-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1187-1191
doi:10.5923/j.ajmms.20241405.09
Received: Apr. 15, 2024; Accepted: May 3, 2024; Published: May 7, 2024

Methods of Diagnostics of Precancer Diseases of the Cervic Associated with Papillomavirus
Navruzova Nilufar Orzijonovna
Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan
Correspondence to: Navruzova Nilufar Orzijonovna, Bukhara State Medical Institute named after Abu Ali ibn Sina, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

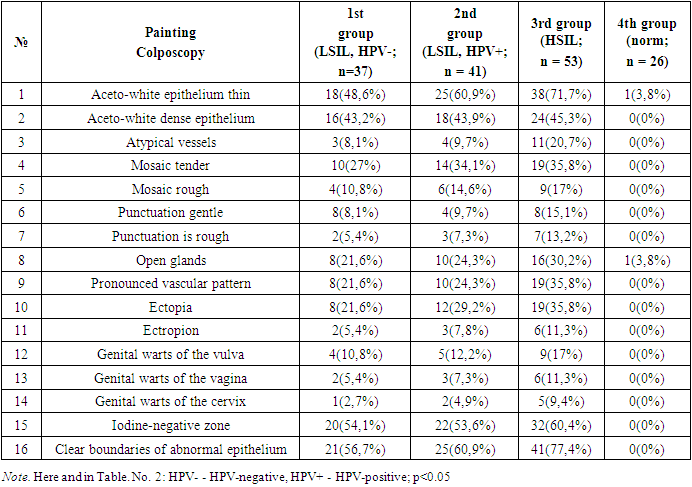
In accordance with the results of cytological examination and testing for HPV, all examined patients were divided into 3 groups: the 1st group consisted of 37 HPV-negative patients with LSIL, the 2nd group included 41 HPV-positive patients with LSIL, the 3rd group consisted of 53 patients with a cytologically confirmed diagnosis of HSIL, all patients in this group were HPV-positive. The control group included 26 women with a visually unchanged cervix and the absence of HPV according to real-time PCR, who applied to the antenatal clinic for a preventive examination. The patients of the main and control groups included in the study were comparable in age and parity.
Keywords: Precancerous diseases of the cervix, Diagnostics, Colposcopy, Pap test, HPV
Cite this paper: Navruzova Nilufar Orzijonovna, Methods of Diagnostics of Precancer Diseases of the Cervic Associated with Papillomavirus, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1187-1191. doi: 10.5923/j.ajmms.20241405.09.
1. Introduction
- Diseases of the cervix, especially precancerous are one of the most common pathological conditions of the reproductive system in women of reproductive age. Despite the widespread use of screening programs, cervical cancer (CC) still occupies a leading position among the causes of death from oncological diseases of the female genital organs [1,5,9].The World Health Organization has recognized the oncological danger of highly oncogenic human papillomaviruses (HPV) and its leading role in the etiology of cervical cancer (CC). As is known, the viral genome transforms cervical epithelial cells and leads to the development of cervical dysplasia of varying severity (cervical intraepithelial neoplasia - CIN II–III) and cervical cancer. With invasive cervical cancer, HPV is detected in 95% of cases [2,7,11].Human papillomaviruses (HPV) are sexually transmitted and often found in young people. They are usually neutralized by the immune system. However, prolonged presence of high-risk HPV (HR) can lead to the development of abnormal cells in the cervix; this condition is considered precancerous if the surface layer of the cervix is affected by at least two-thirds. After a few years, precancer can turn into cervical cancer. Not all people with precancerous conditions develop cervical cancer, but it is difficult to predict who will develop it. There are a number of different HPV-BPs that can cause precancer and cervical cancer. The most significant high-risk HPVs are HPV16 and 18 as they are responsible for approximately 70% of cervical cancers worldwide. Preventive vaccination by intramuscular injection of virus-like particles triggers the formation of antibodies that protect against future HPV infections. The human papillomavirus (HPV) is one of the common viruses that can cause about 6 different types of cancer later in life. Cancer can develop years, sometimes decades, after a person is infected with HPV [3,12,17].The risk of HPV infection exists at any age, but the most frequent infection is typical for young women and especially adolescents (20%). The frequency of infection in women aged 45–55 years is 5%. In 80–90% of cases, human papillomavirus infection (PVI) spontaneously regresses, however, in 10–20% of cases, HPV persists for a long time and the risk of developing HPV-associated diseases increases [4,10,21].HPV-associated diseases include precancerous and malignant tumors of the cervix, vulva, vagina and anus, oral cavity and larynx, recurrent respiratory papillomatosis, and anogenital warts [6,13,20].Cases of HPV-associated cancers have increased. Thus, cancer of the vulva and vagina accounts for 5% of all gynecological cancers (40 thousand cases per year), anal cancer - 100 thousand cases annually (40 thousand in men and 60 thousand in women). It has now been proven that anal neoplasias (anal intraepithelial neoplasia - AIN), as well as cervical neoplasias (CIN), are strongly associated with HPV infection [23,25]. Thus, in 23.3% of patients with morphologically verified CIN, AINs of varying severity were identified [8,15,19]. There is an increase in HPV-related extragenital pathology, in particular, recurrent respiratory papillomatosis (HPV 6, type 11), squamous cell lung cancer (type 6, 11, 16, 18), laryngeal cancer (type 16, 18), focal hyperplasia of the epithelium (type 13, 32), conjunctival papillomas (type 6, 11), oral warts (type 2, 4), oral condylomas (type 6, 11), red papillomatosis of the oral cavity (6, 11th type). It should be noted that 15–20% of all cancers of the oral cavity and pharynx are caused by HPV. For all the listed lesions caused by HPV infection, a single screening was developed only for the cervix [14,16,18].Screening is a system of primary examination of groups of clinically asymptomatic individuals in order to identify cases of the disease. Unlike the cervix, screening has not been developed to detect the pathology of the vulva, vagina, anus, and extragenital pathology. The principles of examination of patients with pathology of the cervix are aimed at diagnosing changes in the epithelium of the cervix, which are caused by HPV.Goal: To reveal the prevalence of precancerous diseases of the cervix associated with papillomaviruses in women who applied to a gynecologist, and to evaluate the diagnostic capabilities of laboratory and cytological methods.
2. Methods
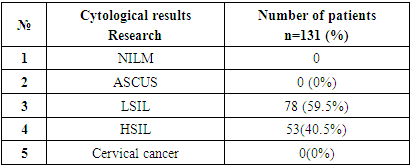
- Conducted clinical and laboratory examination of 131 patients with diseases of the cervix. All patients underwent the necessary diagnostic standard: examination of the cervix in the mirrors, cytological examination of smears from ecto- and endocervix, polymerase chain reaction (PCR) for HPV, pH-metry, extended colposcopy of the cervix. Material for the study of vaginal microbiocenosis was collected from the posterolateral wall of the vagina, for the detection of HPV - from the cervical canal. The scrapings were placed in an Eppendorf tube containing 1 ml of physiological saline, the material was stored and transported in accordance with the current regulatory documents. DNA was isolated using a set of reagents PROBA-GS (“Standard diagnostics”, Bukhara). The study was carried out by PCR with real-time detection of results (RT-PCR) using HPV reagents (“Diagnostic Standard”, Bukhara) in a detecting amplifier DT-96, according to the manufacturer’s instructions, in the laboratory (“Diagnostic Standard”, Bukhara).The possibilities of the HPV test in Uzbekistan currently include the determination of 2 types of HPV - 16, 18 (polymerase chain reaction method - PCR); qualitative and quantitative determination of HPV type 21 by real-time PCR [16, 18, 26, 31, 33, 35, 39, 44 (55), 45, 51, 52, 53, 56, 58, 59, 66, 68, 82, 6, 11]; identification of high-risk HPV; quantitative determination of HPV types included in the Digene test (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 6, 11th).Cytological examination of smears (PAP-test) has until now been the basis of screening programs aimed at the early detection of HPV-associated precancer and cancer. A decrease in mortality by 20–60% was achieved due to the introduction of state screening programs (1960–2000s) based on the PAP test in Europe and North America [9].According to the WHO, about 600,000 cases of cervical cancer are registered annually in the world and, despite ongoing therapeutic measures, the mortality rate is 45-50%. With the advent of the polymerase chain reaction (PCR) and cytological studies (PAP test) in the arsenal of diagnostic methods, the detection of the virus in urogenital samples has become extremely simplified. PCR makes it possible not only to detect virus DNA with high sensitivity, but also to determine its type, which is extremely important in predicting the disease, while liquid cytology more accurately determines the degree of cell damage.The obvious advantages of the HPV test include its high sensitivity, the ability to assess the further risk of progression of the process, its use in a group of women vaccinated against HPV, etc. The real-time PCR method allows to determine the amount of DNA of clinically significant types of HPV bv in the sample, in contrast to conventional PCR.The visual method is an alternative to cytology in cases where it is not feasible. Assessment of the condition of the epithelium of the vagina and cervix can be performed visually using samples with 3-5% acetic acid and Lugol's solution. Its sensitivity and specificity are 69–72%. Can be used by well trained medical staff in the absence of a colposcope.It should be emphasized that there are no specific colposcopic signs of HPV lesions of the cervical epithelium, indirect signs are acetowhite epithelium, puncture, mosaic, the severity of which depends on the severity of the process.Analysis of the results of extended colposcopy was carried out in 131 women with precancerous cervical pathology and 26 - the control group of conditionally healthy women. All patients underwent a cytological examination (PAP test), smear microscopy, and HPV testing for highly oncogenic types. All patients underwent a cytological examination (PAP test), smear microscopy, and HPV testing for highly oncogenic types. The effectiveness of the colposcopy method was evaluated according to the criteria of sensitivity and specificity.
3. Results and Discussion
- In accordance with the results of cytological examination and testing for HPV, all examined patients were divided into 3 groups: the 1st group consisted of 37 HPV-negative patients with LSIL, the 2nd group included 41 HPV-positive patients with LSIL, the 3rd group consisted of 53 patients with a cytologically confirmed diagnosis of HSIL, all patients in this group were HPV-positive. The control group included 26 women with a visually unchanged cervix and the absence of HPV according to real-time PCR, who applied to the antenatal clinic for a preventive examination. The patients of the main and control groups included in the study were comparable in age and parity.The results of the studies showed that a normal cytological picture in smears from exo- and endocervix was found in the control group in all women (100.0%). The smears were represented by the cells of the upper layers of the stratified squamous epithelium (SSE) - superficial and intermediate. The nuclear-cytoplasmic ratio was evaluated, i.e. Normally, the nucleus was small, round with a normal chromatin structure, the cytoplasm was large. The background of the smear also consisted of colonies of bacteria in the form of sticks – Lactobacillus.
|
|
4. Conclusions
- Thus, early detection (screening) of HPV-related diseases and a rational approach to patient management using evidence-based diagnostic methods can prevent oncological diseases.As a result of the study, it was found that the severity of colposcopic changes in the cervical epithelium (AWE, AWE with mosaic/puncture) significantly correlates with cytological changes in LSIL and HSIL. Signs such as coarse mosaic/punctuation were significantly more common in patients with severe squamous intraepithelial lesions (HSIL) of the cervix. It was also found that with pronounced colposcopic changes, highly oncogenic HPV genotypes were detected significantly more often. In the presence of colposcopic signs such as AWE and AWE with mosaic/puncture, HPV genotype 16 dominated.Based on the results of our study, the importance of performing extended colposcopy, along with fluid cytology and HPV testing, is important for the early diagnosis of cervical SIL.
ACKNOWLEDGEMENTS
- The authors are grateful for the support and helpful comments provided by the department of Obstetrics and gynekology in Bukhara State Medical Institute, as well as other experts consulted as part of the process. We would also like to thank Bukhara city maternity complex for her assistance in creating the figure for our literature search.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML