-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1178-1181
doi:10.5923/j.ajmms.20241405.07
Received: Apr. 11, 2024; Accepted: May 3, 2024; Published: May 7, 2024

Minor Invasive Treatment of Metastatic Spinal Tumors with Radiofrequency Ablation
Khamrokulov Bekzod Bahodirovich1, Polatova Djamilya Shogayratovna2, Alimov Ijod Rustamjonovich3
1Basic Doctoral Student, Department of Neurosurgery, Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
2Doctor of Medical Sciences, Head of the Department of Oncology and Medical Radiology, Tashkent Dental Institute, Tashkent, Uzbekistan
3Doctor of Philosophy in Medical Sciences, Docent of the Department of Neurosurgery, Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
Correspondence to: Khamrokulov Bekzod Bahodirovich, Basic Doctoral Student, Department of Neurosurgery, Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

According to the literature, malignant neoplasms are one of the leading causes of death in people under 65 years of age. The incidence of bone metastases in cancer patients is high. Thus, out of 1000 post-mortem examinations performed on patients who died from malignant tumors, bone metastases are detected in 25-30% of cases, the most common localization of malignant metastases in the bone of the skeleton is the spine (65%). The main clinical manifestations of spinal metastases are pain, pathological fractures of the vertebral bodies, compression of the spinal cord/nerve roots. These symptoms significantly reduce the quality of life of this category of patients. The main reasons for a decrease in the quality of life of patients with metastatic spinal lesions are severe pain syndrome and impaired motor activity. The most serious complication of spinal metastases is spinal cord compression with the development of paresis/plegia. Such a complication occurs in 5% - 10% of all patients with oncological disease Metastatic lesions of the bones of the spine, sharply worsen the quality of life of patients, taking into account the pronounced pain syndrome and gross neurological disorders. In some cases, radical treatment of multiple spinal metastases is not successful, respectively, there is a need to provide assistance by relieving pain syndrome and improving the quality of life of patients. Thus, surgical treatment of metastatic spinal lesions in order to improve the quality of life of patients requires minor surgical intervention, including adequate anesthesia, less surgical aggression and early rehabilitation of patients.
Keywords: Corporectomy, Vertebrectomy, Malignant neoplasms, Cancer patients, Localization of malignant metastases, Tumour
Cite this paper: Khamrokulov Bekzod Bahodirovich, Polatova Djamilya Shogayratovna, Alimov Ijod Rustamjonovich, Minor Invasive Treatment of Metastatic Spinal Tumors with Radiofrequency Ablation, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1178-1181. doi: 10.5923/j.ajmms.20241405.07.
1. Introduction
- In terms of the frequency of metastasis of malignant tumours, skeletal bones rank third, after the liver and lungs, [2,3]. The spine is one of the main localisations of bone metastases. According to some authors, the frequency of its lesions can reach 70%. Primary benign and malignant tumours of the spine are diagnosed in 1-3%, and metastatic tumours - in 96% of patients [1,4]. The most common types of tumours that metastasize to the spine are breast, lung and prostate cancers [5,6]. The underlying problem of tumour metastasis to the spine is a pronounced pain syndrome due to tumour compression of nerve roots, or a pathological fracture of the vertebral body with the development of compression and pain syndrome of varying severity and, as a consequence, a significant reduction in the quality of life [7,8]. Most often, patients with metastatic spinal lesions are bedridden and receive only symptomatic treatment.Surgical treatment for tumour lesions of the spine is possible both in "radical" volume in case of solitary lesions, when the entire affected segment of the spinal column is removed (corporectomy, vertebrectomy) and various types of reconstruction and stabilisation are performed, and for palliative purposes (decompressive laminectomy, vertebro-, kyphoplasty) in case of multiple metastatic lesions.Given the prevalence of the metastatic process in the spinal column with multiple metastases, it is not always possible to carry out radical surgical treatment, so doctors implement various options of palliative treatment and symptomatic therapy. In this article, we wanted to give our experience with palliative treatments for surgical management of patients with metastatic spinal lesions.The aim of the study is to improve the quality of life of patients with metastatic spinal lesions by applying palliative treatment methods.
2. Material and Methods
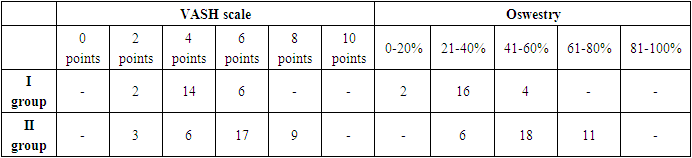
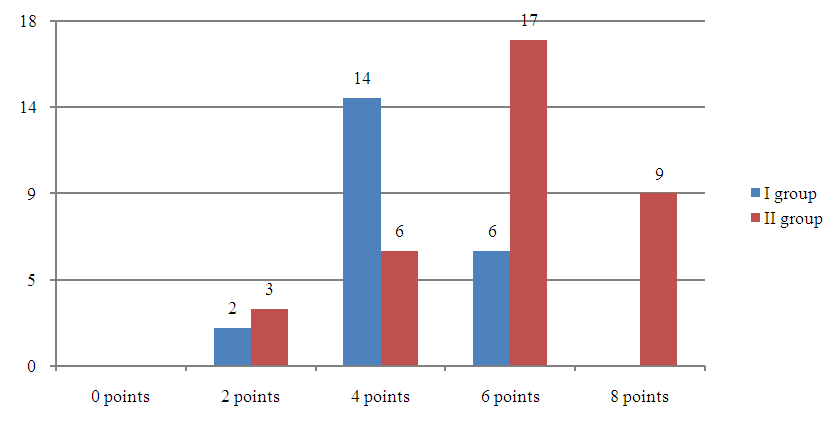
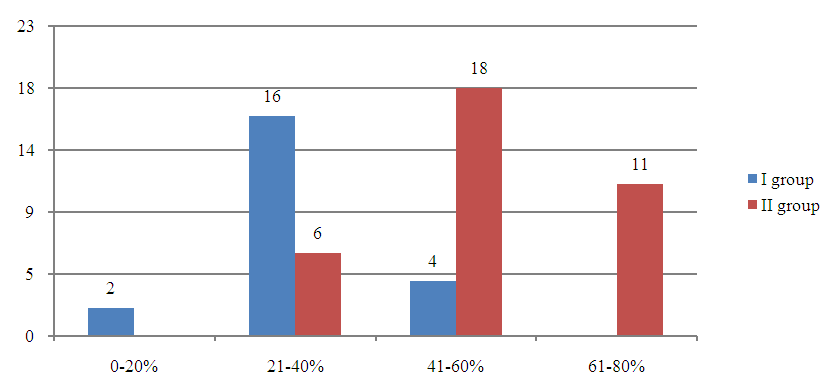
- The material is based on the selection of case histories of 35 patients treated at RSNPMCN from 2019 to 2020, who constituted the control (II) group of the study and 22 patients treated at Nano Medical Clinic from 2020 to 2022, who constituted the main (I) group of patients selected for the study. Out of them 38 (67%) were males and 19 (33%) were females. The age of the patients ranged from 48 to 65 years. The average age of the patients was 56.5 years.As diagnostic measures, in addition to general clinical and laboratory investigations, the patients underwent intrumental examination methods such as spondylogram, MRI, MSCT, skeletal bone scintigraphy, as well as all necessary diagnostic options for oncology search in the body.Among the topical location of the pathological process in the spine, isolated and multiple vertebral lesions were detected. There were 12 patients with isolated vertebral lesions and 45 patients with multiple vertebral lesions. Among the patients with isolated lesions, in 3 (25%) patients the pathological process was located in the cervical spine, in 2 (17%) patients in the thoracic spine, and in 7 (58%) patients in the lumbosacral spine. Among 45 patients with multiple spinal lesions, 7 (15%) patients had lesions in the cervical and thoracic spine, 18 (50%) patients had lesions in the thoracic and lumbar spine, 9 (21%) patients had lesions in the cervical and lumbosacral spine, and 11 (24%) patients had lesions in the cervical, thoracic, and lumbosacral spine. In 22 (49%) patients with multiple vertebral lesions, the pathological process was detected in other parts of the bone skeleton by scintigraphy in the form of metastases.In all studied patients in both groups, vertebral lesions were limited to the vertebral body without destruction of the vertebral walls.In all patients, the main clinical sign of the disease was severe pain in the spine and restriction of movements according to the localisation of the pathological process.The dynamics of pain syndrome was assessed according to the VAS scale, and the quality of life according to the Oswestry questionnaire. At the same time, the pre-treatment parameters (Table 1).
|
 | Diagram 1. In the majority of the studied patients (in group I - 59%, in group II - 51%) pain syndrome according to VAS reached 8 points |
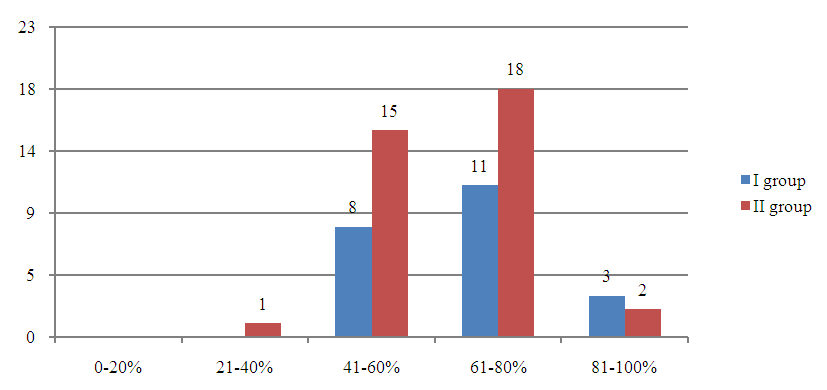 | Diagram 2. In the majority of the studied patients (in group I - 50%, in group II - 51%) the reduction of the quality of life according to Oswestry corresponded to 61-80% |
|
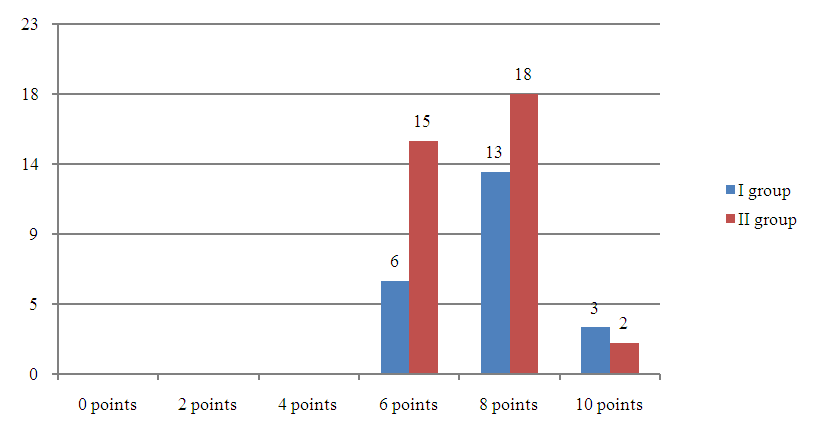
3. Conclusions
- Using the application of the method of percutaneous vertebroplasty with the combination of radiofrequency ablation of sympathetic branches of nerve roots of the affected spinal segment by a metastatic tumour, a significant reduction in pain syndrome and improvement in the quality of the remaining life of patients can be achieved.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML