-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 1012-1015
doi:10.5923/j.ajmms.20241404.43
Received: Mar. 21, 2024; Accepted: Apr. 12, 2024; Published: Apr. 18, 2024

Violations of the Functional Activity of the Sympathoadrenal System in the Development of Hypertension in Young People
Oybekova Gulasal Saidazimovna, Khuzhamberdiev Mamazoir Axmedovich, Vakhabov Bahramjon Muminjanovich
Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Arterial hypertension is one of the main risk factors that determines the prognosis of morbidity and mortality in the population. The problem of hypertension remains very relevant in many countries of the world. The results of our studies, to some extent, can show the important role of impaired SAS activity in the formation of hypertension in young people. It has been established that individuals engaged in IT activities experience a regular increase in the activity of the sympathoadrenal system due to constant exposure to the occupational factor, which is proved by an increase in the daily excretion of catecholamines and a decrease in MAO activity. Materials and methods. The study included 40 men aged 25 to 44 years, with a mean age of 33.4±5.6 years. Clinical, instrumental and special research methods were performed. It was revealed that in the population of young people engaged in active professional activities, there are violations of the functional activity of the sympathoadrenal system, manifested by an increase in the excretion of catecholamines, in particular epinephrine and norepinephrine, and a decrease in the content of the key enzyme of catecholamine deamination-monoaminе oxidase (MAO).
Keywords: Hypertension, Men, IT, Catecholamines, Epinephrine, Norepinephrine, Dopamine, Monoaminе oxidase
Cite this paper: Oybekova Gulasal Saidazimovna, Khuzhamberdiev Mamazoir Axmedovich, Vakhabov Bahramjon Muminjanovich, Violations of the Functional Activity of the Sympathoadrenal System in the Development of Hypertension in Young People, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 1012-1015. doi: 10.5923/j.ajmms.20241404.43.
Article Outline
1. Introduction
- The main cause of death in economically developed and rapidly developing countries is cardiovascular diseases (CVD). According to large studies conducted in different countries of the world, diseases of the cardiovascular system occupy a leading position in the structure of mortality and by 2020 have reached global significance. According to WHO research conducted in the Republic of Uzbekistan, it has shown that it belongs to the states with the highest development of cardiovascular diseases [1]. Recently, despite state programs for the prevention, treatment and prevention of cardiovascular diseases, the problem remains not fully solved (Khuzhamberdiev M. A. 2023, Kurbanov R. D. 2023, Fozylov Kh. G. 2023) [5].A special place in the problem of cardiovascular diseases is given to hypertension. According to WHO data from 2020, more than 30 % of the world's adult population suffers from hypertension and this is more than a billion people. Arterial hypertension is one of the main risk factors that determines the prognosis of morbidity and mortality in the population. The problem of hypertension remains very relevant in many countries of the world, including Uzbekistan. According to WHO experts, by the end of 2021, Uzbekistan is experiencing an increase in the number of cases in women by 9%, and in men even higher by 15%. Such a high prevalence of hypertension around the world, rightly allows us to consider it a "disease of civilization" [1]. Recently, there has been a tendency to increase the number of young people with hypertension. The widespread unfavorable lifestyle among young people in recent years has become not only a medical, but also a socio-economic problem of our time [1]. A large number of studies have been devoted to the pathogenesis, diagnosis, and treatment of hypertension in young adults (Lyamina S. V., 2010; Sundstorm J., 2012; Nechaeva G. I., 2013; Chernova I. M., 2014; Khuzhamberdiev M. A., Vakhabov B. M. 2023) [5,6,7,8]. At the same time, from the point of view of diagnosis, organization of the treatment of hypertension in young people is very important. Treatment and prevention of hypertension in this age group, many unresolved issues remain. According to the data of Feskova A. A., Pertsev A.V. from 2020, over the past 5-7 years, an increase in blood pressure is observed in 33-42% of adolescents, while 17-26% have persistent hypertension. Features that make it difficult to diagnose hypertension in the early stages in young people are the transient nature of increased blood pressure (BP) at the beginning of the disease and the conditionality of criteria for increased blood pressure (Kotovskaya Yu. V., Kobalava Zh. D., Kobzev R. Yu., 2012; Govorukhina A. A., Popova M. A., Vologzhanina N. A., 2015), as well as a peculiar clinical picture, in which vegetative disorders play an important role (Wein A.M., 2003; Conradi A. O., 2013), among the latter, great importance is attached to the increase in the tone of the sympathetic nervous system, which is considered to be the trigger moment for increasing blood pressure in young patients [2,3,4].Hypertension at a young age contributes to the increasing actualization of the problem, conducting research in this category of patients. In recent decades, it has consistently occupied one of the leading places in the structure of access, disability and mortality in cardiovascular diseases.Early diagnosis of arterial hypertension in young people will allow timely detection of the disease at the earliest stage of the process. The obtained data may serve as a basis for further development of preventive measures for the development of hypertension in young people.
2. Material and Research Methods
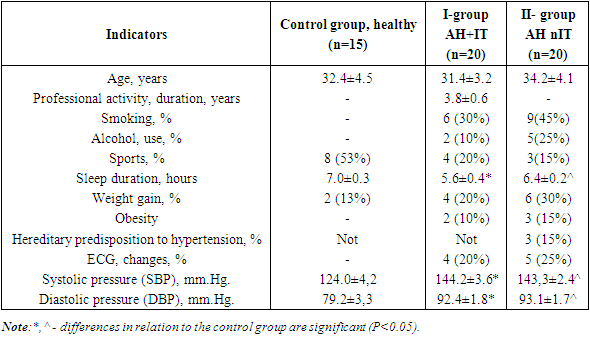
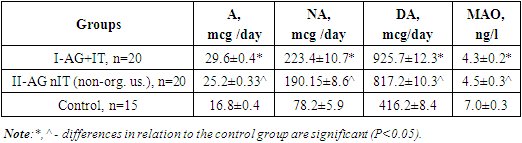
- The study included 40 male patients with arterial hypertension aged 25 to 44 years, with an average age of 32.8±3.6 years, and 15 relatively healthy male patients aged 20 to 44 years, with an average age of 32.4±4.5 years. Blood pressure (BP) was measured after 5 minutes of rest twice on both hands according to the accepted standard method at intervals of 5 minutes, in parallel, blood pressure was measured using automated electronic (oscillometric) devices, model Omron M6 ("Omron" Japan), according to the established protocol. The main blood pressure indicator included the average of two measurements, if there was a difference in blood pressure between the measurements of more than 5 mm. pt. st., then blood pressure was re-measured for the third time. Arterial hypertension was determined according to the WHO criteria adopted in 2023: systolic blood pressure (SBP) is greater than or equal to 140 mm.рHg, diastolic blood pressure (DBP) is equal to 90 mm Hg. The study was conducted after obtaining the participants informed consent, all the requirements of the Helsinki Declaration of the World Medical Association on Ethical Principles of conducting the study were observed. medical research from 2013. Depending on their professional activity, the study participants were divided into 2 groups: I-group I-20 men with hypertension who are engaged in IT at the age of 25 to 40 years, the average ageыof which was 31.4±3.2 years, II-group II-men who were diagnosed with hypertension as a result of preventive examinations at the place of residence those who do not have a certain type of professional activity, aged from 25 to 44 years, with an average age of 34.2±4.1 years, in the number of 20 people. The control group consisted of 15 relatively healthy male volunteers aged 20 to 44 years, whose average age was 32.4±4.5 years. Two days before the study, all participants were advised not to consume certain foods in their diet, such as strong tea and coffee, alcohol, cheese, and some fruits such as bananas and grapes. 96 hours before the study, exclude the use of antibiotics, beta-blockers, MAO inhibitors, exclude increased physical and neuropsychiatric overexertion.The daily urinary excretion of catecholamines (CA)-epinephrine (A), norepinephrine (HA), and dopamine (DA)-was determined by the fluorimetric method an Elisa bioliquid analyzer (Germany), and the ratio of norepinephrine to epinephrine-the norepinephrine-HA/epinephrine-A ratio was calculated using calculation methods.Determination of monoaminе oxidase (MAO), аkey catecholamine deamination enzyme, in blood serum was performed by Elisa (Germany).Static processing of the study results was performed pakets using Microsoft Excel 2010 SPSS Statistics 22.0 application software packages Statistics for Windows. Nonparametric methods of data analysis were used: Fischer and Mann-Whitney criteria to identify various indicators of the occurrence of deviations of the studied parameters from physiological norms. Changes in the probability of erroneous acceptance of the null hypothesis (p<0.05) were considered statistically significant.
3. Results and Discussions
- Comparative characteristics of age, social, behavioral, and instrumental indicators in the studied groups are presented in table 1.
|
|
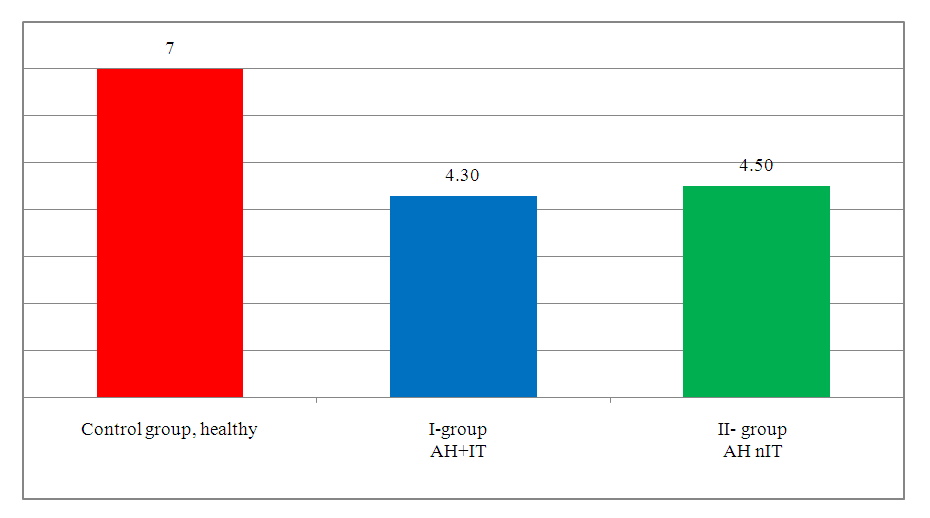 | Figure 1. Daily excretion MAO activity in relatively healthy and studied groups |
4. Сonclusions
- There were multidirectional changes in the daily excretion of catecholamines: epinephrine, norepinephrine and dopamine, depending on their professional activity; male individuals engaged in IT showed the maximum level of the hormonal and mediator components of the sympathoadrenal system. It has been established that individuals engaged in IT activities experience a regular increase in the activity of the sympathoadrenal system due to constant exposure to the occupational factor, which is proved by an increase in the daily excretion of catecholamines and a decrease in MAO activity. The results of the study can serve as a scientific basis for assessing and predicting the risk of cardiovascular diseases with the development of specific preventive measures to prevent violations of the functional state of the sympathoadrenal system in this category of subjects.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML