Indiaminov S. I.1, Boltaev N. A.2
1Republican Scientific and Practical Center of Forensic Medical Examination, Ministry of Health of the Republic of Uzbekistan, Tashkent
2Navoi Branch of the Republican Scientific Center of Emergency Medical Care, Ministry of Health of the Republic of Uzbekistan, Navoi
Correspondence to: Indiaminov S. I., Republican Scientific and Practical Center of Forensic Medical Examination, Ministry of Health of the Republic of Uzbekistan, Tashkent.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The question of the timing of injury formation in cases of blunt trauma, both generally and particularly in cases of combined and multiple injuries, remains relevant in contemporary forensic medicine. It continues to be inadequately studied due to the exceptionally wide variety of factors that directly or indirectly influence the degree of development and dynamics of local and systemic reactive responses of organs and tissues. In order to identify changes in brain structures of individuals who died from combined polytrauma and to establish the timing of injuries, we examined the brains of 313 bodies of individuals with combined and multiple polytrauma, where there were no injuries to the skull and brain, which we referred to as extracerebral polytrauma. For specialized forensic-histological examination, samples were taken from the large cerebral hemispheres with cortex and underlying white matter, as well as from the wall of the lateral ventricle with a portion of the hypothalamus. A complex of morphometric studies was applied. It was found that in the early stages of extracerebral combined polytrauma, signs of acute edema and swelling are observed in nervous tissue. As the duration of trauma increases, the intensity of lesions in nervous tissue structures significantly increases, as evidenced by the dynamics of indicators, severity, volume, and degree of neuronal damage. It was noted that the average volumetric density of bloodless vessels significantly increases with the duration of traumatic illness caused by extracerebral combined and multiple trauma. It was also found that in individuals with extracerebral combined trauma from 9-12 hours to 6-8 days after the trauma, regardless of treatment received, there is a progressive decrease in glial index indicators in brain tissues.
Keywords:
Combined trauma, Timing, Brain, Structures, Morphometry
Cite this paper: Indiaminov S. I., Boltaev N. A., Forensic-Medical Significance of Changes in the Structures of the Brain of Individuals Who Died at Different Times of Extracerebral Combined Trauma, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1098-1102. doi: 10.5923/j.ajmms.20241404.62.
1. Introduction
The issue of timing in the formation of injuries resulting from blunt trauma, both generally and specifically in cases of combined and multiple trauma, remains pertinent in contemporary forensic medicine. It continues to be inadequately studied due to the exceptionally wide array of factors that directly or indirectly influence the degree of development and dynamics of local and systemic reactive responses of organs and tissues [Naumenko V.G., Mityaeva N.A., 1980; Sosedko Yu.I., 1985; Sapozhnikova M.A., 1988; Lapteva M.I., 2007; et al.].Establishing the thanatogenesis, causes of death, and timing of injuries in cases of various durations of survival following combined and multiple polytrauma is relevant not only to clinicians, especially surgeons and anesthesiologists-reanimatologists, for improving the diagnosis and treatment of trauma complications. It is known that in cases of combined and multiple trauma, accompanied by traumatic illness, the body develops a wide variety of local and systemic reactions with characteristic temporal dynamics. Moreover, determining the immediate causes is of paramount importance. It has been noted that both mechanical and thermal trauma result in early and late complications being the main and immediate causes of mortality [Selye G., 1971; Negovsky V.A., 1972; Bogomolov D.V., 2003; Zbrueva Yu.V., Dzhuvalyakov P.G., Bukeshov M.K., et al., 2012; and others].The utilization of so-called local reactions in injury zones for determining the timing of polytrauma is inefficient due to the different rates of their development in various organs and tissues, and the severity of polytrauma significantly influences their development time ([Sosedko Yu.I., 1985]). Hence, the prospective solution to this problem lies in using general trauma reactions, among which vascular organ reactions are the earliest and most universal, exhibiting certain sequences and phases of development under various impacts [Naumenko V.G., Mityaeva N.A., 1980; Viter V.I. et al., 2018; and others].Modern forensic-histological methods allow for the identification of changes in organ and tissue structures, particularly in brain structures, enabling the determination of the nature and phase of vascular-tissue reactions, thereby establishing the timing of injuries and substantiating the immediate causes of death, as well as the thanatogenesis of combined and multiple polytrauma accompanied by traumatic illness. However, for reliable and objective determination of temporal dynamics in the changes of structures of any organ and tissue, there arises the necessity to combine forensic-histological studies with modern morphometric methods [Avtandilov G.G., 1996; Pigolkin Yu.I., Bogomolov D.V., 2000-2010; Indiaminov S.I. et al., 2012; 2018; 2023; and others].Morphological studies, in conjunction with morphometric methods and mathematical analyses of obtained data, fully allow for objectifying the results of forensic-histological studies, addressing existing issues in understanding processes occurring at different time intervals following trauma [Avtandilov G.G., 1996].Objective: The aim of this study is to identify the dynamics of changes in brain structures in individuals who died from combined polytrauma in order to establish the timing of injuries.
2. Materials and Methods
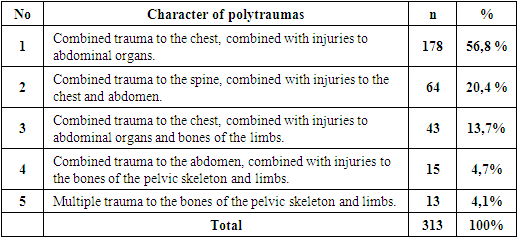
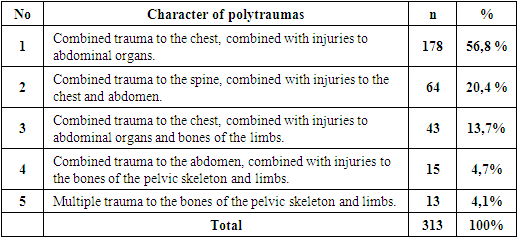
The brain tissue from 313 deceased individuals with combined and multiple polytrauma was examined. These individuals had no injuries to the skull and brain, a condition referred to as "extracerebral polytrauma" in this study. The selection of cases of death from polytrauma was based on anatomoclinical classifications of combined and multiple traumas [Shevchenko V.P. et al., 1980].The distribution of observations according to the nature and localization of combined and multiple polytrauma is presented in Table 1.Table 1. Character and location of combined and polytraumas
 |
| |
|
It is evident that the majority of injuries consist of combined trauma to the chest, combined with injuries to abdominal organs (56.8%), followed by spinal trauma combined with injuries to the chest and abdomen (20.4%), and chest trauma combined with injuries to abdominal organs and bones of the limbs (13.7%). Other variants of extracerebral polytrauma accounted for 4.1% and 4.7%, respectively. The majority of those who died from combined and multiple polytrauma were males, comprising 75.0%, while the remaining 25.0% were females. The largest proportion (43.7%) belonged to individuals aged 18-60 years.It was found that 168 victims (53.1%) with polytrauma died in medical institutions, while the remaining 145 (46.3%) died at the scene of the incident or in transit to medical facilities.To minimize the influence of autolytic processes on brain structures, cases with a time of death within 1 day were included in the study: in most cases (282), this was within 4-6 hours, in 19 cases within 7-12 hours, in 6 cases within 13-18 hours, in 4 cases within 19-24 hours, and in 2 cases within 25-36 hours. The duration of trauma in 145 cases ranged from a few minutes to 1 hour, while in the remaining 168 cases, it ranged from 1-2 hours to 8 days. In 72 cases, the presence of ethanol in various concentrations was detected in the blood of the victims during forensic chemical analysis of blood and urine. The volume of external and internal blood loss associated with injuries ranged from 1.0-1.5 liters to 2.0-2.5 liters. Infusion-perfusion therapy was administered to individuals who died in medical institutions in appropriate volumes.Complications of extracerebral combined and multiple polytrauma depended on the nature of the injuries to body parts and organs. Specifically, injuries to the chest structures predominated in manifestations of hemo-pneumothorax, tamponade, and pleuro-pulmonary shock. Meanwhile, injuries to abdominal organs led to massive blood loss and septic complications, while spinal cord injuries resulted in cervical-cranial trauma and spinal cord detachment. Traumatic shock, fat and thromboembolism, as well as septic complications, were common complications of injuries to limb and pelvic structures.The noted complications were direct causes of death for the victims during various periods of traumatic illness. During the examination of thanatogenesis of polytrauma, assessment was made considering the nature of the occurring complications.Taking into account the periodization of traumatic illness according to the classification of periods by S.A. Seleznev and G.S. Khudaybergenov (1984) and I.I. Deryabin and O.S. Nasenkin (1983), the studied material was divided into the following two subgroups: the first subgroup included individuals who died during the acute reaction period or in the shock period (up to 1 day) with 235 cases, while the second subgroup included 78 individuals who died during the early manifestations of trauma or during the period of adaptation and the risk of complications (from 1 day to 6-8 days).For specialized forensic-histological examination, samples were taken from the large cerebral hemispheres with cortex and underlying white matter, as well as from the wall of the lateral ventricle with a portion of the hypothalamus, which were fixed in 10% neutral formalin, passed through a series of alcohol baths, and prepared as paraffin blocks. Histological sections were stained with hematoxylin and eosin, as well as with Van Gieson's, Nissl's, and Mallory's methods. The study was conducted in two stages: the first stage involved in-depth forensic-histological examination of brain structures and the wall of the lateral ventricle with a portion of the hypothalamus, while the second stage involved morphometric studies of these structures and statistical analysis of the results.During the morphometric studies, the following methods were applied to quantitatively assess changes and their dynamics in brain structures:1. Histostereometric examination of the mean volumetric density (MVD) of vessels using the measuring grid by G.G. Avtandilov (1996).2. Morphometric studies of neuroglial complexes of the brain proposed by D.V. Bogomolov et al. (2001).3. Determination of the degree of nervous system damage using the method by A.M. Chubinidze (1972).4. Morphometric examination of the pericellular (PCP) and perivascular (PVP) spaces using the method by S.I. Indiaminov (2012) and Z.E. Zhumanov and S.I. Indiaminov (2023).
3. Results and Discussion
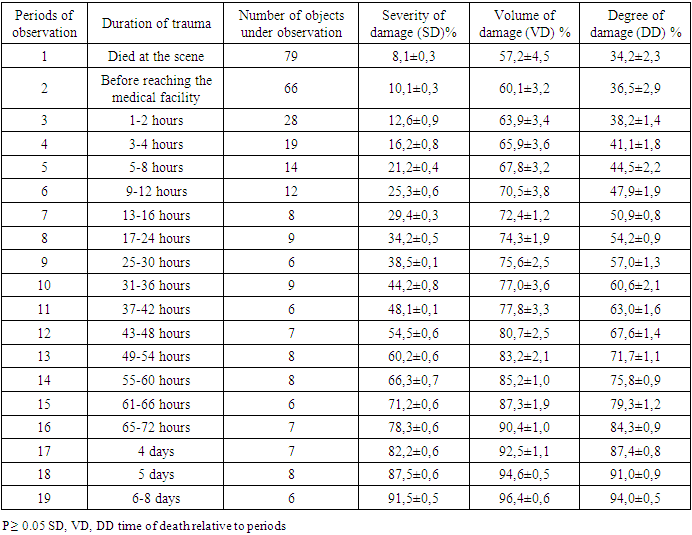
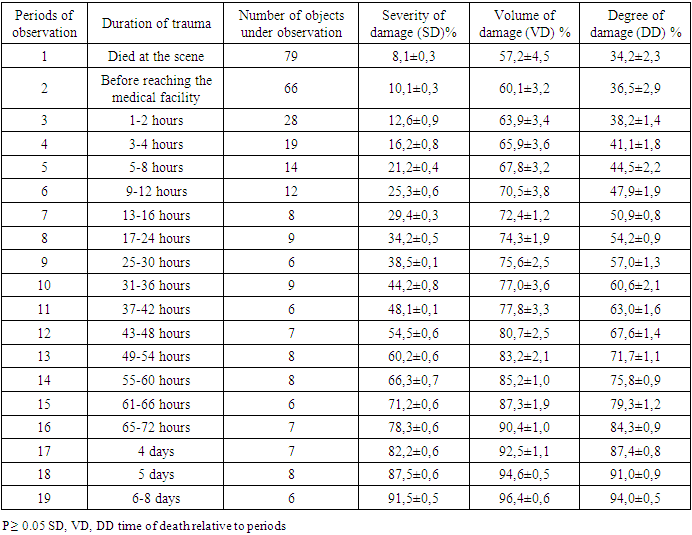
According to A.I. Chubinidze (1972), for practical purposes, histological changes in brain structures, regardless of the cause and localization of CNS lesions, can be divided into 4 severity groups:1. Grade 1 - representing mild damage, where the indicator value does not exceed 20%.2. Grade 2 - representing moderate damage, where the indicator value ranges from 20% to 50%.3. Grade 3 - representing severe damage, where the indicator value exceeds 50%.4. Grade 4 - characterized by persistent necrosis of the affected area (A.I. Chubinidze. Arch. Pathol. 1972. Vol. 11. p. 77).When studying the conditions of neurons in the cerebral cortex of deceased individuals who suffered injuries at the scene of the incident, it was found that the severity of the lesion (SL) was 8.1%±0.3, the volume of the lesion (VL) was 57.2%±4.5, and the degree of lesion (DL) was 34.2%±2.3, which corresponds to Grade 2±2.3. In cases of fatal outcomes in the early stages (up to 1 hour) after injury, the severity of the lesion (SL) was 10.1%±0.3, the volume of the lesion (VL) was 60.1%±3.2, and the degree of lesion (DL) was 36.5%±2.9 (P≥0.03).In the period from 1-2 hours to 9-12 hours after injury, the severity of the lesion (SL) ranged from 12.6%±0.9 to 25.3%±0.6, the volume of the lesion (VL) ranged from 63.9%±3.4 to 70.5%±3.8, and the degree of lesion (DL) ranged from 38.2%±1.4 to 47.9%±1.9. According to A.I. Chubinidze's data, these indicators correspond to moderate, i.e., Grade 2, neuron lesions.With injury durations from 13-16 hours to 6-8 days, the severity of the lesion (SL) ranged from 29.4%±0.3 to 91.5%±0.5, the volume of the lesion (VL) ranged from 72.4%±1.2 to 96.4±0.6, and the degree of lesion (DL) ranged from 50.9%±0.8 to 94.0%±0.5. These indicators correspond to severe, i.e., Grade 3, neuron lesions. After 6-8 days post-injury, Grade 4 neuron lesions, i.e., persistent necrosis, were observed in the studied brain areas (P≥0.05). Table 2.Table 2. The severity, volume, and degree of neuron damage in the structures of the cerebral cortex of the brain in individuals who died as a result of extracerebral combined trauma (M ± m, %)
 |
| |
|
Thus, in the early stages of extracerebral combined trauma, signs of acute edema and dystrophy are detected in nervous tissue. As the duration of the trauma increases, the intensity of damage to nervous tissue structures significantly increases.We also found that in individuals who died at the scene of the incident from extracerebral polytrauma, perivascular edema (PVE) in the brain regions under study was 3.31±0.02, while in those whose death occurred between transportation and arrival at the hospital after the trauma, PVE was - 4.48±0.02. However, the difference in these two periods was low (1.3 times). In the first 1-2 hours after the trauma, PVE was 5.41±0.02, after 9-12 hours - 6.28±0.03, and after 17-24 hours - 6.81±0.02. This indicates a significant increase in PVE values by 2 times compared to the 1st period. By 25-30 hours after the trauma, PVE was 7.29±0.04, at 4 days - 10.46±0.02, and after 6-8 days - 11.29±0.02. This means that PVE values increased by 1.6 times compared to the 8th period (17-24 hours) and by 3.4 times compared to the 1st period (P≥0.03).In individuals who died at the scene of the incident, pericellular edema (PCE) in the brain regions was 2.26±0.02. In those who died during the transportation to the hospital after the trauma, it was 3.03±0.02. However, the differences in PCE values between these two periods were only 1.3 times. At later stages, i.e., in the first 1-2 hours after the trauma, PCE was 3.44±0.02, after 9-12 hours - 6.43±0.03, and after 17-24 hours - 7.75±0.02. This indicates a significant increase in PCE values by 3.4 times compared to the 1st period. By 25-30 hours after the trauma, PCE was 8.57±0.02, at 4 days - 11.79±0.02, and after 6-8 days - 12.05±0.03. This means that at the last period, PCE values increased by 1.5 times compared to the 8th period (17-24 hours) and by 5.3 times compared to the 1st period (P≥0.05).The data presented indicate a high degree of damage to the nervous tissue of the brain in cases of extracerebral combined trauma. Therefore, the thanatogenesis of traumatic disease varies depending on the types and severity of combined and multiple injuries. With preserved vascular filling, caused by combined trauma, the degree of involvement of nervous tissue and blood vessels in the thanatogenesis of polytrauma is approximately the same. With hypovolemia caused by combined trauma, an increase in pericellular edema (PCE) indicators over the course of traumatic disease may be observed.In individuals who died at the scene of the incident from combined trauma, the degree of hypovolemia (mean volumetric density - MVD of vessels) of brain tissue was 2.82±0.24, while in those who died before the victim was taken to a medical institution, this indicator was 2.84±0.26. One to two hours after the trauma, it was 3.79±0.25, three to four hours later - 3.89±0.21; five to eight hours later - 4.74±0.25; nine to twelve hours later - 4.90±0.20; 4.96±0.14 after thirteen to sixteen hours; 4.93±0.23 after seventeen to twenty-four hours; 5.97±0.12 after twenty-five to thirty hours; 5.94±0.16 after thirty-one to thirty-six hours; 6.94±0.16 after thirty-seven to forty-two hours; 6.95±0.47 after forty-three to forty-eight hours; 8.96±0.14 after forty-nine to fifty-four hours; 9.92±0.19 after fifty-five to sixty hours; 10.94±0.16 after sixty-one to sixty-six hours; 11.95±0.15 after sixty-seven to seventy-two hours; 13.07±0.18 after four days; 13.90±0.21 after five days; 14.94±0.16 after six to eight days. Thus, the mean volumetric density (MVD) of bloodless vessels significantly increases over the course of traumatic disease caused by extracerebral combined and multiple trauma. The results of studying the reactions of round-cell glia in pathological conditions have shown that the higher the density of glia in the brain tissue, the smaller the mean glial distance, and the higher the functional activity of the neuroglial complex of the brain (D.V. Bogomolov, Yu.I. Pigolkin, O.V. Dolzhansky, 2001).We found that the glial index in the cortex of the brain of individuals who died at the scene of the incident from combined trauma is 11.85±0.01, while in those who died before hospitalization in a medical institution, it is 11.63±0.02. Glial index indicators one to two hours after the trauma were 11.49±0.03. It was noted that the glial index indicators progressively increased up to 9-12 hours after the injury, and then decreased: after 3-4 hours - 11.23±0.03; after 5-8 hours - 11.31±0.03; after 9-12 hours - 11.48±0.03; after 13-16 hours - 11.45±0.03; after 17-24 hours - 11.41±0.02; after 25-30 hours - 11.53±0.02; at 31-36 hours - 10.61±0.04; at 37-42 hours - 10.32±0.02; after 43-48 hours - 9.73±0.02; after 49–54 hours - 9.43±0.02; after 55-60 hours - 9.32±0.02; at 61-66 hours - 8.66±0.02; after 67-72 hours - 8.22±0.02; after four days - 7.59±0.02; after five days - 7.03±0.02; and after 6-8 days, it was 6.40±0.02. These data indicate that in individuals with extracerebral combined trauma, there is a progressive decrease in glial index indicators in brain tissue from 11.48±0.01 to 6.40±0.02 from 9-12 hours to 6-8 days after the injury, regardless of the treatment performed (p≥0.05).
4. Conclusions
1. Thus, in the early stages of extracerebral combined polytrauma, signs of acute edema and swelling are detected in the nervous tissue. As the duration of the trauma increases, the intensity of damage to the structures of the nervous tissue significantly increases, as evidenced by the dynamics of indicators of severity of injury (ТП), volume of damage (VD), and degree of damage (DD).2. Judging by the results of studies on perivascular edema (PVE) and pericellular edema (PCE), the hematogenesis of the traumatic disease varies depending on the severity and duration of combined and multiple polytraumas. With the preservation of vascular perfusion due to combined trauma, the degree of involvement of nervous tissue and blood vessels in the thanatogenesis of combined polytrauma is approximately the same. With hypoperfusion, a predominance of PCE indicators may be observed over time in traumatic disease. Consequently, the mean volumetric density (MVD) of de-vascularized vessels significantly increases with the duration of traumatic disease caused by extracerebral combined and multiple traumas.3. It has been noted that the indicators of the glial index increase up to 9-12 hours after the trauma from 11.23±0.03 to 11.48±0.03. After 9-12 hours and up to 6-8 days, the indicators of the glial index decrease from 11.45±0.03 to 6.40±0.02 (p≥0.05). These data indicate that in individuals with extracerebral combined trauma, there is a progressive decrease in the indicators of the glial index in brain tissue from 9-12 hours to 6-8 days after the trauma, regardless of the treatment administered.4. The collected data plays a crucial role in determining the duration of combined polytrauma and evaluating the thanatogenesis of traumatic disease.
References
| [1] | Avtandilov, G.G. (1996). Kompyuternaya mikrotelefotometriya v diagnosticheskoy gistotsitopatologii [Computer microtelephotometry in diagnostic histocytopathology]. Moscow: RMAPO. |
| [2] | Bogomolov, D.V. (2003). Vozmozhnosti primeneniya modal'noy logiki pri tanatogeneticheskom analize v sudebnoy meditsine i patologii [Possibilities of using modal logic in tanatogenetic analysis in forensic medicine and pathology]. Problemy ekspertizy v meditsine, 3(4), 40–42. |
| [3] | Viter, V.I. (2018). Sudebno-meditsinskaya gistologiya [Forensic histology]: Rukovodstvo dlya vrachey. Izhevsk, p. 234. |
| [4] | Zbrueva, Yu.V., Dzhuvalyakov, P.G., Bukeshov, M.K., Bogomolov, D.V., & Fedulova, M.V. (2012). Sudebno-meditsinskaya otsenka tanatogeneza pri perezhitii mekhanicheskoy i termicheskoy travmy [Forensic medical assessment of tanatogenesis in mechanical and thermal trauma experience]. Sudebno-meditsinskaya ekspertiza, 55(5), 24–26. |
| [5] | Lapteva, M.I. (2007). Sudebno-meditsinskoe ustanovlenie davnosti tupoy mekhanicheskoy travmy myagkikh tkanei (morfometricheskoe issledovanie) [Forensic medical establishment of the duration of blunt mechanical trauma to soft tissues (morphometric study)]. Avtoref.diss.kand.med.nauk. Moscow, 22 p. |
| [6] | Naumenko, V.G., & Mityaeva, N.A. (1980). Gistologicheskie i tsitologicheskie metody issledovaniya i sudebnaya meditsina [Histological and cytological methods of research and forensic medicine]. Moscow: Meditsina. |
| [7] | Pigolkin, Yu.I., Bogomolov, D.V., Bogomolova, I.N., Baranova, M.Ya., & Ozdamirova, Yu.M. (2001). Vozmozhnosti ispol'zovaniya morfometricheskikh metodov v sudebno-meditsinskoy diagnostike otravleniya narkotikami [Possibilities of using morphometric methods in forensic medical diagnosis of drug poisoning]. Problemy ekspertizy v meditsine, 1(1), 18–20. |
| [8] | Sapozhnikova, M.A. (1988). Morfologiya zakrytoy travmy grudi i zhivota [Morphology of closed chest and abdominal trauma]. Moscow: Meditsina. |
| [9] | Sosedko, Yu.I. (1985). Sudebno-meditsinskaya diagnostika tupoy cherepno-mozgovoy travmy [Forensic medical diagnosis of blunt cranial-cerebral trauma]. In Aktual'nye voprosy sudebnoy meditsiny i ekspertnoy praktiki [Current issues in forensic medicine and expert practice]. Rostov-on-Don, 65–67. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML