-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1093-1097
doi:10.5923/j.ajmms.20241404.61
Received: Feb. 2, 2024; Accepted: Apr. 3, 2024; Published: Apr. 25, 2024

Features of Clinical and Neurological Manifestations and Biochemical Aspects of the New Coronavirus Infection (COVID-19) in Children
Temirova M. K., Botirov I. R., Mukhammadjonova D. M.
Tashkent Pediatric Medical Institute, Andijan State Medical Institute, Republic of Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article reveals the relevance of the problem of coronavirus infection in children, examines the risks of the disease, neurological manifestations, laboratory data, and considers options for the severe course of the disease.
Keywords: COVID-19, New coronavirus infection, Pediatric multisystem inflammatory syndrome, Meningitis, Encephalitis, Encephalopathy
Cite this paper: Temirova M. K., Botirov I. R., Mukhammadjonova D. M., Features of Clinical and Neurological Manifestations and Biochemical Aspects of the New Coronavirus Infection (COVID-19) in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1093-1097. doi: 10.5923/j.ajmms.20241404.61.
Article Outline
1. Introduction
- At the end of December 2019, an outbreak of a new coronavirus infection (COVID-19) caused by the SARS-CoV-2 coronavirus, leading to severe acute respiratory syndrome, was recorded in Wuhan (Hubei Province, China). [1] In almost all published original studies of COVID-19 cases, it is noted that, in addition to impaired respiratory system function, one third of patients (30%-35%) show signs of damage to the nervous system. [2-3] When infected with the SARS-CoV-2 virus, patients experience headache, nausea, vomiting, dizziness, myalgia, weakness, fatigue. Nausea and vomiting can be the result of disorders of both the digestive and nervous systems, if these symptoms manifest themselves along with headache, high intracranial pressure. Obviously, SARS-CoV-2 can infect the nervous system. The presence of viral particles directly in neurons is shown using electron microscopy on brain slices of patients who died from COVID-19. [4] According to recent publications, this virus causes a range of neurological complications: viral encephalitis, meningoencephalitis, ischemic and hemorrhagic strokes. [5]
2. Objective
- To study the clinical, neurological and biochemical (Substance P) features in children with coronavirus infection.
3. Materials and Methods
- The research work is based on the results of an examination and study of 80 children who received inpatient treatment in the departments of the Specialized Hospital Zangiota №1 for the treatment of patients with coronavirus infection of the hospital, as well as an outpatient examination in the period 2021-2022.
4. The Results of the Study
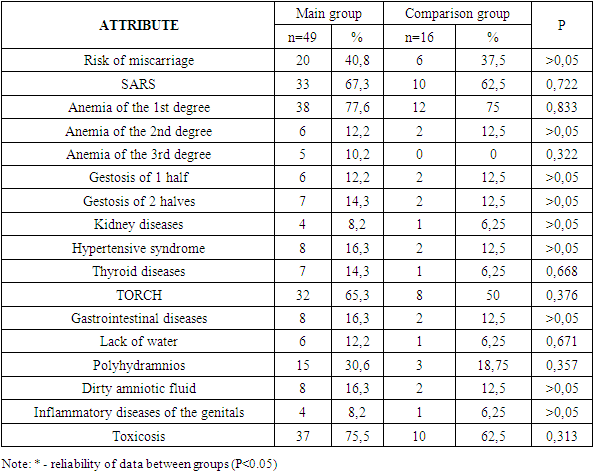
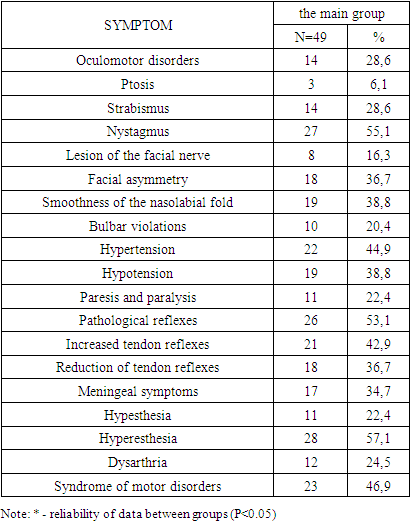
- 80 children with coronavirus infection were under our supervision. The main group consisted of 49 (61.3%) patients, of which 33 (67.3%) boys and 16 (23.7%) girls with confirmed COVID–19 (based on PCR testing of the upper respiratory tract, serological examination for antibodies to SARS-CoV-2, and clinical outcomes) and neurological disorders. The comparison group consisted of 16 (20%) children, of which 7 (43.8%) boys and 9 (56.2%) girls with established COVID–19 infection (based on PCR testing of the upper respiratory tract, serological examination for antibodies to SARS-CoV-2, and clinical outcomes) without neurological disorders. The control group consisted of 15 (18.7%) healthy children, of which 6 (40%) were boys and 9 (60%) were girls.The main group of patients was divided into 2 additional groups: group I, 26 (53.1%) children with neurological disorders without systemic manifestations and group II, 23 (46.9%) children with neurological disorders on the background of systemic disorders (CD and MSVS).
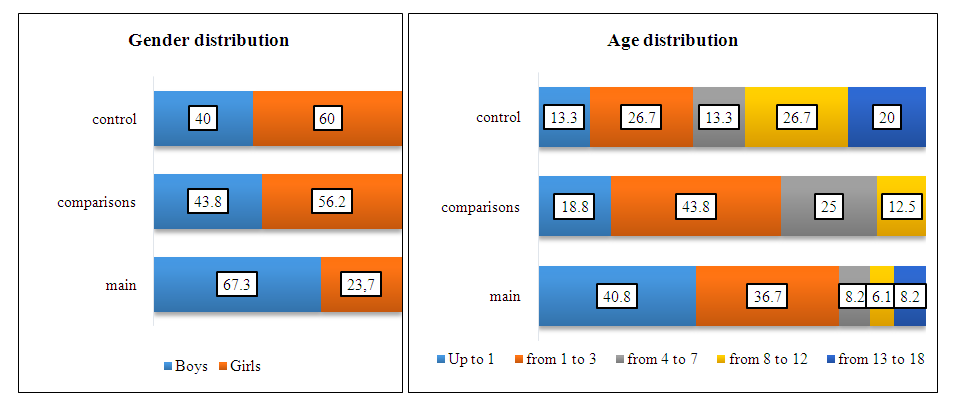 | Figure 1. Sex and age characteristics of the examined patients |
|
|
|
|
|
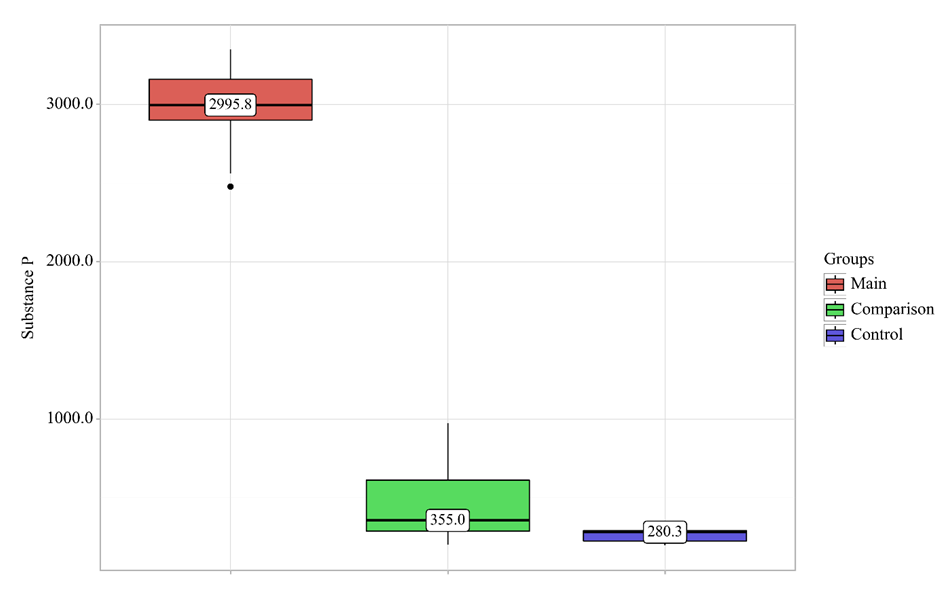 | Figure 2. The level of Substance P depending on the patient group |
5. Conclusions
- Neurological disorders in children with coronavirus infection can occur both in isolation and in the structure of a systemic lesion, which is manifested by multisystem inflammatory syndrome or Kawasaki disease. Neurological disorders in children with COVID-19 most often occur in infancy and in preschool age.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML