.N. Grishkin et al. According to the researchers, the lipid profile in patients with primary hypothyroidism becomes atherogenic in conditions of pronounced thyroid hormone deficiency, while the concentration of anti-atherogenic lipid fractions remains unchanged.Numerous foreign studies have shown that a 7% decrease in LDL-C levels allows for a 15% reduction in the risk of developing coronary heart disease (CHD). The results of a meta-analysis of several multicenter studies on the effectiveness of secondary prevention of CHD using lipid-lowering agents indicate that the progression of the atherosclerotic process stops when LDL-C levels are reduced by 44%. An increase in TSH levels by 1 mIU/L is accompanied by an increase in total cholesterol levels by 0.09 mmol/L in women and by 0.62 mmol/L in men. However, researchers did not find a significant correlation between TSH levels and LDL-C, indicating the development of hyperlipidemia in the examined patients due to causes other than hypothyroidism [29].Novitskaya A.B. (2004) studied the level of lipid peroxidation activity and the state of the body's antioxidant defense system in patients with various phases of autoimmune thyroiditis. According to the author, the level of lipid peroxidation and antioxidant system activity in autoimmune thyroiditis during the euthyroid phase is not significantly disturbed. In patients with autoimmune thyroiditis during the subclinical hypothyroidism phase, activation of free radical oxidation, depletion of the body's antioxidant defense, and accumulation of lipid peroxidation intermediates are registered. Thus, the severity of lipid peroxidation changes in autoimmune thyroiditis is closely related to the degree of thyroid dysfunction.Alongside dyslipidemia and disturbances in central and intracardiac hemodynamics in hypothyroidism, abnormalities in the thrombotic-vascular and coagulation links of the hemostasis system and blood fibrinolytic activity have been detected. Most researchers have found an increase in the level and activity of plasminogen activator inhibitor, platelet aggregation activity, and a high concentration of activated factor VII in patients with hypothyroidism. It is believed that fibrinolytic activity in hypothyroidism is usually somewhat increased. Nevertheless, some researchers have obtained opposite results, indicating a lack of consensus on changes in blood fibrinolytic activity in hypothyroidism.
2. Materials and Methods
- The study used samples of venous blood from 73 patients with autoimmune thyroiditis and 58 healthy donors, constituting the control group. The level of total cholesterol (TC), high-density lipoproteins (HDL), low-density lipoproteins (LDL), very-low-density lipoproteins (VLDL), the atherogenic coefficient, and triglycerides (TG) in the blood serum were determined by an enzymatic method using a Mindray autoanalyzer (China) with reagents from "Human" company (Germany). Reagents from the same company were used as control material.
3. Results and Discussions
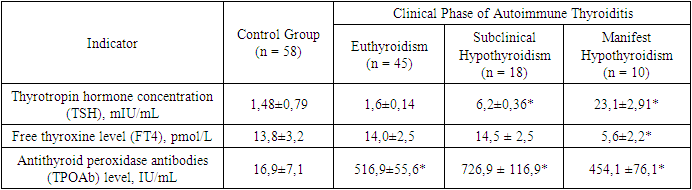
- The evaluation of thyroid gland hormonal activity and the level of antibodies to thyroperoxidase in the study groups are presented in Table 1.
|
|
4. Conclusions
- Thus, the lipid profile in patients with subclinical and overt hypothyroidism exhibits an atherogenic nature, most pronounced in the overt phase of the disease. Meanwhile, the level of anti-atherogenic lipid fraction in the analyzed groups of AIT patients did not significantly differ from that of healthy individuals. Our findings are consistent with data from the majority of domestic and foreign researchers [2,18,23,26].
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML