-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1022-1024
doi:10.5923/j.ajmms.20241404.45
Received: Apr. 3, 2024; Accepted: Apr. 15, 2024; Published: Apr. 18, 2024

Comparison of Routine Ligation of the Great Vessels of the Uterus after Cesarean Section with a Group without Ligation
Inoyatova N. M., Asatova M. M., Jalalov U. D.
Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

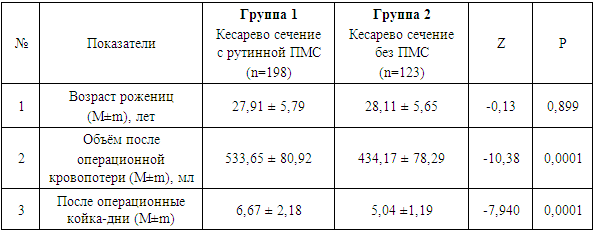
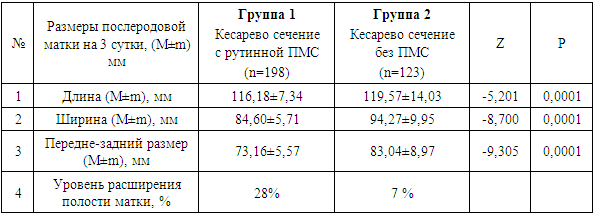
Postpartum hemorrhage (PPH) is a serious obstetric problem in the world and in our country. Due to the high incidence of PPH, especially during cesarean section, routine ligation of the great uterine vessels (GVL) during cesarean section has been suggested by national experts. The purpose of our study was to compare the results of a pilot facility with routine PMS during cesarean section with a facility that does not. In 2022, a pilot was carried out in one of the obstetric complexes, where 198 birth stories were randomly selected according to routine PMS. In another obstetric complex, 123 birth histories without routine PMS were randomly selected. The average age of patients in group 1 was 27.91 ± 5.79 years, in group 2 – 28.11 ± 5.65 years. The volume of blood loss in group 1 was 533.65 ± 80.92 ml, which was on average 100 ml more than in the group without ligation and amounted to 434.17 ± 78.29 ml. The average bed day in group 1 was 6.67 ± 2.18 days versus 5.04 ± 1.19 days in group 2. Analysis of the involution of the uterine cavity from dilated with inclusions to closed showed that in the group where routine PMS was performed, it occurred in 28% than without it in 7%. Routine PMS during cesarean section is an unreasonable procedure that increases the amount of intraoperative blood loss, operation time, length of stay in the clinic, as well as the risks of postpartum complications.
Keywords: Cesarean section, Prevention of postpartum hemorrhage, Ligation of the great vessels of the uterus, Uterine involution
Cite this paper: Inoyatova N. M., Asatova M. M., Jalalov U. D., Comparison of Routine Ligation of the Great Vessels of the Uterus after Cesarean Section with a Group without Ligation, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1022-1024. doi: 10.5923/j.ajmms.20241404.45.
1. Relevance
- Postpartum hemorrhage (PPH) is a serious obstetric problem and continues to be the most common cause of maternal mortality and morbidity both in the world and in our country [8]. According to the 4th confidential report in 2018–2020. in our country, the first place among the causes of maternal mortality (MS) was obstetric hemorrhage amounting to 29.1%, the intensive rate of MS from obstetric hemorrhage was 5.4 per 100,000 births [5]. Morbidity and mortality increase not only with delays in diagnosis and treatment, but also with any increase in cesarean section rates. Currently, the main tactic for surgical treatment of PPH during cesarean section is organ-sparing tactics. Such conservative methods of surgical control of obstetric hemorrhage include ligation of the great vessels of the uterus (GV) or internal iliac arteries, application of compression sutures or embolization of the uterine vessels, up to postpartum hysterectomy [2,3,4,6,7,8]. Due to the high incidence of postpartum hemorrhage, especially during cesarean section, national experts have proposed routine ligation of the great vessels of the uterus during cesarean section, and some experts have suggested prophylactic ligation only in high-risk groups [1]. Despite the fact that, according to WHO recommendations and existing national guidelines, this tactic is recommended only in the surgical hemostasis algorithm [3,4,8].The purpose of our study was to compare the results of a pilot institution with routine ligation of the great vessels of the uterus during cesarean section with an institution that does not practice this.
2. Materials and Methods
- In 2022, piloting was carried out in one of the obstetric complexes. In an obstetric complex that practices routine ligation of the great vessels of the uterus after cesarean section, a 5% randomized sample of 4203 histories of operative deliveries for emergency and planned indications was performed for the 2022 calendar year. The selection of stories was done in random order. From the total population of caesarean sections performed during the year in this institution, 210 cases were randomly selected (using the random number function in Excel). During the sampling process, 12 stories with insufficient documentation were excluded; a total of 198 birth stories were studied (group 1).In another obstetric practice that does not routinely perform ligation of great vessels after cesarean section, a 5% randomized sample of 3020 histories of operative deliveries for emergency and elective indications was performed for the 2022 calendar year. The selection of stories was done in random order. From the total population of caesarean sections performed during the year in this institution, 151 stories were selected in random order (using the random number function in Excel). During the sampling process, 28 stories with insufficient documentation were excluded, and a total of 123 birth stories were studied (group 2).When studying birth histories, the woman’s age, length of hospital days, volume of intraoperative blood loss were analyzed; to study uterine involution, the biometric dimensions of the uterus were assessed on the 3rd day using transabdominal ultrasound (length, width and anteroposterior size of the uterus), the uterine cavity was assessed and its contents.Statistical data processing was carried out on a Pentium-4 type PC using standard software tools “MS Excel”, “SPSS-22”, which ensure the effective use of mathematical statistics methods. Due to the fact that the variation series had an uneven distribution (determined by the Kolmogorov-Smirnov test), a significant difference between the two groups was determined by non-parametric methods using the Mann-Whitney U test, and correlation analysis was carried out using the Spearman rank correlation coefficient rs.
3. Research Results
- All women from 2 groups were of active reproductive age from 19 (18 years in group 1) to 44 years. The average age of patients in group 1 was 27.91 ± 5.79 years, in group 2 – 28.11 ± 5.65 years. It should be noted that the rate of planned cesarean sections was higher in group 2 than in group 1 (26.8% versus 7.5%). All women in labor in the 1st group underwent routine ligation of the great vessels of the uterus, while in the 2nd group this surgical intervention was performed only according to strict indications. 5 (4%) women from group 2 underwent ligation of the great vessels for surgical reasons in order to enhance hemostasis. In each group, one hysterectomy was performed for surgical indications, which was 0.5% in the first group and 0.8% in the second group.The volume of blood loss in the group with routine PMS was 533.65 ± 80.92 ml, which is on average 100 ml more than in the group without PMS, where the volume was 434.17 ± 78.29 ml.This intervention led to an increase in the mother's stay in the postpartum department of the obstetric complex by an average of 1.63 days due to the fact that in the postpartum period the contraction of the uterine cavity and the outflow of contents were reduced. The average bed-day of stay for women in labor in group 1 was 6.67 ± 2.18 days versus 5.04 ± 1.19 days in group 2 (Table 1).
|
|
4. Conclusions
- Obstetric hemorrhage is a fairly serious pathology that can develop in any woman during pregnancy and especially in the postpartum period. In this regard, the readiness to provide prompt assistance in stopping bleeding in the postpartum period is decisive in preventing further obstetric complications. To stop bleeding, it is necessary to follow a clear algorithm, which includes conservative and surgical methods. Surgical methods of hemostasis are divided into organ-preserving methods, such as ligation of the uterine vessels and others, and at the final stage this is hysterectomy [3,4,7,8]. All these steps are recommended for bleeding, the volume of which should be 1000 ml or more during a cesarean section or in the presence of clinical signs of hemorrhagic shock.In this regard, routine ligation of the great vessels during cesarean section is an unreasonable procedure that increases the amount of intraoperative blood loss, operation time, length of stay in the clinic, as well as risks in the postpartum period.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML