-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1080-1083
doi:10.5923/j.ajmms.20241404.58
Received: Mar. 29, 2024; Accepted: Apr. 16, 2024; Published: Apr. 19, 2024

Forensic Aspects of Diagnosing Diffuse Axonal Brain Damage in Traumatic Brain Injuries
A. A. Iskandarov, A. A. Ismatov, K. U. Kodirov
Department of Forensic Medicine and Medical Law, Tashkent Pediatric Medical Institute, Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Traumatic brain injury (TBI) is the principal cause of invalidity and death in the population under 45 years of age worldwide. This mini-review aims to systematize the forensic approach in neuropathological studies, highlightingthe proper elements to be noted during external, radiological, autoptical, and histological examinations with particular attention paid to immunohistochemistry and molecular biology. In the light of the results of this mini-review, an accurate forensic approach can be considered mandatory in the examination of suspected TBI with medico-legal importance, in order to gather all the possible evidence to corroborate the diagnosis of a lesion that may have caused, or contributed to, death. From this point of view, only the use of an evidence-based protocol can reach a suitable diagnosis, especially in those cases in which there are other neuropathological conditions (ischemia, neurodegeneration, neuro-inflammation, dementia) that may have played a role in death.
Keywords: Traumatic brain injury, Neuropathology, Forensic radiology, Autoptic approach, Histopathology, miRNA, Molecular biology, Axonal brain injury, Pyramidal, Extrapyramidal, Bolshovsky and Glis, Pathomorphological manifestations
Cite this paper: A. A. Iskandarov, A. A. Ismatov, K. U. Kodirov, Forensic Aspects of Diagnosing Diffuse Axonal Brain Damage in Traumatic Brain Injuries, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1080-1083. doi: 10.5923/j.ajmms.20241404.58.
Article Outline
1. Introduction
- Traumatic brain injury (TBI) occupies a leading place among all types of mechanical injuries. It is characterized by a wide variety of clinical and morphological manifestations and high rates of mortality and disability, which gives this problem important medical and social significance [1,2,4,9,12]. The works currently available in the literature devoted to various aspects of the forensic medical assessment of TBI cannot be considered scarce. However, the primary emphasis in them is on studying the mechanism of bone damage. Additionally, the forensic assessment of brain injury has been developed primarily for cases with cerebral damage visible on gross examination. However, the literature often provides evidence of a discrepancy between the severity of brain damage and relatively minor external manifestations of injury, as well as the absence or mild severity of cranial damage [4].In the practice of a forensic medical expert, there are often cases of TBI obtained in conditions of obviousness in the presence of witnesses, without visible various changes in the brain and its membranes, without bone damage to the vault and base of the skull and the absence of damage to the soft tissues of the head. Histological examination in such observations also, as a rule, does not bring certain clarity, and expert assessment of the nature of the damage, the mechanism and conditions of causing TBI is accompanied by significant difficulties, often serving as a reason for repeated examinations [5,6,7,10,11]. These unique forms of TBI include diffuse axonal brain injury (DBA).The purpose of this study is to develop clinical and morphological criteria for expert assessment of DAP in traumatic brain injuries.
2. Materials and Methods of Research
- The material for the study was 52 cases of fatal TBI, in the vast majority of cases it was associated with a road traffic accident (RTA). According to our observations, DAP occurred in 13 cases, which accounted for 25% of all deaths. It should be noted that all of these cases with DAP victims were in specialized departments of the Research Institute of Traumatology and Orthopedics, the Republican Center for Neurosurgery and the Scientific Center for Emergency Medical Care (RSCEM) of the Ministry of Health of the Republic of Uzbekistan. The average age of victims in cases of DAP was 37.4±2.6 years and the victims were all male.Research methods included both clinical (CT and MRI) and general morphological. The syndrome of disconnection of the hemispheres, subcortical formations and brain stem, which dominates during long-term experience of trauma in victims (more than 2 weeks) after the transition of coma to a persistent vegetative state, is of great expert importance in the assessment of DAP. The presence of this syndrome is a reliable sign of this form of TBI (_). This syndrome makes it possible to diagnose DAP based on clinical data even without CT and MRI.
3. Research Results and Discussion
- Clinical manifestations of DAP indicate that the main diagnostic criterion for this form of TBI is a long-term coma that occurs from the moment of injury with severe brainstem and hemispheric disorders. In addition to diagnostic, these signs also have expert significance. Coma in all cases of DAP in our observations (13) developed from the moment of injury and lasted up to 30-40 days. Moreover, in most cases (61.5%) the victims were in a comatose state until death. In these cases, the duration of coma ranged from 2 days to 29 days (on average 15.5±2.3 days). In other cases in which recovery from it was noted, the duration of the coma varied from 3 to 38 days (on average 17.3 ± 3.4 days).Among victims with DAP, both deep coma (4-5 points on the GCS) and moderate coma (6-7 points on the GCS) occurred in 5 observations. It should be noted that deep coma was associated with younger age, while moderate coma was more common at older age. Just like coma, from the moment of injury, all victims with DAP experienced severe brainstem symptoms, which were pronounced for almost two weeks. There was depression or absence of photoreaction of the pupils on one or both sides, corneal reflexes, and upward gaze. The difference between the eyes vertically and horizontally and loss of the oculocephalic reflex were noted in almost half of the cases (46.2%).Pyramidal and extrapyramidal disorders reached a high frequency (84.6%). In 5 cases (38.5%) of observations, coma was accompanied by symmetrical or asymmetrical decerebration or decortication; At the same time, vorleable changes in muscle tone were noted from diffuse muscle atony to hormetonia. In the dynamics of the clinical course of DAP, when surviving trauma for up to two weeks, a transition from coma to a persistent vegetative state was observed. With CT and MRI, the criteria for DAP during the first two weeks after injury are: the absence of focal extra- and intracerebral damage accompanied by compression of the brain; changes in brain volume; “motley” picture of white matter.In addition to changes in the volume and density of brain tissue, CT and MRI in cases of DAP revealed small focal increases in density (hemorrhages) in the deep structures of the brain. They were mainly localized in the corpus callosum, in the semioval center, in the area of the internal capsules and basal ganglia. The macroscopic picture of the brain in DAP is determined by the duration of the trauma. When victims die within the first week after injury, moderate swelling of the brain is detected, more often in young people. Morphological markers of DAP are small-focal or focal hemorrhages in the corpus callosum in the region of the basal ganglia, centrum semiovale, and less commonly in the trunk. These injuries are based on ruptures of intracerebral vessels, which are associated with stresses inside the brain as a result of its rotational displacement.After surviving for one week, white matter hemorrhages show signs of age, and if a long time has elapsed (more than a month) after the injury, brown cysts form in the area of primary damage. When examining the brain in cases of longer-term experience, a picture of brain atrophy with expansion of the basal cisterns and subarachnoid fissures is determined. Histological examination of the brain in cases of DAP, in addition to traditional staining, requires the mandatory use of methods according to Bielschowsky and Glies for changes in the axial cylinders, according to Markey and Spielmeyer - for early and late demyelination.According to our observations, in the initial stages of DAP, it is advisable to use silver impregnation (according to Bolshovsky and Glis) to resolve the issue of the presence of damage to the white matter. In periods of more than 1 week, we determined DAP by osmium impregnation according to Marquis, where degenerative changes in the myelin sheaths were determined. When the injury was experienced for more than two months, areas of axonal damage were identified when staining preparations using the Spielmeyer method, areas of axonal damage were identified, which by that time were completely demyelinated. The results of our studies showed that damage to axonal DAP was mainly found in the trunk (76.6%), in the corpus callosum, in the internal capsules (50.3%), in 46.8% - in the basal ganglia and in 36.4% - in the semioval center.It should be noted that during macroscopic examination of the brain, damage in these structures was found much less frequently. Consequently, macroscopic examination allows us to resolve the issue of the presence of DAP, but histological verification is mandatory. In addition, establishing the localization of areas of axonal damage during histological examination with a high degree of probability allows us to resolve the issue of the circumstances and mechanism of head injury. Pathological manifestations, being diagnostic criteria for DAP, make it possible to judge their age. Thus, the detection of axonal balls with signs of initial axonal degeneration near them in the above-mentioned parts of the brain indicates a duration of the post-traumatic process of no more than 3 days. If, in addition to the axonal balls, degenerative changes are determined along the entire length of the damaged axons, then the period of experiencing the injury can last from 3 days to 7 days. In this case, the degeneration of myelin sheaths is determined by the Marquis method, which allows us to conclude that the experience lasted for at least 5 days. Determination of a moderate macrophage reaction in areas of damage to the white matter in the above structures indicates a duration of the post-traumatic period of at least one week. At the same time, the identification of signs of secondary degeneration of the central nervous system pathways near the sites of primary axonal damage indicates a period of trauma experience from one week to 14 days. The discovery of pronounced signs of degeneration of nerve fibers in the area of injury in the presence of a small number of axonal balls indicates that more than 2 weeks have passed since the injury. The absence of axonal balls and the disappearance of damaged nerve fibers against the background of diffuse proliferation of macrophages and pronounced secondary degeneration of nervous tissue indicates that the brain has been injured for more than a month.Complete demyelization of the white matter in the area of primary damage against the background of generalized degeneration of brain axons indicates a duration of TBI of at least 2 months. Morphological signs of atrophy of the white matter of the brain and determination of degenerative changes in the axons of the brain and peripheral nervous system indicate that the brain has been injured for more than 3 months. Thus, based on the nature of the pathomorphological changes in the brain during DAP, one can speak with a certain degree of certainty about the timing of the onset of head injury. Clinical, morphological and CT criteria for diagnosing DAP depending on the duration of the post-traumatic period are presented in Table No. 1.
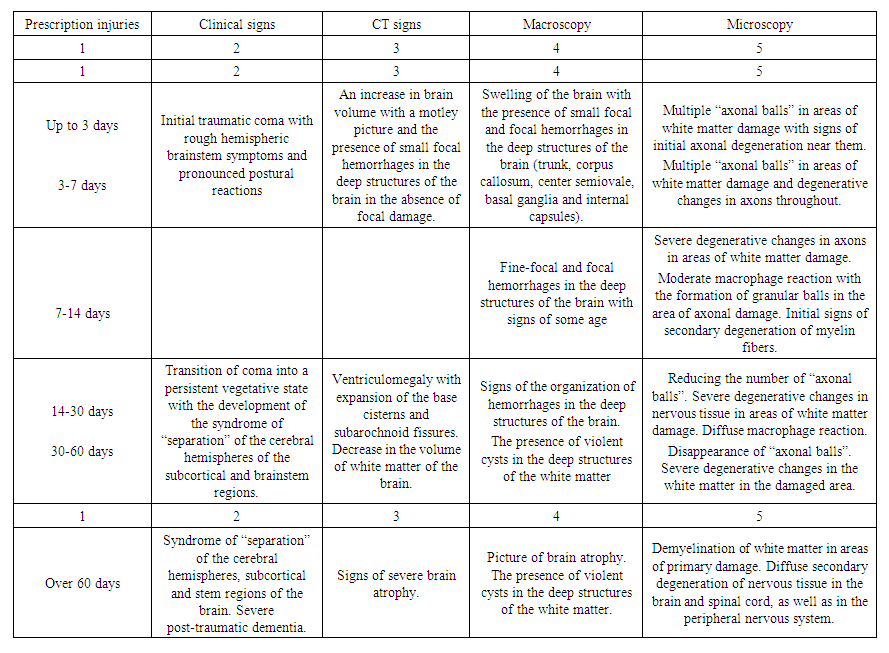 | Table 1. Clinical, morphological and CT criteria for diagnosing DAP, taking into account the duration of traumatic brain injury |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML