-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1077-1079
doi:10.5923/j.ajmms.20241404.57
Received: Mar. 22, 2024; Accepted: Apr. 10, 2024; Published: Apr. 19, 2024

Obesity is a Risk Factor for Prediabetes
Mukhamedova V. M., Nishanova M. S.
Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Obesity is a disease that, unfortunately, is becoming more and more common. We can see obese patients on the street, at work, and even at home; our loved ones find themselves overweight. Obesity is a very insidious disease; it can begin to develop for reasons such as stress, poor lifestyle or hereditary predisposition. Obesity is necessarily accompanied by other diseases, such as, for example, diabetes mellitus, arterial hypertension, varicose veins, arthrosis, and atherosclerosis. If obesity is not treated promptly, people doom themselves to develop chronic diseases and even die.
Keywords: Obesity, Overweight, Prediabetes, Glycated hemoglobin
Cite this paper: Mukhamedova V. M., Nishanova M. S., Obesity is a Risk Factor for Prediabetes, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1077-1079. doi: 10.5923/j.ajmms.20241404.57.
1. Introduction
- Prediabetes can progress to T2DM in 50% of cases within 5 years [3]. In this regard, prediabetes has received increasing attention in attempts to delay the onset of T2DM and prevent or delay microvascular and macrovascular complications [1,4].However, information on the epidemiology of prediabetes and its associations with obesity is scarce and absent in the modern population of the Andijan region. This is the reason for late diagnosis of diabetes and its complications with all its serious consequences. For this reason, there are still no epidemiological diagnostic criteria for prediabetes, although risk factors for prediabetes and/or diabetes are formed or accumulate long before specific manifestations appear [2].Purpose of the study: to study the effect of body mass index on the incidence of carbohydrate metabolism disorders.
2. Materials and Methods
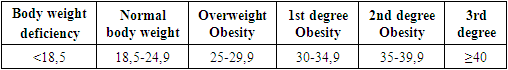
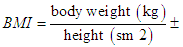
- Strictly according to the scenario of the epidemiological study, 2112 people (coverage - 100.0%), women - 83.1% and men - 16.9% were examined. All those examined were representatives of the indigenous population of the Markhamat district of the Andijan region. Involvement of the population in the survey was ensured through a written invitation and home visits. Work with the invitation was completed after the survey.The following methods were used in the population survey: epidemiological, clinical, biochemical, instrumental and statistical. The population was examined using standardized and unified DiaHatar questionnaires to assess the risk of prediabetes and T2DM.Risk factors were determined and assessed according to the criteria of the WHO, the Russian Association of Endocrinologists (2017), EASD and ADA (2015, 2018), Clinical recommendations for the management of patients with type 2 diabetes mellitus of the Republic of Uzbekistan (2 For a biochemical study before blood sampling, the fasting period was 10-12 hours The concentration of glucose in the blood plasma was determined using the Mindray A88 automatic analyzer. Determination of glycemia/glucose in the blood plasma. A fasting plasma glucose level of <6.1 mmol/l was taken as normoglycemia, and a range of plasma glucose concentrations was taken as impaired fasting glucose (IFG). from 6.1<7.0 mmol/l, for impaired glucose tolerance (IGT) ≥7.8<11.1 mmol/l, concentration equal to or exceeding 7.0 mmol/ (ADA criteria) - DM. Glycated hemoglobin (HbA1c) was also selected as a diagnostic criterion for diabetes. The study of HbA1c in venous blood was carried out on a Mindray A88 analyzer using the Max-Planck-Ring21 65205 Wiesbaden Germany reagent, manufactured in Germany. This method for determining HbA1c is standardized in accordance with the requirements of NGSP/DCCT and IFCC.The anthropometric study was carried out as follows: height was determined in the “standing” position with an accuracy of 0.5 cm (without shoes), and the heels, buttocks and shoulders of the subject should touch the measuring pole, the head should be positioned so that the connecting line was horizontal. Body weight was measured without shoes on standard scales, with an accuracy of 0.1 kg. To study overweight (BMI) and obesity, the following was carried out: calculation of body mass index (BMI) was carried out using the Quetelet index (QI) - the ratio of body weight in kg to the square of height in meters according to the formula, the level of obesity was calculated (Table 1).
|
3. Results and Their Discussions
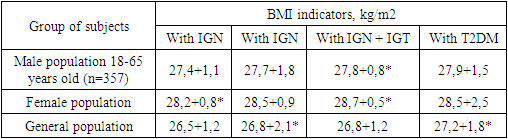
- It turned out that all individuals with glycemic disorders have increased body weight (Table 2). Thus, BMI was noted in various disorders of body weight with the following indicators: with NGN - 27.4 kg/m2 (in women - 28.2 kg/m2 and men - 26.5 kg/m2, P> 0.05), with IGT - 27.7% (in women - 28.5 kg/m2 and men - 26.8 kg/m2, with IGN + IGT - 27.8 kg/m2 (in women - 28.7 kg/m2 and in men -26.8 kg/m2, (P>0.05) and with diabetes – 27.9 kg/m2 (in women – 28.5 kg/m2 and men – 27.2 kg/m2; (P>0, 05).
|
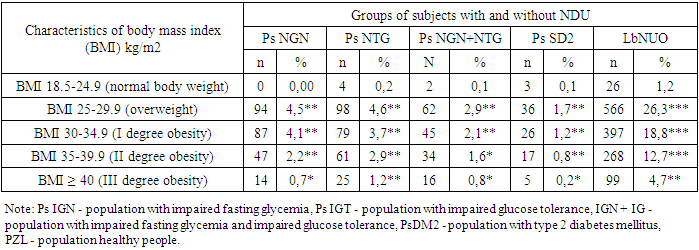
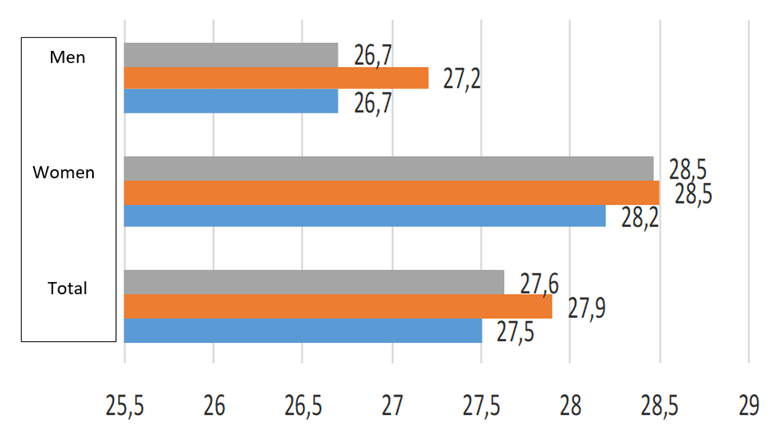 | Figure 1. Risk of developing glycemic disorders depending on BMI in those examined |
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML