-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1136-1139
doi:10.5923/j.ajmms.20241404.69
Received: Apr. 12, 2024; Accepted: Apr. 27, 2024; Published: Apr. 30, 2024

Results of Subepithelial Vascularized Palatal Flap with Simultaneous Use of PRF for Repair of Maxillary Sinus Perforation
Sh. A. Boymuradov, D. R. Ruziboev
Tashkent Medical Academy, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic odontogenic maxillary sinusitis (hereinafter referred to as COMS) is an inflammatory disease of the mucous membrane of the maxillary sinus caused by odontogenic infection and is a widespread disease. According to several authors, chronic forms of rhinosinusitis in Russia affect about 15% of the population. Epidemiological studies conducted in more than 30 countries indicate a 3-fold increase in the incidence of sinusitis over the past decades. At the same time, an increase in their frequency was noted, increasing by 1.5–2% annually. Data from the National Ambulatory Medical Care Survey (NAMCS) in the United States demonstrate that sinusitis is the fifth most common diagnosis for which antimicrobials are prescribed. In addition, it is known that as part of the 2008 National Health Survey carried out in the United States, it was found that one in 7 people (13.4%) over the age of 18 years had sinusitis during the previous calendar year, while the incidence in adults females were 1.9 times higher than males, 21 and the group of patients aged 45 to 74 years was most susceptible to the disease.
Keywords: Odontogenic maxillary sinusitis, Rhinosinusitis, Tooth extraction
Cite this paper: Sh. A. Boymuradov, D. R. Ruziboev, Results of Subepithelial Vascularized Palatal Flap with Simultaneous Use of PRF for Repair of Maxillary Sinus Perforation, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1136-1139. doi: 10.5923/j.ajmms.20241404.69.
1. Introduction
- Odontogenic maxillary sinusitis (OMS) is an inflammatory disease of the mucous membrane of the maxillary sinus (MS) caused by an odontogenic infection. FSHD is a widespread disease [3].The polyetiology, diversity and high prevalence of inflammatory processes of the paranasal sinuses, and in particular the maxillary sinuses [2,5-9] is the basis for active research and discussion of this issue. The need for adequate, joint work of doctors of various specialties - otorhinolaryngologists, maxillofacial surgeons and dentists is justified by the difficulty in diagnosing and treating odontogenic maxillary sinusitis [10].Sinusitis of odontogenic etiology accounts for 26 to 40% of all inflammatory diseases of the maxillary sinus [7]. In recent years, there has been a noticeable increase in cases of hospitalization of patients with inflammatory diseases of the maxillary sinuses, often provoked by odontogenic causes [11,12]. One of the reasons for the development of this inflammatory pathological process is defects in the bottom of the maxillary sinuses, initiated by tooth extraction - from 41.2 to 91.7% [13].Odontogenic maxillary sinusitis, complicated by the presence of oroantral communications, is the most difficult form of odontogenic maxillary sinusitis from a treatment point of view [9]. This is explained by the fact that the oroantral communication “unites” the upper jaw with the oral cavity, which leads to a gross disruption of the architectonics and functioning of these 7 structures, necessitating the elimination of the formed communication. First of all, the perforation hole serves as a route of invasion into the sinus cavity of microorganisms with anaerobic and anaerobic types of respiration [14]. Contamination of the maxillary sinuses with flora that is not typical for this anatomical formation causes an immune response with the development of an inflammatory process with all subsequent clinical manifestations. In the absence of adequate therapy, this leads to chronicity of the maxillary sinus, long-term nasal breathing disorder, which ultimately contributes to the deterioration of the physiological parameters of the body as a whole and is a prerequisite for the development of general pathological conditions [15-17]. In addition to the above, odontogenic sinusitis can provoke the development of severe complications, such as thrombosis of intracranial sinuses, meningitis, and sepsis [6].Odontogenic maxillary sinusitis, complicated by the presence of oroantral communications, are divided into acute maxillary sinusitis (J 01.0), chronic maxillary sinusitis (J 32.0) (ICD 10). Based on the clinical rubrication, various methods of complex treatment of TMD are proposed [4]. One of the main stages of complex treatment of perforation sinusitis remains surgical intervention, the purpose of which is to correct the defect in the floor of the maxillary sinus [1].Despite the fact that dozens of types of surgical procedures have been described to eliminate defects in the floor of the maxillary sinuses, relapses occur quite often (9–30%) [2].Existing methods of surgical treatment of patients with defects of the floor of the maxillary sinuses are mostly exclusively invasive and often do not meet the principles of biological expediency, do not have an etiopathogenetic effect, do not restore the functional component (nasal breathing, adequate aeration of paranasal sinusitis), have significant risks of disease relapse and 8 more Moreover, they do not meet modern requirements, which are expressed in the most careful attitude towards the bone and soft tissue components of the alveolar process of the upper jaw, in particular, the attached and keratinized gum, necessary for subsequent dental rehabilitation with support for implants [1,4].Summarizing the above, it is worth noting that the issue of complex treatment of odontogenic maxillary sinusitis, complicated by the presence of oroantral communications, cannot be considered closed, and the choice of the optimal method for its elimination still remains a topic of active study.
2. Results
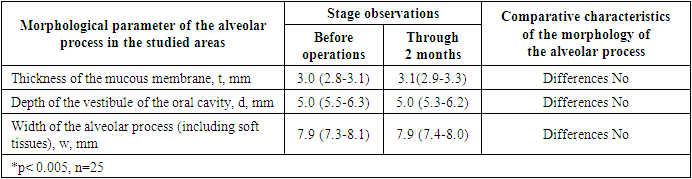
- After the surgical intervention, we carried out daily examinations and dressings, as well as recording dynamic changes in the clinical manifestations of the postoperative inflammatory process on days 3, 7, 10 and 14 based on scoring characteristics. Assessing the hyperemia of the mucous membrane in the postoperative area, we observed that the severity of this manifestation of the inflammatory process was characterized as moderate 2.0 points (1.0-2.0) and significantly regressed (on average) by 7 and 10 days, and by 14 completely was allowed. The low invasiveness of the surgical technique was confirmed, in particular, by the absence of collateral edema at all time intervals, which, in our opinion, is associated with the absence of large area full-thickness flaps (with trauma to the periosteum) and the absence of soft tissue mobilization techniques. We assessed wound bleeding during meals as insignificant during the first 3 days after surgery. According to patients, bleeding occurred due to trauma recipient zone when brushing teeth or breaking the diet, it was also noted that bleeding stopped quickly and spontaneously. When surveying patients regarding the severity of pain symptoms, patients noted that pain of minor intensity was present only during the first 3 days.Based on the data obtained, we concluded that patients fully recovered after surgery within 14 days, as well as the absence of complications such as pain, swelling or recurrence of perforation until the day of suture removal when carrying out a complex method of treatment of acute perforated maxillary sinusitis, developed by us.We recorded changes in the morphological parameters of the alveolar process in patients of the main subgroup before and after 3 months of surgery, which is presented in Table 1.
|
3. Discussion
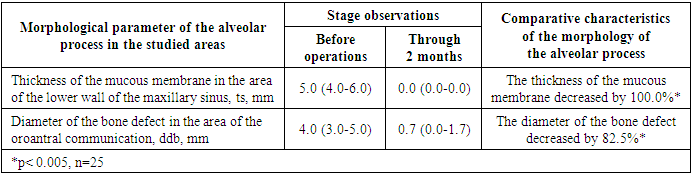
- We assessed CBCT data in patients of subgroup 2-a, the selection criteria were: ts - thickness of the mucous membrane of the maxillary sinus in the preoperative period t 1 and 3 months after surgery t 2, ddb - diameter of the bone defect in the area of the oroantral communication before surgery ddb 1 and 3 months after surgery ddb 2. Comparison of statistical data of radiological characteristics are presented in Table 2. Based on CBCT data in the preoperative period, the thickness of the mucous membrane of the maxillary sinus (in the area of the lower wall) corresponded to 5.0 (4.0-6. 0) mm, which we interpreted as the presence of minor reactive mucositis in the area of the oroantral communication, which developed in response to surgical trauma and minimal, initial microbial invasion of the bacterial flora of the oral cavity. The diameter of the bone defect in the area of the oroantral communication before surgery averaged 4.0 (3.0-5.0) mm. 3 months after surgery, the thickness of the PVS ts 2 was 117 0.0 (0.0-0.0) mm, which corresponds to a normal X-ray image of the maxillary sinus.
|
4. Conclusions
- A complex method for the treatment of chronic odontogenic maxillary sinusitis, complicated by the presence of an oroantral communication, using a subepithelial vascularized flap, autologous bone structures and platelet-rich fibrin (PRF). The use of the developed method of complex treatment significantly reduces the morbidity of surgical treatment: it reduces the intensity of the inflammatory reaction in the early postoperative period, and allows preserving the morphology of the bone and soft tissue components of the alveolar process of the upper jaw. The thickness of the mucous membrane in the area of the defect in the bottom of the maxillary sinus before surgery was 2.5(2.0-2.9) mm and 2.6(2.3-3.0) mm 3 months after surgery, the depth of the oral vestibule maintained preoperative values. values – 6.9 mm, the width of the alveolar process is unchanged before and 3 months after surgery and is 9.0 mm. X-rays revealed complete restoration of the functioning of the ostiomeatal complex and the upper jaw in 100% of cases 3 months after surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML