Tokhtaev B. U.1, Yusupov A. A.2
1Director of the Samarkand Branch of the Republican Specialized Eye Microsurgery Scientific and Practical Medical Center, Uzbekistan
2Professor of Ophthalmology Department of Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Contraindications to drugs of different pharmacological groups - instructions are not repeated in different groups, which makes it possible to choose treatment measures based on concomitant diseases in a particular patient. In patients with primary open-angle glaucoma, laser trabeculoplasty is a procedure with a significantly higher rate of effective intraocular pressure reduction in eyes with thinner corneas after surgery. The only factor that indicates the effectiveness of laser trabeculoplasty is the initial high level of intraocular pressure.
Keywords:
Glaucoma, Laser trabeculoplasty, Tonometry, Intraocular pressure
Cite this paper: Tokhtaev B. U., Yusupov A. A., Clinical Effectiveness of Laser Trabeculoplasty Surgery in Ophthalmology Practice, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1028-1032. doi: 10.5923/j.ajmms.20241404.47.
Article Outline
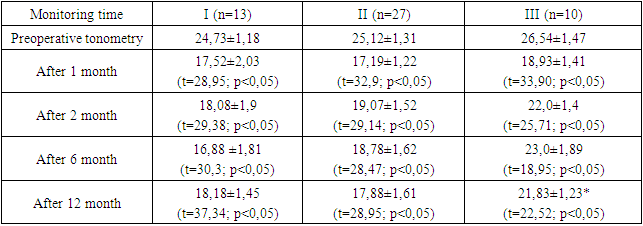
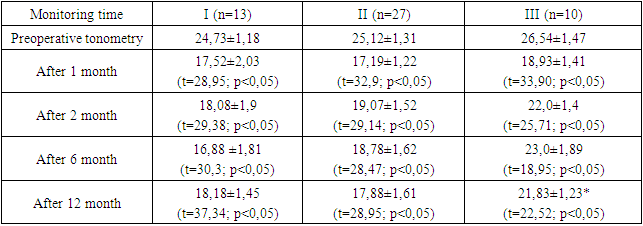
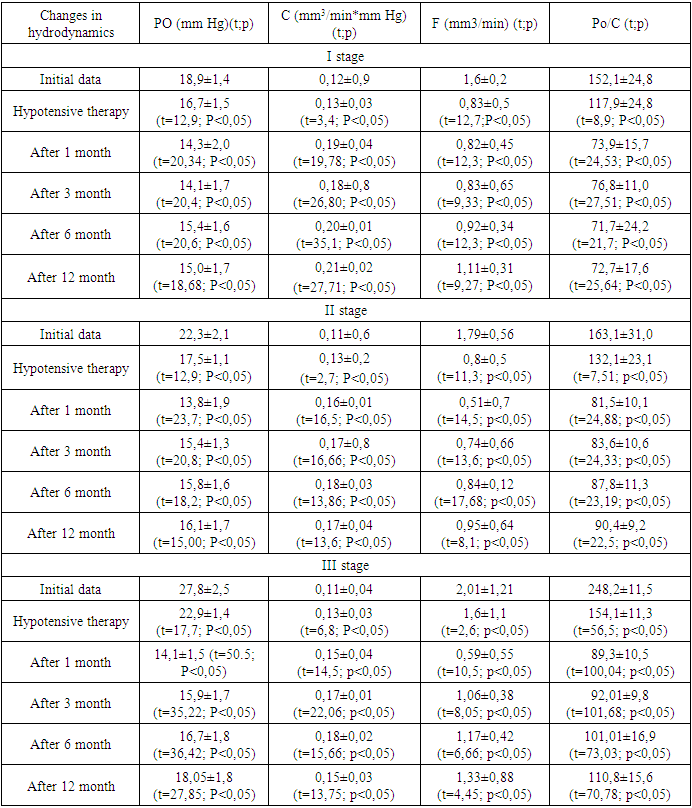
In our increasingly developed modern society, the search for new information on the etiopathogenesis of glaucoma is becoming a pressing issue today due to the increasing proportion of elderly people in the population of countries around the world. With medical advances, lifestyles are improving at the same time that the world population is growing and the risk of visual impairment due to population ageing is increasing. Between 2000 and 2010, the increase in the number of ophthalmic patients was 4-5% of the world population, with an annual increase of 7%. Rejuvenation in diseases such as cataract and glaucoma is a process that is receiving special attention. Today, 30-35 year olds with these diseases can be found in the world population [2,8,10]. According to a study conducted in the United States in 2011, 2.71 million people in the United States had eye disease, and these patients were between the ages of 70 and 79 (31 per cent). The Academy of Ophthalmology estimates that by 2050, 7.32 million people in the United States could have eye disease [1,7,9]. Due to demographic changes in Asian countries, the number of people in need of eye care services was 437 million in 2010, and this figure could rise to 827 million by 2030 [3,6].Different follow-up results of patients who underwent selective laser trabeculoplasty at different follow-up periodsPatients who underwent selective laser trabeculoplasty surgery were dripped non-steroidal anti-inflammatory drugs into the operated eye for immediate prophylaxis. To prevent possible complications, these drugs were administered in specific doses to all 50 patients for a week after surgery. On the first day after surgery 2 patients (4%) had mild hyperaemia of the conjunctiva of the eye, a condition that lasted for 5-6 days, and the patient's sensation of foreign body in the eye disappeared. This condition was eliminated without the use of additional therapeutic measures. However, on the first day after the procedure of selective laser trabeculoplasty 3 (6%) patients had reactive intraocular pressure 5.3±1.0 mm. Hg. No further complications after the operation were revealed.The patients were followed up for one year after selective laser trabeculoplasty surgery in the following order:Stage 1 - selective laser trabeculoplasty before surgery;Stage 2 - up to 1 month after the operation;Stage 3 - from 1 to 3 months after SLT surgery;Stage 4 - 3 to 6 months after SLT surgery;Stage 5 - from 6 months to 1 year after SLT surgery.Clinical efficacy of the surgical procedure of selective laser trabeculoplasty was determined by three main functional indices: normalisation of intraocular pressure, stabilisation of visual field acuity.Table 1. Tonometric parameters in patients undergoing SLT surgery
 |
| |
|
The results of periodic tonometry are plotted in Figure 1. The presented data reflect the reliability in 95% of cases. As can be seen from this figure, all stages after SLT surgery are characterised by a statistically significant decrease in intraocular pressure (p <0.05). Stability of intraocular pressure was found to be maintained in stages I and II of the disease. In stage III of the disease, a statistically significant increase in IOP was observed 3 months after SLT surgery (p<0.05); when patients in this group were examined one year later, a significant decrease in IOP was found. It was found that the differences between the groups divided by disease stages were significant (p<0.05).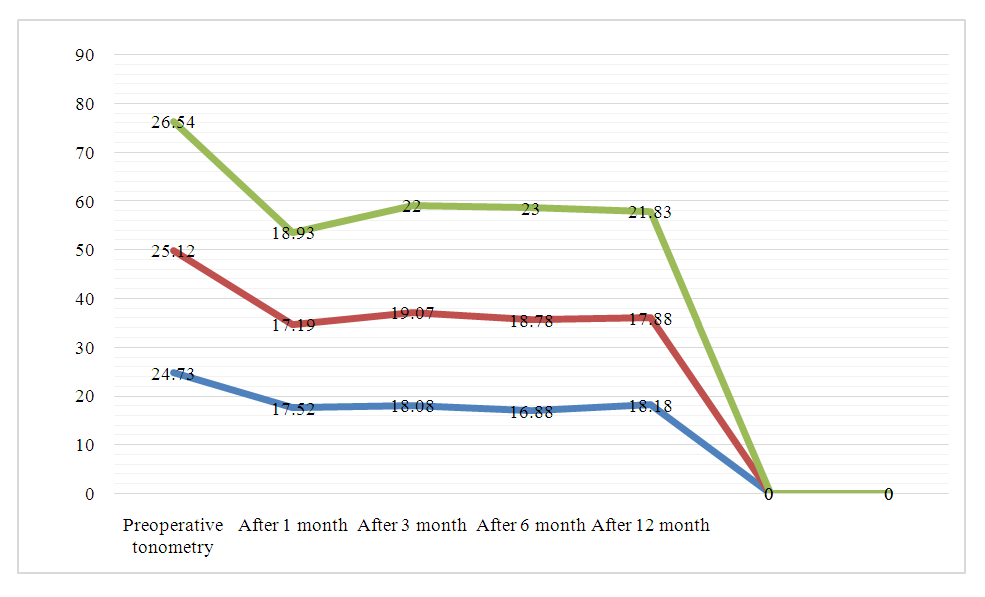 | Figure 1. Dynamics of periodic tonometry |
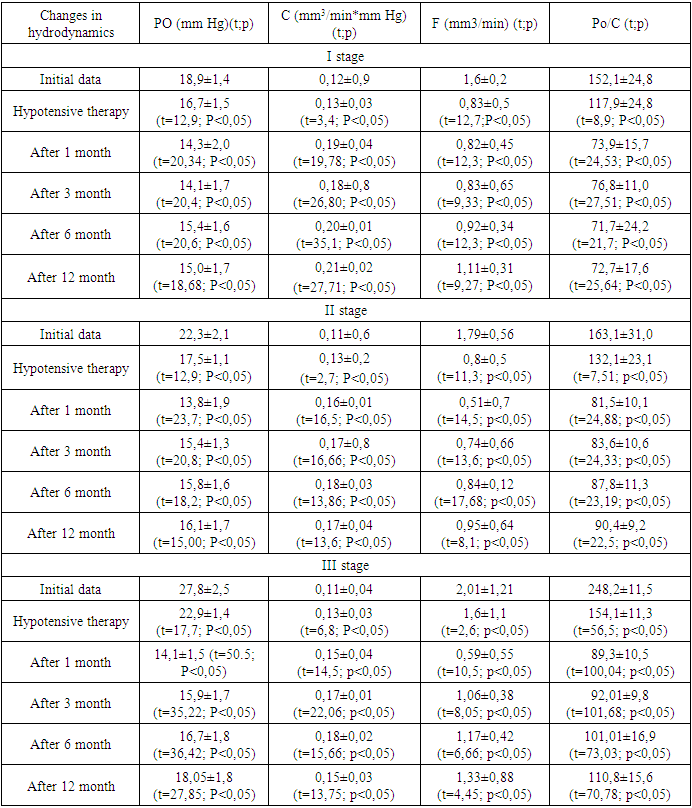
At 6 months after the selective laser trabeculoplasty surgery in patients who were in stage III of the disease and receiving combined antihypertensive therapy, an increase in intraocular pressure was noted in 4% of cases. Two patients underwent repeat selective laser trabeculoplasty to reduce intraocular pressure in these patients and stabilise the course of the disease. According to the results of nonparametric analysis of variance, statistically significant trends (P<0.05) in their improvement were observed.Table 2 shows the changes in ocular hydrodynamics in the group of patients who underwent SLT surgery at different stages of the disease. According to the results of the analysis, statistically significant trends (p<0.05) were observed in positive data.Table 2
 |
| |
|
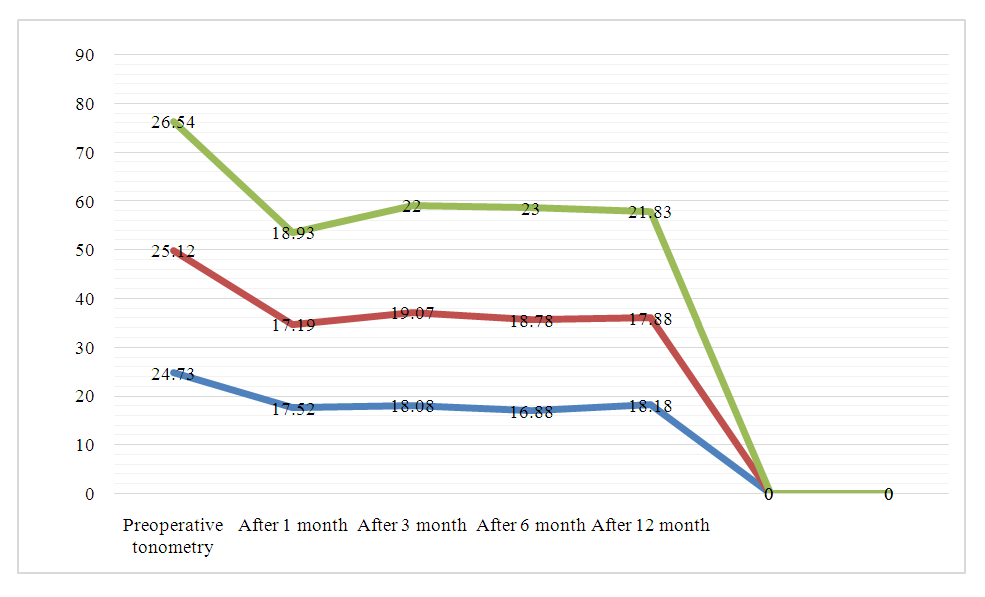
Although there are many hypotensive agents currently available in practical medicine to lower IOP, conservative treatments have low efficacy because there are several factors affecting treatment. Factors such as patients' refusal to use eye drops, the high cost of medication, and the decreasing effectiveness of medication reduce the effectiveness of treatment. Under these circumstances, achieving normal IOP becomes impossible, which creates a number of problems in clinical trials. Currently, the treatment of glaucoma by selective laser trabeculoplasty is of great interest. Evidence for the use of selective laser trabeculoplasty in surgery was reported in 1995-1996 by Mark A. Latina and is evident in the papers of his co-authors. Samara Regional Ophthalmological Hospital of the Russian Federation staff Al.O. Turutina, A.S. Malyshev, A.O. Turutina, A.V. Fadeeva's study for 36 months revealed the advantages of selective laser trabeculoplasty. Al.O. Turutina, A.S. Malyshev, A.O. Turutina, A.V. Based on the results of Fadeeva's follow-up of 36 months, it was found that selective laser trabeculoplasty surgery was the most effective method in patients with stage I-II glaucoma (53.3% and 41.1%, respectively). In these groups a reduction or complete cessation of the use of IOP-lowering eye drops was achieved In primary open-angle glaucoma stage III, if it is impossible to prescribe a surgically curable procedure to the patient, the procedure of selective laser trabeculoplasty can be used as an auxiliary method. Also it should be separately noted that in some patients during the long period of observation IOP is on the average 6±1.3 mm higher than the initial value. This condition is insufficient to achieve target pressure in stage III glaucoma.There were no statistically significant cases of acute visual changes at stages I, II and III of the disease (n > 0.05). Figure 2 clearly shows the dynamics of visual acuity at different stages. The results reflect arithmetic mean values, probability errors indicate the reliability of the results obtained in 95% of cases.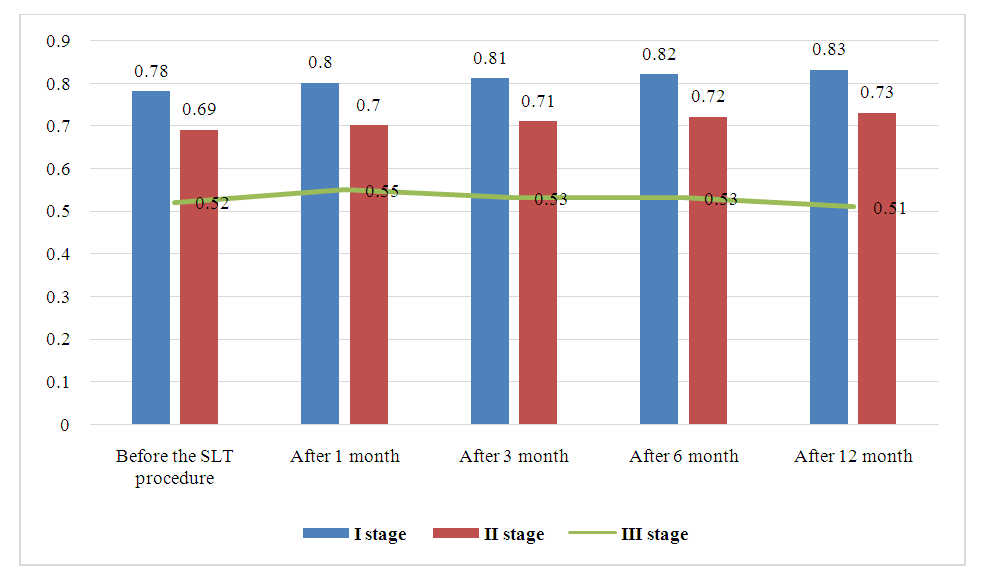 | Figure 2. Dynamics of visual acuity at different stages of the disease |
When analysing the optical cohort tomography readings within 12 months after the procedure of selective laser trabeculoplasty performed for therapeutic purposes, no negative dynamics of the results was revealed. It was found that (P>0.05) recorded in patients with stage I and II open-angle glaucoma was reliable. A year and a half after the first laser surgery, the patients with stage III disease who underwent reoperation and then achieved the desired IOP were 2. After the selective laser trabeculoplasty procedure, the postoperative period remained stable, no statistically significant difference between preoperative and postoperative values (p>0.05) was found.Thus, statistically significant reduction of intraocular pressure in patients was observed at all stages after selective laser trabeculoplasty procedure (p<0.05). In stages I and II, a stably maintained IOP level was observed, not exceeding the target pressure value. Intraocular pressure was found to be a statistically significant parameter (p<0.05) for elevation in stage III open-angle glaucoma. Differences in IOP levels between groups were statistically significant (p<0.05).No significant improvement of visual acuity at all stages of the disease was revealed (n>0.05). An encouraging case was the recurrence of statistically significant (p<0.05) positive dynamics of changes in the general boundaries of the visual field in patients with open angle glaucoma stages I, II and III. In all groups there was a significant recurrent difference in the stages of the disease (p<0.05). When analysing the parameters of visual acuity during 12 months of selective laser trabeculoplasty practice in all patients with stages I and II of open angle glaucoma no negative dynamics was revealed, in patients with stage III of the disease no statistically significant differences were found (p>0,05).Assessment of quality of life after selective laser trabeculoplasty procedure in patients with glaucomaUsing the selective laser trabeculoplasty technique, 200 patients aged 40 to 78 years were recruited, of which 150 patients underwent laser surgery (in 150 eyes), 96 of these patients are female (48%) and 104-male (52%). In all 200 patients (200 eyes), the anterior chamber angle during gonioscopy was open and of medium width. According to the severity of trabecular pigmentation, the patients were divided into 4 groups: mild (I) in 58 pairs of eyes, moderate (II) in 78 pairs of eyes, pronounced (III) in 42 pairs of eyes, and severely pronounced (IV) in 22 pairs of eyes. For all questions in the NEI VFQ - 25 questionnaire in patients at all stages after the selective laser trabeculoplasty procedure, the results of the open-angle glaucoma patient questionnaire evaluation were obtained.The condition of all patients who underwent selective laser trabeculoplasty was assessed using the following questions in the NEI VFQ - 25 questionnaire: how often do you feel pain or discomfort in the patient's eye area? (itching, eye pain, spreading pain). This survey found an improvement in patients' quality of life after the selective laser trabeculoplasty procedure. The survey showed that 8.0 per cent of patients did not experience "eye pain or discomfort" before SLT. Two years after SLT surgery, 30% (X2 = 42.3 P < 0.001) of patients did not experience severe eye pain. " Occasionally observed pain " was 32.0% before SLT, while this decreased to 16% after surgery (X2=12.7; P<0.001). " Pain observed most of the time " - 32% before surgery (X2=31; P<0.001) - while this rate decreased to 8.1% after surgery. " Very frequently observed pain " - was 18% preoperatively and 1% (X2=32.6; p<0.001) one year after this operation."How difficult is it to read simple notes in newspapers and magazines? "While before selective laser trabeculoplasty surgery 8% of patients responded, "I have no problems," one year after SLT surgery this was found to decrease to 16% (X2=4.8; P=0.017). To the above question, 14% responded that" on very rare occasions I have problems " before surgery, and after surgery this rate decreased to 26% (X2=5.8; P=0.013) and the positive result was a relapse. Patients who responded:" very difficult to read" decreased from 22% to 14% before SLT (X2=1.5; P=0.122). These data above indicate an improvement in patients' quality of life.Using the question" how difficult is it for you to perform everyday activities that require very clear vision (cooking, sewing, housework, using various tools)", a positive trend was also observed:" I never have difficulties " - 17.2% responded before. surgery and 56.18% (X2=80.1; P<0.001) responded after; "sometimes I experience this difficulties " - 43.2% responded before SLT and 17.93% (x2=36.5; p<0.001) after surgery; the number of" very difficult " responses decreased from 15.6% to 8.4% (X2=5.5; p=0.019)."How difficult is it for you to read notes with street or shop names?" when asked "why?". 26.0% of patients never had difficulty before surgery and 45.8% (X2=20.4; P<0.001) after surgery; 34.0% of patients sometimes had difficulty before surgery and 21.7% (X2=8.8; P=0.003) after surgery; 19.2% of patients had difficulty before SLT and 16.9% (X2=0.3; p=0.581) had great difficulty 12 months after surgery. The question: "how difficult is it to notice things that are far away from you due to visual impairment? " shows an improvement in patients' quality of life: the proportion of patients who never had difficulties increased from 26.0 to 47.2% (X2=23.3; P<0.001); those who sometimes had difficulties decreased from 32.8 to 19.2% (X2=11.3; P=0.001); their vision prevented them from noticing objects far away from them. the number of patients also decreased from 6.4% to 2.4% (x2=3.9; p=0.05)."How difficult is it to distinguish and choose the clothes you want to wear when going out because of visual impairment?" to the questions " why?" and " how difficult is it to go to parties, parties or restaurants because of visual impairment? The number of responses" I never had difficulty "ranged from 57.2 to 77.7% (X2=23; P<0.001) and 55.2 to 57.6% (or=1.1; CI=0.8 to 1.6; X2=0.2; P=0.652) respectively, and the number of responses" sometimes I had difficulty it decreased from 16.8 to 9.6% (x2=5; p=0.025) and from 22.0 to 13.2% (X2=6.1; p=0.014) respectively."How difficult is it to work at a computer for long periods of time due to reduced visual acuity? "and" how difficult is it for you to read small text on food labels, medications, and receipts if you use glasses or contact lenses? the number of responses" I never have difficulty "ranged from 6 to 12% (X2=6.9; P=0.005) and 10 to 18% (X2=6.4; P=0.001); the number of responses" very difficult" ranged from 18.0 to 10.0%. (X2=4.7; P=0.03), and the number of responses to the second question ranged from 26 to 20% (X2=4.6; P=0.031), which returned positive results.These indicators, accordingly, confirm the improvement in patients' quality of life after SLT surgery.The number of patients who never had problems with shaving, styling or make-up, or recognising people's faces, increased from 40.0% to 64.0% (X2=28.0; P<0.001), respectively. A similar trend stated, "how difficult is it for you to watch television because of decreased vision? "28% of patients before SLT and 44% of patients one year after surgery patients never had problems (X2=12; P <0.001)."Do unpleasant sensations such as itching or eye pain interfere with your activities? "before surgery, 18% of patients answered" never", and after surgery increased to 58% (X2=71.8; P<0.001).The number of patients who answered" never "to the question" do you need help from others because of vision loss" increased to 32 and 52% (x2=16.2; p<0.001). Those who answered "Most of the time" decreased to 16 and 6% (x2=6.2; p=0.01) respectively. These results prove the improvement of the patients' quality of life.The number of patients with the best visual assessment increased from 2 to 8% (X2 = 7.6; P = 0.002) one year after selective laser trabeculoplasty.The data obtained in the course of our research indicate that the results of clinical efficacy and stabilisation of intraocular pressure after selective laser trabeculoplasty surgery are consistent with the data presented in many foreign literatures [4,5].The NEI/VFQ-25 all-question questionnaire found that patients' quality of life improved one year after selective laser trabeculoplasty surgery.
References
| [1] | Ashan H. et al. Profil Pasien Glaukoma pada Lansia di Rumah Sakit Khusus Mata (RSKM) Padang Eye Center Tahun 2021 // Scientific Journal. – 2022. – Т. 1. – №. 5. – С. 354-362. |
| [2] | Burhani H. R., Fitri I., Andrianingsih A. Perbandingan dan Certainty factor pada Sistem Pakar Untuk Mendiagnosa Dini Penyakit Glaukoma // Jurnal JTIK (Jurnal Teknologi Informasi dan Komunikasi). – 2021. – Т. 5. – №. 3. – С. 291-299. |
| [3] | US Eye Disease Statistics.: https://www.aao.org/eye-disease-statistics. Ссылка 14 ноября 2019. |
| [4] | World Health Organization et al. The world health report 2008: primary health care now more than ever. – World Health Organization, 2008. |
| [5] | Zheng Y. et al. How much eye care services do Asian populations need? Projection from the Singapore Epidemiology of Eye Disease (SEED) study // Investigative ophthalmology & visual science. – 2013. – Т. 54. – №. 3. – С. 2171-2177. |
| [6] | Ma A., Stephanie W. Y., Wong J. K. W. Micropulse laser for the treatment of glaucoma: a literature review // Survey of ophthalmology. – 2019. – Т. 64. – №. 4. – С. 486-497. |
| [7] | Lusthaus J., Goldberg I. Current management of glaucoma // Medical Journal of Australia. – 2019. – Т. 210. – №. 4. – С. 180-187. |
| [8] | Lestak J. et al. he Visual Field in Normal Tension and Hyper Tension Glaukoma // Clinical Research. – 2014. – Т. 3. – №. 12. |
| [9] | Korneeva A. M. Classification of methods of clinical and economic analysis // News of the Institute of Management Systems of SSEU. – 2018. – No. 1. – pp. 260-263. |
| [10] | Kremkova E. V., Novoderezhkin V. V., Rabadanova M. G. Features of new possibilities for laser correction of primary open-angle glaucoma // Clinical gerontology. – 2016. – T. 22. – No. 9-10. – pp. 41-42. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML