-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1126-1129
doi:10.5923/j.ajmms.20241404.67
Received: Apr. 2, 2024; Accepted: Apr. 22, 2024; Published: Apr. 28, 2024

Impact of Extensively Drug-Resistant, NDM-Producing Klebsiella Pneumoniae on the Healthcare System: A Case Study from a Tertiary Hospital in the United Arab Emirates
Ahmad Subhi 1, Salma O. Alshamsi 1, Ahmad Barbuor 2, Mohamad Mahfouz 2, Aulin Vitus 3
1Adult Infectious Diseases, Department of Medicine, Al-Qassimi Hospital, Emirates Health Services, UAE
2Department of Internal Medicine, Al-Qassimi Hospital, Emirates Health Services, UAE
3Prevention and Control of Infection Department, Al-Qassimi Hospital, Emirates Health Services, UAE
Correspondence to: Ahmad Subhi , Adult Infectious Diseases, Department of Medicine, Al-Qassimi Hospital, Emirates Health Services, UAE.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The emergence of extensively drug-resistant (XDR) Klebsiella pneumoniae, particularly strains producing the New Delhi metallo-beta-lactamase (NDM) enzyme, poses a formidable challenge to healthcare systems globally. In this manuscript, we present a retrospective case analysis conducted at a tertiary hospital in the United Arab Emirates (UAE) to investigate the impact of XDR Klebsiella pneumoniae on patient outcomes and healthcare resource utilization. Our study included 149 patients with XDR Klebsiella pneumoniae isolates, revealing a concerning trend of resistance to ceftazidime/avibactam and aztreonam antibiotics, indicative of prevalent NDM and AmpC gene mutations. This highlights the urgent need to address antimicrobial resistance. The implications of XDR Klebsiella pneumoniae on the UAE healthcare system are profound, encompassing clinical, financial, and infection control challenges. Prolonged hospital stays, increased morbidity and mortality rates, and significant financial burdens were observed. Effective antibiotic stewardship programs and multidisciplinary interventions are imperative to mitigate the spread of antimicrobial resistance and improve patient outcomes. In conclusion, our findings underscore the urgency of addressing the threat posed by XDR Klebsiella pneumoniae in the UAE healthcare setting. Proactive measures are essential to combat antimicrobial resistance and safeguard patient health.
Keywords: Klebsiella pneumoniae, Extensively drug-resistant, New Delhi metallo-beta-lactamase, Antibiotic stewardship, United Arab Emirates, Healthcare system
Cite this paper: Ahmad Subhi , Salma O. Alshamsi , Ahmad Barbuor , Mohamad Mahfouz , Aulin Vitus , Impact of Extensively Drug-Resistant, NDM-Producing Klebsiella Pneumoniae on the Healthcare System: A Case Study from a Tertiary Hospital in the United Arab Emirates, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1126-1129. doi: 10.5923/j.ajmms.20241404.67.
Article Outline
1. Introduction
- Carbapenems are indeed crucial antibiotics for treating severe infections caused by multidrug-resistant Gram-negative bacteria. Klebsiella pneumoniae, a common nosocomial pathogen, has increasingly shown resistance to carbapenems, posing a significant challenge, particularly in intensive care units (ICUs) where vulnerable patients are at greater risk of infection [1].Klebsiella pneumoniae is a versatile bacterium found in various environments, including soil, water, plants, and sewage, as well as in the human body, particularly in the nasopharynx and gastrointestinal tract. While it normally coexists harmlessly with humans, it can turn opportunistic and cause infections, both in hospital settings and the community. Its prevalence in hospital environments, especially in intensive care units, underscores its significance as a nosocomial pathogen [2].Infections caused by Klebsiella pneumoniae range from urinary tract infections to more severe conditions like bacteremia, respiratory tract infections, invasive liver abscesses, endophthalmitis, and endocarditis. The ability of Klebsiella pneumoniae to form biofilms on catheters contributes to its role in catheter-associated urinary tract infections. Additionally, it is a leading cause of neonatal sepsis, often stemming from localized infections in the urinary, gastrointestinal, or respiratory tracts.The emergence of extensively drug-resistant (XDR) Klebsiella pneumoniae, particularly those harboring the New Delhi metallo-beta-lactamase (NDM) enzyme, poses a formidable challenge to global healthcare systems. Klebsiella pneumoniae, a gram-negative bacterium, is notorious for its ability to acquire resistance mechanisms, rendering it resistant to multiple antibiotics, including carbapenems, often considered last-line therapies for multidrug-resistant infections [3]. The spread of XDR Klebsiella pneumoniae strains, fueled by factors such as overuse and misuse of antibiotics, inadequate infection control practices, and global interconnectedness, has raised concerns about the efficacy of available treatment options and the potential for widespread transmission within healthcare facilities [4].Several important risk factors for CRE infection were reported in previous studies and works of literature compared to controls showed that patients with an extended length of stay (LOS) could be at higher risk of infection due to the increased contact time with hospital environment, healthcare providers, and other patients. Receiving antimicrobial therapy such as beta-lactams or having previous surgery was also associated with CRE infections compared to controls. Surgery generally increases LOS increasing the potential for infection during the stay, and an open wound increases the risk of infection of any type [13].In recent years, the Gulf region has witnessed a troubling rise in cases of antibiotic-resistant infections, particularly those caused by New Delhi Metallo-beta-lactamase (NDM) and Carbapenem-resistant Enterobacteriaceae (CRE). These bacteria have developed mechanisms to resist some of the most potent antibiotics, posing significant challenges to healthcare systems and public health [11].In the United Arab Emirates (UAE), where the healthcare system strives to provide high-quality care to a diverse population, the emergence of XDR Klebsiella pneumoniae presents unique challenges. To understand the impact of these infections on patient outcomes, healthcare resource utilization, and infection control efforts, a retrospective case analysis was conducted at a tertiary hospital in the UAE. This manuscript aims to present the findings of this analysis and discuss the implications for healthcare practice and policy in the UAE and beyond.
2. Methods
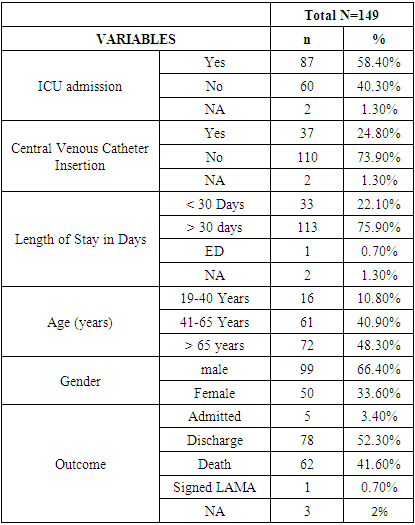
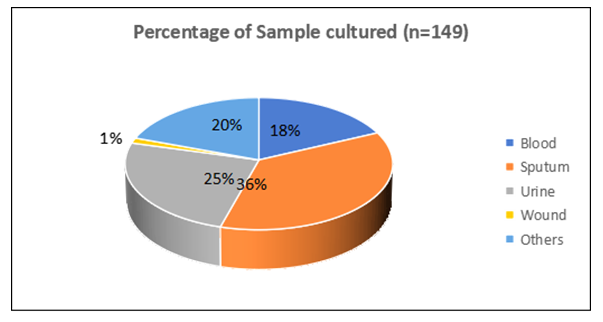
- After receiving the approval by the ethical committee of the Ministry of Health and Prevention (MoHAP) in UAE, a retrospective analysis was conducted using electronic medical records to identify patients with XDR Klebsiella pneumoniae isolates from January to July 2023. A total of 149 samples collected, The most common culture samples were sputum (36.2%), followed by urine (24.8%), others (19.5%), blood (18.1%), and wound (1.3%) [Fig. 1]. Data on antibiotic susceptibility patterns, clinical outcomes, and healthcare resource utilization were collected and analyzed. Descriptive statistics were used to summarize the findings, focusing on the prevalence of XDR Klebsiella pneumoniae and its resistance to ceftazidime/avibactam and aztreonam antibiotics.
 | Figure 1. Percentage of Sample cultured (n=149) |
3. Results
- Carbapenem resistance in Klebsiella pneumoniae or other bacteria occurs by two main mechanisms: production of carbapenemases and via porin loss combined with the presence of AmpC cephalosporinases or ESBLs and/or overexpression of efflux pumps [7,9].As carbapenemases are primarily mediated via mobile genetic elements contributing to the spread of carbapenem resistance, a more detailed discussion of these enzymes including class B (e.g., IMP, VIM, NDM) according to the Ambler classification. class B enzymes called metallo-β-lactamase (MBLs) which have garnered significant attention due to their rapid spread globally. They are often found in Enterobacteriaceae and have the ability to hydrolyze a broad range of β-lactam antibiotics but cannot hydrolyze the monobactam aztreonam unless there is a dual resistant gene mutation including NDM plus AmpC cephalosporinases or ESBLs [6].Studies and surveillance reports indicate a significant uptick in the incidence of NDM and CRE in the Gulf region. Countries like Saudi Arabia, the United Arab Emirates, and Kuwait have reported hospital outbreaks and increasing cases, highlighting the pressing nature of this public health crisis [10].The study that was focused on 149 patients infected with extensively drug-resistant (XDR) Klebsiella pneumoniae isolates. These bacteria demonstrated high resistance rates to ceftazidime/avibactam (73.8%) and aztreonam (57.7%) [Fig. 2], suggesting the presence of NDM and AmpC gene mutations. Various clinical samples such as blood, urine, sputum, and others showed diverse rates of resistance, indicating the varied sources and presentations of infection.
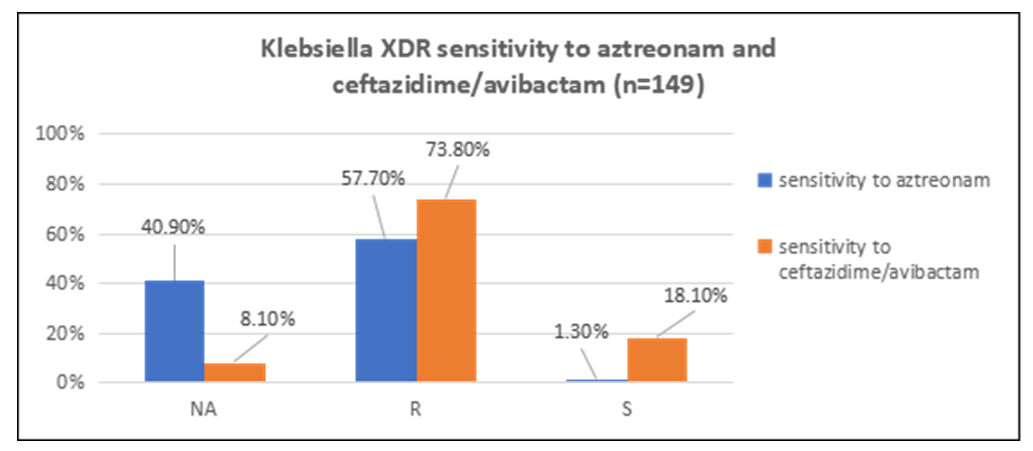 | Figure 2. Klebsiella XDR sensitivity to aztreonam and ceftazidime/avibactam (n=149) |
|
4. Conclusions
- The rise of antibiotic resistance poses one of the greatest threats to global health today, with carbapenem-resistant Enterobacterales (CRE) at the forefront of this crisis. Identified as a critical priority by the World Health Organisation (WHO), CRE infections are notoriously difficult to treat due to the limited alternatives available. The consequences of these infections are severe, leading to worse outcomes, extended hospital stays, and significant financial burdens on healthcare systems. This article delves into the challenges posed by CRE and explores the urgent need for innovative solutions [12].This retrospective case study at Al-Qassimi Hospital has illuminated the severe implications of extensively drug-resistant Klebsiella pneumoniae, particularly strains producing the New Delhi metallo-beta-lactamase enzyme, within the United Arab Emirates healthcare setting. The high resistance rates to critical antibiotics such as ceftazidime/ avibactam and aztreonam among the isolates studied signify a pressing challenge in managing infections effectively. This resistance not only complicates treatment strategies but also escalates the risk of adverse patient outcomes, including prolonged hospital stays and increased mortality rates.The study's findings underscore the urgent need for a multifaceted approach to tackle the growing threat of antimicrobial resistance. Key strategies should include the implementation of robust antibiotic stewardship programs aimed at optimizing the use of antibiotics to combat resistance development. Furthermore, rigorous infection control measures are essential to prevent the spread of these resistant strains within healthcare facilities. This includes enhancing hygiene practices, improving patient screening, and ensuring the judicious use of antibiotics.Additionally, the results highlight the importance of multidisciplinary collaboration among healthcare professionals, policymakers, and researchers to develop and enforce policies that address the root causes of antimicrobial resistance. Continuous surveillance and research are crucial to monitor resistance patterns and to innovate new treatment options.Ultimately, addressing the challenge of XDR Klebsiella pneumoniae and other resistant pathogens requires a concerted effort at both the national and international levels. The healthcare system in the UAE, like those worldwide, must adapt to this evolving threat to ensure the continued effectiveness of antibiotics and the protection of global health.This case study serves as a call to action, emphasizing the need for immediate and coordinated responses to mitigate the impact of antimicrobial resistance on patient health and healthcare resources.
Funding Acknowledgements
- This work received no specific grant from any funding agency.
Conflicts of Interest
- The authors declare that there are no conflicts of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML