Arziev I. A., Rustamov S. U.
Samarkand State Medical University, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The results of the examination and treatment of 341 patients with acute cholecystitis were analyzed. In the conditions of the Charlson multimorbidity index (3.20 - 3.31) for acute cholecystitis in elderly and senile patients, the high surgical and anesthesiological risk P3, P4 reaches 76.2% (according to the ASA scale) and 69.8% (according to the APACHE scale II), which dictates the priority of minimally invasive interventions at the stages of treatment. The use of minimally invasive puncture-drainage, laparoscopic and endoscopic techniques, taking into account the surgical and anesthetic risk according to ASA, APACHE II and the Charlson comorbidity index, allows for timely completion of the necessary treatment procedures, reducing the number of postoperative complications from 19.7% to 6.4%, postoperative mortality from 6.7% to 1.9%, as well as reduce the length of inpatient treatment by an average of 5.5 bed days.
Keywords:
Acute cholecystitis, Surgical and anesthesiological risk, Surgical tactics
Cite this paper: Arziev I. A., Rustamov S. U., Differentiated Surgical Tactics in the Treatment of Patients with Acute Cholecystitis with High Operational Anesthetic Risk, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1016-1021. doi: 10.5923/j.ajmms.20241404.44.
1. Introduction
Despite the increased quality of surgical care for the population over the past two decades, acute cholecystitis is one of the most common diseases of the abdominal cavity, especially in groups of elderly and senile patients with a high operational and anesthetic risk. Overall mortality has been at approximately the same level over the past 10 years and varies, depending on the proportion of destructive forms of the disease, within 5-8%. At the same time, the mortality rate in severe forms of acute cholecystitis remains very high and reaches 12-15%.A peculiarity of the condition of almost all elderly and senile patients is the presence of concomitant pathology, often of a systemic nature, and with the development of an acute inflammatory process, the process is layered on the main pathology, which further increases the surgical and anesthetic risk. Often the course of the main and concomitant diseases mutually aggravate each other, competing with each other. The main place is occupied by the pathology of the cardiovascular system, 50-60% of patients have a history of diseases of the respiratory system. More than half of the patients have a history of diabetes mellitus; such a number of patients are overweight, often grade 3-4 (30-60%).The above points to the need for timely diagnosis of gall bladder destruction, further study and improvement of surgical treatment of acute cholecystitis in elderly and senile patients using minimally invasive surgery, which will reduce postoperative mortality in this group of patients.
2. Purpose of the Research
Improving the results of treatment of patients with acute cholecystitis with a high operational and anesthetic risk through a differentiated choice of method of surgical correction with priority use of minimally invasive interventions.
3. Materials and Methods of Research
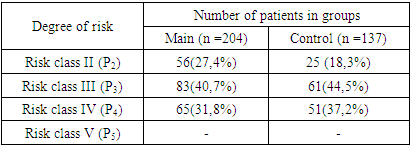
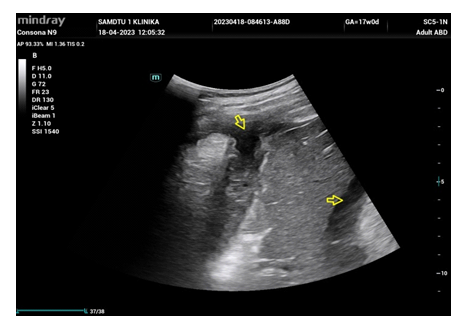
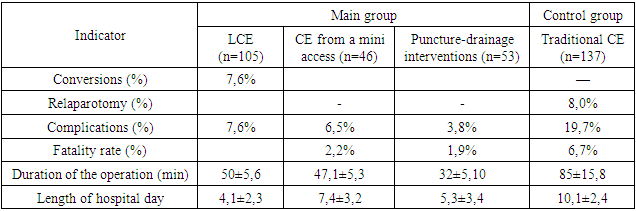
The results of the examination and treatment of 341 patients with acute cholecystitis who were treated in the surgical departments of the multidisciplinary clinic of Samarkand State Medical University in 2016-2023 were analyzed. 137 patients (comparison group) were operated on using laparotomy access, 204 (main group) surgical interventions were performed using minimally invasive techniques. Of these: 53 patients underwent puncture-drainage interventions under ultrasound guidance, 105 laparoscopic, 46 CE from minilaparotomy access.All patients were over 60 years of age and were divided into age categories of 60-74 years (elderly) - 296 (86.8%) and 75 years and older (senile age) - 45 (13.2%), long-livers (90 years and older) were not included in the study. Patients had a history of 2 to 5 concomitant general somatic diseases.The criteria for the study were clinical and ultrasound signs of acute cholecystitis, the presence of signs of systemic inflammatory response syndrome (fever, leukocytosis, and others), the presence of surgical and anesthetic risk (class P2, P3, P4 according to the ASA classification), the lack of a positive effect from conservative therapy in within 48 hours.All patients in the study had concomitant diseases, both compensated and mutually aggravating (comorbidity), which aggravated the course of the underlying disease, complicated decision-making in terms of the extent of surgery, as well as the course of the postoperative period.The comorbidity index in the comparison group was 3.31, and in the main group of the study it was 3.20, i.e. the indicators are identical. The index allows you to calculate the probability of death in conditions of comorbidity and with scores of 3-4, its probability according to the Charlson index is up to 52% in a given age category, which confirms the high surgical and anesthetic risk.All 341 patients diagnosed with acute cholecystitis underwent a sonographic examination of the gallbladder, surrounding tissues, organs of the hepatopancreatoduodenal zone and the abdominal cavity within 2 hours of the onset of hospitalization. According to the results of ultrasound examination, the average dimensions of the gallbladder were as follows: length - 119 ± 14.5 mm, width 38.6 ± 8.3 mm, in these cases there was an increase in the wall of more than 4 mm. During subsequent ultrasound examinations, special attention was paid to changes in the size of both the gallbladder itself and its wall; when assessing the nature of the contents, the alarming moment was the appearance of “hepatization” of it, which in all cases indicated the presence of infection in the lumen of the gallbladder.Ultrasound in the gray scale mode was performed in 100% of cases in our patients, and it was found that signs of acute cholecystitis were observed in 296 patients (86.8%), including 178 (87.2%) of 204 of the main study group.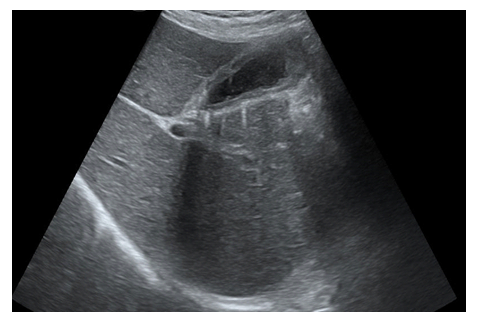 | Figure 1. Patient S., 46 years old. Sonogram: Acute destructive cholecystitis without extravesicular complications. "Double circuit" of the gallbladder wall |
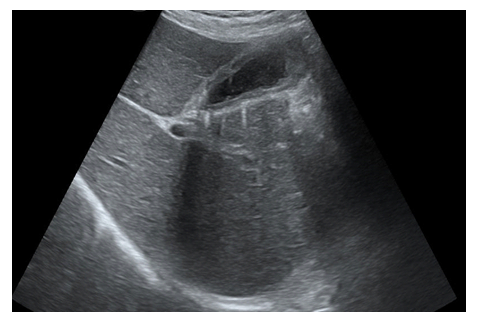
 | Figure 2. Patient A. 63 years old. Sonogram: Acute destructive cholecystitis with a perivesical abscess |
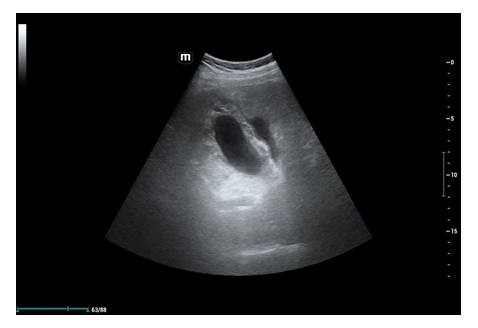
 | Figure 3. Patient Z., 51 years old. Sonogram: Gallbladder perforation with widespread peritonitis. Free fluid in Morrison's sinus |
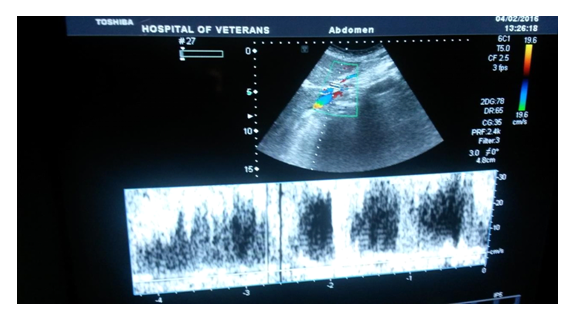
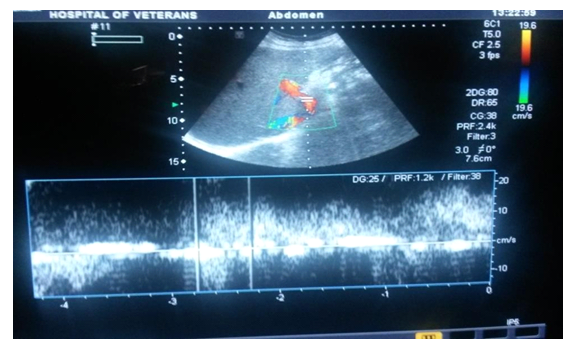
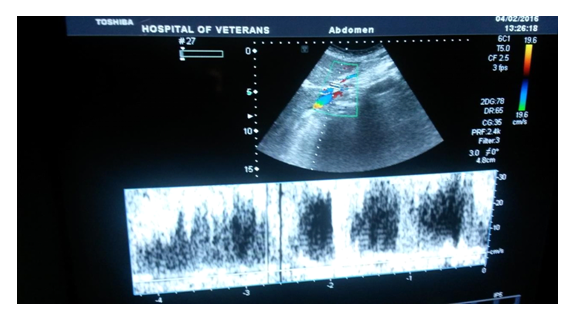
In 16.8% of cases in the main study group, the signs of acute cholecystitis were doubtful and therefore 26 patients underwent ultrasound dopplerography using color Doppler mapping and power Doppler in the unpaired branches of the aorta: the celiac trunk, the common and native hepatic artery and the cystic artery, which made it possible to clarify the presence the inflammatory process in the gallbladder and more clearly determine surgical tactics. At the same time, in patients, in the absence of ultrasound signs of acute destructive cholecystitis in the “gray scale” mode, there were changes in linear blood flow velocities in the celiac trunk basin towards an increase, which indicated a systemic inflammatory reaction in destructive cholecystitis in the stage of toxemia.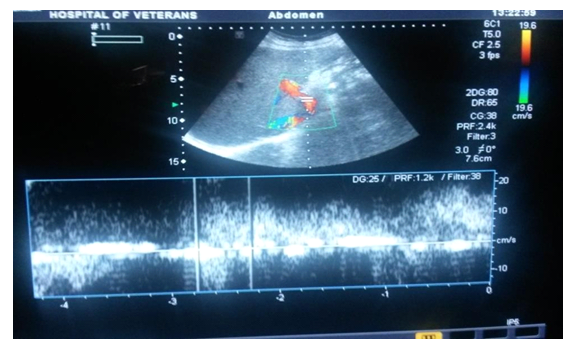 | Figure 4. Patient S., 68 years old. Ultrasonic triplex scanning in acute phlegmonous cholecystitis |
 | Figure 5. Patient A. 72 years old. Ultrasonic triplex scanning in acute gangrenous cholecystitis |
So, if the normal diameter of the celiac axis is 7.13±1.32; V.vol 1258.35±14.41; V.max min 100-105 m/s, then with destructive cholecystitis these figures increased accordingly: diameter 8.55±1.0; V.vol 1965.1 ± 27.24; V.maxmin 150-110m/s.The algorithm for diagnosing acute cholecystitis with the addition of ultrasound in the gray scale mode of color Doppler ultrasound increased the information content to 92.3% and made it possible to limit the use of expensive X-ray and radiological research methods.
4. Results and Discussion
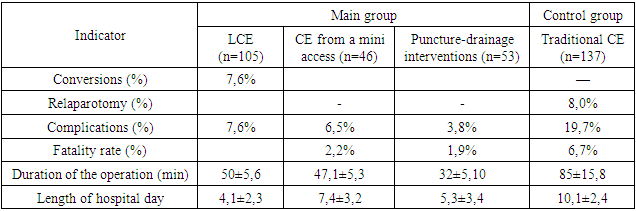
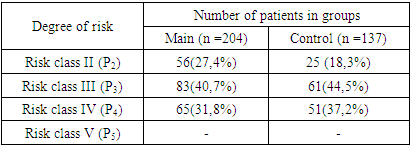
To determine surgical tactics, predict and prevent complications in the treatment of acute cholecystitis, a comprehensive assessment of the general condition of the patient was carried out. The use of the ASA classification is advisable when predicting the outcomes of all types of surgical interventions, and the patients were distributed according to the degree of surgical and anesthetic risk as follows. Table 1. Patient Distribution According to ASA Classification
 |
| |
|
40.7% of patients in the main group and 44.5% in the control group, 31.8% of patients in the main group and 37.2% in the control group, corresponded to risk class IV, i.e. concomitant diseases and their complications were poorly controlled and posed a potential threat to life in themselves. Consequently, taking into account multimorbidity, the majority of patients in both groups were classified into classes P3 and P4 (76.2%).To calculate the possible development of a fatal outcome, the severity of patients was assessed in accordance with the APACHE-II scoring system.The proportion of patients with a score of more than 20 in the main group was 49.5%, in the control group – 53.3% with a mortality probability of up to 30% according to the APACHE II scale. The proportion of patients with a score of 30 or more was 8.8% in the main group and 8.6% in the comparison group with a probability of death of 65%, which dictated the priority of minimally invasive interventions at the stages of treatment.The main group included 204 patients with acute cholecystitis, who, in order to improve treatment results, against the background of high surgical and anesthetic risk, underwent both minimally invasive radical laparoscopic surgeries, from a mini-access, and puncture-drainage interventions under ultrasound control.Minimally invasive puncture-drainage interventions under ultrasound control were performed in patients with acute cholecystitis with a high operational and anesthetic risk, in whom radical surgery in the scope of cholecystectomy was impossible due to the severity of their physical condition (P3, P4).These interventions were performed in 53 (25.9%) patients, of which 15 (7.3%) patients underwent percutaneous transhepatic puncture of the gallbladder (PTG) under ultrasound guidance, 38 (18.6%) - percutaneous transhepatic drainage of the gallbladder. bubble (BHJP). At the same time, gallbladder puncture was performed in patients in extremely serious condition.The effectiveness of PPV during the primary operation was 88.5%. The final efficacy, taking into account repeated punctures, was 96.1%. In this group of patients, one complication was observed in the form of perforation of the gallbladder wall, which required laparotomy, cholecystectomy, sanitation and drainage of the abdominal cavity.In this group, patients with ASA P4 indicator predominated, which corresponds to the presence of severe concomitant pathology with symptoms of decompensation of organs or body systems. The majority of patients (61%) had 3 or more concomitant diseases. At the same time, diseases of the cardiovascular, respiratory, central nervous and endocrine systems predominated. According to the Charlson comorbidity index, 86.5% had scores of 7 or more, which indicated a high transnosological comorbidity of patients.PPJP was performed in 38 patients (Fig. 6,7). | Figure 6. Simultaneous installation of drainage into the cavity of the gallbladder |
 | Figure 7. Echogram (moment of puncture of the gallbladder |
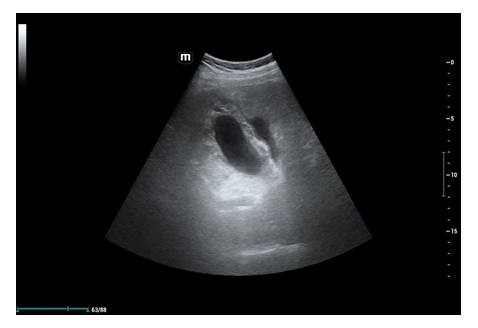
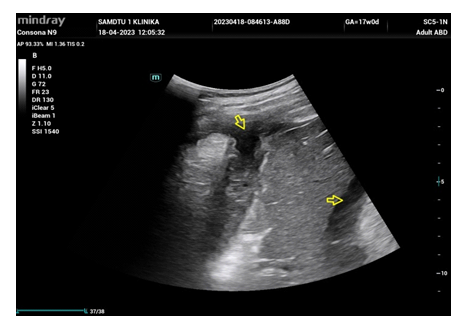
In 11 cases (28.9%) PPJP was performed as the only intervention, without resorting to radical surgery in patients with a high surgical risk.The effectiveness of PPCC was assessed by the degree of relief of inflammatory manifestations, both local and systemic, and changes in the gall bladder itself were also assessed. It should be noted that the relief of clinical symptoms (pain, nausea, vomiting and others) of acute cholecystitis occurred on average 2-3 days from the moment of drainage placement.By 3-5 days, a decrease in the severity of the systemic inflammatory response syndrome was noted, and by the time of discharge, which on average occurred on the 18th day, the laboratory laboratory results showed complete relief of inflammatory changes. If pronounced leukocytosis was noted upon admission (14.8±1.7x109/l), then on the 3rd day after the intervention it decreased to 11.6±1.9x109/l. By the fifth day after PPJP, normalization of leukocytosis in the blood was noted (9.5±1.2x109/l). In the postoperative period, 2 patients (5.3%) experienced complications such as bleeding along the drainage (spontaneous hemostasis), migration of drainage from the lumen of the gallbladder (no additional interventions were required), inflammatory changes in the soft tissues around the drainage tube. The most common complications were inflammatory changes in soft tissues in the drainage area.Complications that required urgent surgical intervention were present in 2 cases: in 1 case – parenchymal bleeding into the free abdominal cavity and in 1 – perforation of the gallbladder wall with bile leakage into the free abdominal cavity. There were no deaths among patients with PPJP.As planned, after PCI, relief of acute cholecystitis and correction of concomitant diseases, radical surgeries were performed in 27 patients using laparoscopy (16) and mini-access (11).Thus, puncture-drainage surgical interventions under ultrasound control were performed in patients with a high operational and anesthetic risk (P3 and P4), in the absence of signs of diffuse peritonitis; in 16 (30.2%) patients these procedures turned out to be definitive, and in 37 (69.8%) as the first stage before radical surgery.Endoscopic papillotomy was performed in 12 patients as EPST. Elderly patients predominated according to the ASA scale P3 and P4. EPST was performed in the presence of mechanical jaundice due to choledocholithiasis. This procedure was the second stage after PPJP (9), PPJP (3).The performance of laparoscopic cholecystectomy in this group of patients and the use of a mini-approach significantly expanded the treatment options for this category of patients. Radical minimally invasive surgeries were performed in 151 (74.0%) patients.Laparoscopic surgeries were performed in 105 (51.5%) patients, according to the ASA scale, they corresponded to (P2-P3). In patients with a high surgical and anesthetic risk (P3), performing LCE under conditions of tense carboxyperitoneum leads to serious consequences, such as myocardial infarction, pulmonary embolism, and respiratory failure. To level out these phenomena, in our study, LCE was performed at a minimum pressure of 6-8 mmHg. In this group of patients, the estimated risk of death was 10.5%. Despite this, we did not note any consequences of pneumoperitoneum during surgery.46 (22.5%) patients were operated on using the mini-laparotomy method. When performing minilaparotomy operations, we used a specialized biliary instrument set “Mini-Assistant”.137 patients (comparison group) were operated on using the wide laparotomy approach. Of these, 116 (84.6%) underwent cholecystectomy and 21 (15.3%) had cholecystostomy. Urgent operations were performed in 53 patients (38.7%). In 84 (61.3%) patients, delayed surgical interventions were performed 2-3 days after hospitalization due to the progression of intoxication and the appearance of symptoms of peritonitis. The degree of severity in this group of patients increased by an average of 6-8 points, while the surgical and anesthetic risk according to the ASA system did not decrease. In all patients operated traditionally, in the postoperative period there was an increase in severity on the first day by 12 points, followed by a decrease on days 2-3. In the postoperative period, various complications were observed in 19.7% of patients.Repeated interventions were performed in 11 cases (8.0%) and were associated with eventration (2), bile leakage (5), and the formation of purulent complications (2), with drainage of a subhepatic abscess in 1 case. 9 patients died (6.7%). The cause of death was thromboembolic complications, pneumonia, sepsis, and pancreonecrosis.Thus, in elderly and senile patients with high surgical and anesthetic risk, indications for laparotomy operations were forced and led to a significant number of postoperative complications (19.7%), as well as postoperative mortality (6.7%). The average bed day for traditional operations was 10.1±2.3. This was the reason for reviewing surgical tactics and the scope of surgical interventions for acute cholecystitis, in this category of patients, with an emphasis on minimally invasive high-tech operations.To compare the effectiveness of various methods of treating acute cholecystitis in elderly and senile patients with a high surgical and anesthetic risk, the following criteria were used: conversion, relaparotomy, duration of surgery (min), number of postoperative complications and deaths, length of patient stay in the hospital.When studying postoperative complications, one can note a significantly lower number of them in general after radical minimally invasive operations, both with puncture-drainage, endovideosurgical, and minilaparotomy (6.3% in total), compared with traditional ones (19.7%).The smallest number of postoperative complications (3.8%) is observed when performing puncture-drainage operations, despite the fact that these interventions were performed on patients with the highest degree of operational and anesthetic risk (P4).Table 2. The effectiveness of various methods of surgical treatment of acute cholecystitis (M ± m)
 |
| |
|
Taking into account the severity of patients with acute cholecystitis in accordance with the ASA scale, an algorithm for surgical treatment was developed. In the absence of peritonitis and when assessing the patient’s condition as P4, radical surgery, taking into account the severity of patients with acute cholecystitis in accordance with the ASA scale, determined the most optimal method of surgical treatment. In the absence of peritonitis and when the patient's condition is assessed as P4, radical surgery is accompanied by an extremely high risk. Accordingly, it is advisable to limit ourselves to performing decompressive percutaneous transhepatic intervention: PPJP, PPJP. If these patients have obstructive jaundice caused by choledocholithiasis, EPST is indicated after gallbladder decompression. This approach makes it possible to combine the positive aspects of both methods, stop the inflammatory process in the gallbladder and successfully resolve jaundice.
5. Conclusions
• Puncture-drainage interventions under ultrasound control in acute cholecystitis in patients with a high operational and anesthetic risk (P4), in 67.9% of cases, allow preparing patients for radical surgery (with a reduction in the risk class to P2, P3) using a minimally invasive laparoscopic method, and in 32.1% of cases they are the definitive treatment method.• The use of minimally invasive puncture-drainage, laparoscopic and endoscopic techniques, taking into account the surgical and anesthesiological risk according to ASA, APACHE II and the Charlson comorbidity index, makes it possible to timely perform the necessary treatment procedures, reduce the number of postoperative complications from 19.7% to 6.4%, postoperative mortality from 6.7% to 1.9%, as well as reduce the length of hospital treatment by an average of 5.5 bed days.
References
| [1] | Mini-invasive technologies in the treatment of acute cholecystitis with high surgical and anesthetic risk / A.S. Ermolov, A.A. Gulyaev, P.A. Ivanov [et al.] // Surgery. Zhurnalim. N.I. Pirogova. - 2014. - № 8. -С. 4-8. |
| [2] | Ultrasound and clinical and laboratory diagnosis of true morphologic forms of acute cholecystitis: the need to change the classification / I. M. Buriev, G. G. Melkonyan, N. S. Malyuga [et al.] // Annalykhsurgicheskogohepatologiya. - 2020. - Т. 25, № 3. - С. 55-62. |
| [3] | Hruppkin, V. I. Comparative analysis of ultrasound-guided decompression interventions in acute obturation cholecystitis in patients with high surgical and anesthetic risk / V. I. Hruppkin, A. N. Afanasyev, N. S. Glagolev // Bulletin of Novgorod State University. - 2015. - Т. 85, № 2. - С. 62-67. |
| [4] | Yaroslavtsev, M. I. Features of diagnostics of acute cholecystitis in different patients / M. I. Yaroslavtsev, M. A. Pakhomov, A. M. Morozov // Forcipe. - 2020. - Т. 3, № S. - С. 913-914. Acute cholecystitis: predictive clinico-radiological assessment for conversion of laparoscopic cholecystectomy / Y. R. Jiang, S. J. Ahn, S. J. Choi [et al.]. - DOI 10.1177/0284185120906658 // Acta Radiologica. - 2020. - Vol. 61, № 11. - P. 1452-1462. |
| [5] | Factors that Predict the Need for Subtotal Cholecystectomy / A. Tang, C. M. Cohan, J. Beattie [et al.]. - DOI 10.1177/0003134820979783 // The American Surgeon. - 2020. - Vol. 87, № 8. - P. 1245-1251. |
| [6] | Handra-Luca A. Luschka Ducts of the Gallbladder in Adults: Case Series Report and Review of the Medical Literature / A. Handra-Luca, H. M. Ben Romdhane, S.-M. Hong. - DOI 10.1177/1066896920901334 // International Journal of Surgical Pathology. - 2020. - Vol. 28, № 5. - P. 482-489. |
| [7] | Open Cholecystectomy Under Local Anesthesia for Acute Cholecystitis in the Elderly and High-Risk Surgical Patients / E. M. Slama, M. Hosseini, R. M. Staszak, V. R. Setya. - DOI 10.1177/00031348211050593 // Am Surg. - 2022. -Vol. 88 (3). - P. 434-438. |
| [8] | Open Cholecystectomy Under Local Anesthesia for Acute Cholecystitis in the Elderly and High-Risk Surgical Patients / E. M. Slama, M. Hosseini, R. M. Staszak, V. R. Setya. - DOI 10.1177/00031348211050593 // Am Surg. - 2022. -Vol. 88 (3). - P. 434-438. |
| [9] | Percutaneous cholecystostomy for grade III acute cholecystitis is associated with worse outcomes / Y. Sanaiha, Y.-Y. Juo, S. E Rudasill [et al.]. - DOI 10.1016/j.amjsurg.2019.11.025 // Am. J. Surg. - 2020. - Vol. 220 (1). - P. 197202. |
| [10] | Single port laparoscopic cholecystectomy: technical aspects and results / M. L. Favaro, S. Gabor, R. F. P. Pedroso [et al.]. - DOI 10.1590/0102-672020180001e1388 // Arq. Bras. Cir. Dig. (Säo P ulo). - 2018. - Vol. 31, № 3. - P. e1388. |
| [11] | Steel P. A D. Acute Cholecystitis and Biliary Colic / P. A D. Steel, B. E. Brenner // Medsckape: website. - URL: https: //emedicine. medscape.com/article/1950020-overview. |
| [12] | The Accuracy of Point-of-Care Ultrasound in the Diagnosis ofAcute Cholecystitis / C. J. Wehrle, A. Talukder, L. Tien [et al.]. -DOI 10.1177/0003134821989057 // The American Surgeon. - 2022. - Vol. 88, № 2. - P. 267-272. |
| [13] | Treatment of Acute Cholecystitis at Safety-Net Hospitals: Analysis of the National Inpatient Sample / S. Singh, S. J. Armenia, A. Merchant [et al.] // The American Surgeon. - 2020. - Vol. 86, № 1. - P. 28-34. |




 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML