-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1063-1065
doi:10.5923/j.ajmms.20241404.54
Received: Mar. 21, 2024; Accepted: Apr. 15, 2024; Published: Apr. 19, 2024

Risk Factors for the Development of Diabetes in Khorezm Region
Bakhtiyarova Aziza Maksudbekovna
Student, Urgench branch of the Tashkent Medical Academy, Uzbekistan
Correspondence to: Bakhtiyarova Aziza Maksudbekovna, Student, Urgench branch of the Tashkent Medical Academy, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Given the emergence of new concepts of the etiopathogenetic mechanisms of the development of diabetes mellitus, there is a need to reassess the risk factors for the development of diabetes mellitus. When examining patients with diabetes mellitus in the Khorezm region, a tendency was established towards an increase in the number of patients, rejuvenation of diabetes mellitus and the development of diabetes with increased body weight among them. Exogenous (compliance with a healthy lifestyle) and endogenous (hereditary) risk factors for the development of diabetes mellitus were studied. Preference for fatty, floury, and sweet foods was noted in 39 children and adolescents (73.6%). The risk of developing diabetes for family members with type 1 diabetes is on average 7%. Relatives of the 1st degree of kinship (siblings, children, parents) have the maximum risk - from 2.5% to 7%.
Keywords: Diabetes mellitus (DM) type 1, DM 2, Adolescents, obesity (O.), Hereditary factor, Insulin resistance
Cite this paper: Bakhtiyarova Aziza Maksudbekovna, Risk Factors for the Development of Diabetes in Khorezm Region, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1063-1065. doi: 10.5923/j.ajmms.20241404.54.
1. Introduction
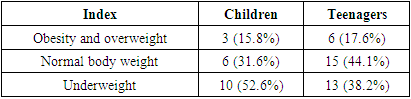
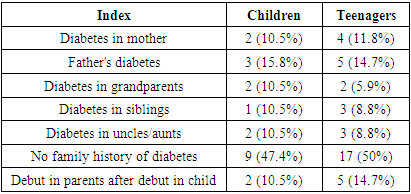
- Diabetes mellitus is called a global problem for humanity, since the disease places a heavy psychological and financial burden on the shoulders of sick people and their families, as well as national health care and economic systems [3]. According to statistics, every 5 seconds, 1 diabetic patient dies in the world; 4.6 million patients die annually; Every year more than 1 million lower limb amputations are performed in the world; more than 600 thousand patients completely lose their vision; about 500 thousand patients begin to receive renal replacement therapy due to end-stage renal failure [1].80-90% of patients suffer from type 2 diabetes mellitus, the leading pathogenetic factor of which is a hereditary factor. It is from this group of “conditionally healthy” individuals that the army of patients with diabetes mellitus is replenished annually by 15%. The proportion of the population with “metabolic syndrome” and obesity is rapidly increasing [2]. Their number already amounts to more than 400 million people, and by 2030 it will increase to 800 million people. Throughout its history, humanity has lived from hand to mouth and only in the last 40 years has there been food in abundance - this has played a big role in the development and spread of diabetes: our body was simply not ready for so many calories.Like throughout the world, the situation with diabetes in Uzbekistan deteriorating catastrophically. According to various estimates, the prevalence diabetes mellitus in the Republic of Uzbekistan ranges from 5 to 9%, while as of January 1, 2018, 230,610 patients with diabetes mellitus: 18,349 patients with diabetes mellitus type 1, and 212,261 patients with diabetes mellitus 2nd type, which is 650 per 100 thousand population [8]. According to the latest data, in Uzbekistan the number of patients with diabetes mellitus is more than 245 thousand, of which more than 2,300 are children and 879 teenagers. In addition to the financial burden, diabetes carries a heavy psycho-emotional burden for parents of sick children. It is known that the genetic factor plays a significant role in the prevalence of this pathology, since patients diabetes mellitus are able to maintain reproductive health with good compensation, but children born to them have a risk of inheriting diabetes. Type 1 diabetes mellitus is not a hereditary disease with monogenic inheritance of genes that have mutations that determine carbohydrate metabolism disorders. There is an opinion among researchers that the cause of type 1 diabetes is not genetic, but environmental (diabetes is more common in countries with unfavorable environmental conditions) and epigenetic [1]. Scientist Dirk Pohl discovered that in identical twins with diabetes, it was not the DNA that was damaged, but its protein “wrapper” - the membrane. It is natural factors that change the protein structure of DNA and force the immune system to attack pancreatic cells. Significant population genetic studies conducted by the Institute of Molecular Genetics of the Academy of Medical Sciences have established that the contribution of genetic factors to its development reaches 80% [3]. Scientists have been able to establish that more than 20 loci on various human chromosomes are linked to type 1 diabetes mellitus. The search for genes predisposing to the development of the disease should be carried out taking into account the multiplicity of these genes, as well as environmental factors. Currently, type 1 diabetes mellitus is classified as a multifactorial disease. [6]. Increasingly, researchers are talking about an increase in the incidence of type 2 diabetes among children and adolescents [7]. According to the authors, 80% of cases of diabetes in children and adolescents are type 1 diabetes mellitus; in the remaining cases, type 2 diabetes mellitus or secondary diabetes mellitus is diagnosed. In both cases, the leading pathogenetic factors are heredity and environmental factors [4,14].The main pathogenetic link in the development of type 2 diabetes mellitus is insulin resistance (IR) [3,13]. When type 2 diabetes mellitus or other carbohydrate metabolism disorders (impaired fasting glycemia and impaired glucose tolerance) are combined with excess weight, dyslipidemia, hyperuricemia and hypertension, i.e. with the main components of the metabolic syndrome, the detection rate of IR is almost 95% [8,12]. The study of the development of IR in various populations has shown that it is a combination of two components: genetic (hereditary) and acquired.Target: Studying the influence of exogenous and endogenous factors on the development of diabetes mellitus in the Khorezm region.Tasks1. Studying the influence of endogenous factors on the development of diabetes mellitus in children and adolescents in the Khorezm region2. Study of hereditary factors in children and adolescents with diabetes mellitus3. Study of predictors in individuals with a high absolute risk of developing diabetes mellitus
2. Materials and Methods
- 53 patients with type 2 diabetes mellitus were examined: 34 adolescents and 19 children hospitalized at the Khorezm branch of the Republican Scientific Medical Center of Endocrinology (clinical examination, anthropometry, laboratory tests). In order to study the predictors of the development of diabetes mellitus, a survey of patients and their parents and relatives was conducted: first of all, patients were interviewed about the inheritance of diabetes. Family nutrition traditions and attitudes towards a healthy lifestyle (HLS) have been studied in detail.
3. Results and Its Discussion
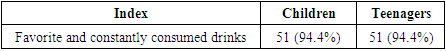
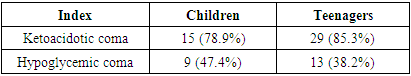
- Exogenous factors include dietary preferences, eating behavior, daily routine, and lifestyle. The issue of consumption of sweet drinks was studied separately: the vast majority of both children and adolescents – 51 (94.4%)% – called them their favorite and constantly consumed drinks.
|
|
|
|
4. Conclusions
- 1. Exogenous factors are of great importance in the development of diabetes mellitus both among children and adults. It is in families that have no idea about a healthy lifestyle that the prevailing number of patients with diabetes has been identified. Preference for fatty, floury, and sweet foods was noted in 39 children and adolescents (73.6%). Only 6 adolescents (26.4%) noted that they had an idea about rational nutrition and tried to adhere to a healthy lifestyle.2. In “nuclear” families, i.e. In families with one or more close relatives suffering from type 1 diabetes, the risk of developing diabetes in the offspring of this family increases. The risk of developing diabetes for family members with type 1 diabetes mellitus is on average 7%. Relatives of the 1st degree of kinship (siblings, children, parents) have the maximum risk - from 2.5% to 7%. Children born to fathers have a greater risk than children born to mothers with type 2 diabetes (3.6-8.5% versus 1.1-3.6%).3. The risk of developing type 2 diabetes mellitus in close relatives of patients is on average 40%, which indicates the familial nature of this disease. In sick children, the risk is 50% if the father is sick, and 35% if the mother is sick. Concordance for type 2 diabetes mellitus in identical twins reaches 80%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML