-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 951-954
doi:10.5923/j.ajmms.20241404.31
Received: Mar. 15, 2024; Accepted: Apr. 9, 2024; Published: Apr. 11, 2024

Chemokines are Predictors of the Transformation of Allergoses into Bronchial Asthma in Children
Matniyozova Zainab Tukhtaboevna, Emgurova Ozoda Razhabturdievna, Khodjaeva Nafisa Abayevna
Assistants, Department of 1-Рediatrics, Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article reflects the survey data aimed at studying the diagnostic significance of monocytic chemotactic protein-1 (MCP-1) in the development of allergies and the transformation of respiratory allergoses (RA) into bronchial asthma (BA), the severity of which may be a criterion for the degree of impairment, which must be taken into account when treating this category of children. A blood test was performed to determine MSR-1 in patients with respiratory allergies and healthy children who do not suffer from allergies. It was found that children have an increase in MSP-1 in bronchial asthma by 2.1 times than in respiratory allergies. The aim of the study was to study the diagnostic significance of MSR-1 in the development of allergies and the transformation of RA into BA in children. The object of the study was schoolchildren living in the conditions of the city of Bukhara. 80 children aged 7-14 years were under observation: boys - 61 (76,25,0±3,0%), girls - 19 (23,7,0±3,0%). After a thorough clinical and allergological examination, the following forms of respiratory allergies and healthy children were identified. Thus, 25 children did not have allergic symptoms, 30 suffered from respiratory allergies, and 25 were diagnosed with bronchial asthma. A blood test was performed to determine MSR-1 in patients selected for the study and in a group of healthy children who do not suffer from allergies at all. The study found an increase in MCP-1 in AD by 1.86 times relative to the control-352.96±78.0 pg/ml, p<0.05. A comparative analysis, depending on the form of allergy in children, also showed an increase in MCP-1 in BA by 2.1 times than in RA, p<0.05. When diagnosing and differentiating respiratory allergoses and bronchial asthma, the determination of the concentration of MCP-1 chemokines in the blood is an informative indicator that must be taken into account when treating this category of children.
Keywords: Chemokine, MSR-1, Respiratory allergoses, Cytokines, Bronchial asthma
Cite this paper: Matniyozova Zainab Tukhtaboevna, Emgurova Ozoda Razhabturdievna, Khodjaeva Nafisa Abayevna, Chemokines are Predictors of the Transformation of Allergoses into Bronchial Asthma in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 951-954. doi: 10.5923/j.ajmms.20241404.31.
Article Outline
1. Introduction
- In recent years, the discovery of chemokines and the study of their role in the pathogenesis of a wide range of diseases have determined the priorities of their research in various pathologies, including allergic diseases. In clinical practice, the study of chemokines makes it possible to assess the nature of the course of the process and predict the outcome of the disease in many allergoses, objectively evaluate the effectiveness of therapy, especially in cases of the use of drugs with immunomodulatory and immuno-correcting activity [1,2,3,5]. The steady growth of respiratory pathology in children and the high risk of the formation of respiratory allergoses determine the relevance of studying the factors and mechanisms of the formation of this pathology in childhood. An important role in the pathogenesis of respiratory allergoses in children is played by an imbalance in the level of cytokines-chemokines involved in the processes of allergic inflammation.Chemokines are substances capable of causing chemotaxis of immune cells into the damaged area. In particular, chemokines are isolated, capable of causing chemotaxis of monocytes. Such chemokines that activate monocyte chemotaxis include MCP-1. MCP-1 belongs to a large family of chemotactic cytokines that cause leukocyte migration into the inflammatory zone. MCP-1 is a protein with four cysteine residues (the first two are located adjacent and form an intermolecular compound in the form of disulfide bridges). Therefore, this protein is also called Chemokine (C–C motif) ligand 2, or CCL2. In humans, the MCP-1 gene is localized on chromosome 17. MCP-1 is involved in allergic inflammation mediated by mast cells and basophils, affecting leukotriene synthesis, histamine release and chemotaxis [2,4]. MCP-1, the most specific for monocytes, belongs to the class of chemokines. MCP-1 increases the chemotactic activity of monocytes and basophils, but it does not attract neutrophils and eosinophils to the inflammatory site. After removal of the N-terminal residue, MCP-1 ceases to act on basophils and becomes a chemoattractant for eosinophils. Basophils and mast cells that interact with CCL2 release their granules into the intercellular space. This effect can also be potentiated by prior exposure to interleukin-3 (IL-3) or other cytokines [2,5,7]. MCP-1 increases the antitumor activity of monocytes and is necessary for the formation of granulomas. CCL2 is found in places of teething and bone destruction. In the pathogenesis of bronchial asthma (BA), the leading factor is the interaction of various immunocompetent cells and inflammatory mediators, the participation of IL-17 in the regulation of neutrophil degranulation and the intensification of eosinophilic inflammation in the respiratory tract. Recent studies have noted the importance of an imbalance in the cytokine system and their producing cells, affecting the effectiveness of anti-inflammatory therapy of various BA phenotypes in children [1,6,7]. It was found that Th17 lymphocytes affect the formation of goblet cell hyperplasia, and IL-17 serves as the main factor enhancing mucin production and goblet cell hyperplasia in the bronchi of patients with asthma, which can affect local inflammation by inducing cytokine release.The aim of the study was to study the diagnostic significance of MCP -1 in the development of allergies and the transformation of respiratory allergosis into bronchial asthma in children.
2. Materials and Methods
- The study was conducted on the basis of the Bukhara regional Multidisciplinary Medical Center. The object of the study was schoolchildren living in the conditions of the city of Bukhara. 80 children aged 7-14 years were under observation: boys - 61 (76,25,0±3,0%), girls - 19 (23,7,0±3,0%). After a thorough clinical and allergological examination, the following forms of respiratory allergy were identified. The selected children were divided into 3 groups: the main 1st group consisted of 25 children with bronchial asthma, the second comparative group included 30 children with respiratory allergies (allergic rhinitis, sinusitis, allergic tracheitis, bronchitis). The control group 3 consisted of 25 healthy children who had no allergic manifestations. All children underwent immunological blood tests: chemokine MCP-1, interleukins IL-4, IL-17A, glutamyltranspeptidase (GGT). The specific diagnosis of allergic diseases was made on the basis of a comprehensive clinical, allergological, functional, laboratory examination and the formulation of specific allergic diagnostic tests (in vivo), taking into account International Consensus.
3. The Results and Their Discussion
- Monocytic chemoattractant protein-1 (MCP-1) is widely involved in normal physiological (angiogenesis) and pathophysiological processes in the body [4,6]. The source of MCP-1 synthesis is a wide range of cells: fibroblasts, monocytes and macrophages, endotheliocytes, leiomyocytes, cardiorabdomyocytes, cortical epithelial cells of the kidney, keratinocytes, epithelial cells of the HEP-2 line, intestinal epithelial cells, osteoblasts, liver adipocytes, chondrocytes, melanocytes, mesotheliocytes, stroma cells bone marrow, astrocytes [7,8]. And in connection with the above, we conducted a study to study the level of MCP-1 in children with respiratory allergies. In order to study the participation of MSR-1 in the development of allergies and the transformation of RA into BA, we performed a blood test to determine MSR-1 in patients selected for the study and in a group of healthy children who do not suffer from allergies at all. The results showed an average concentration of MCP-1 in the blood serum of healthy children, which is 352.96±78.0 u/l, while its minimum gradation was 191 u/l, the maximum gradation was within 510 u/l. (fig.1).
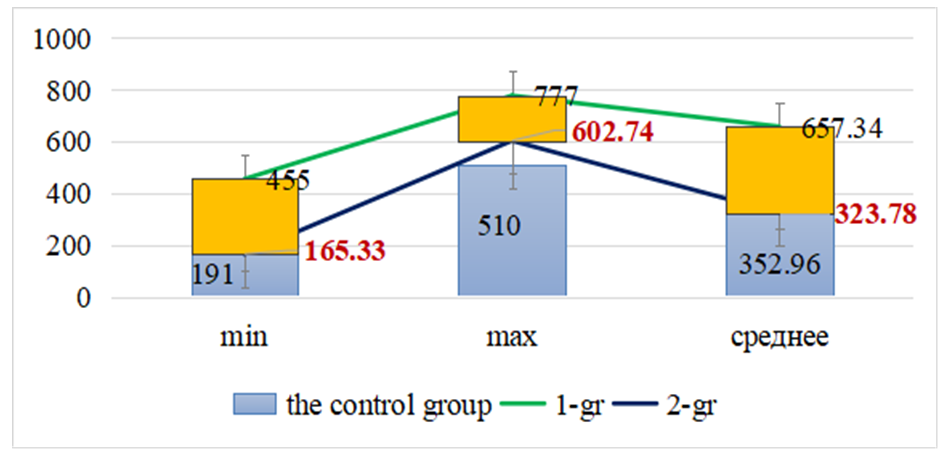 | Figure 1. Gradations of MSR-1 in respiratory allergies in children |
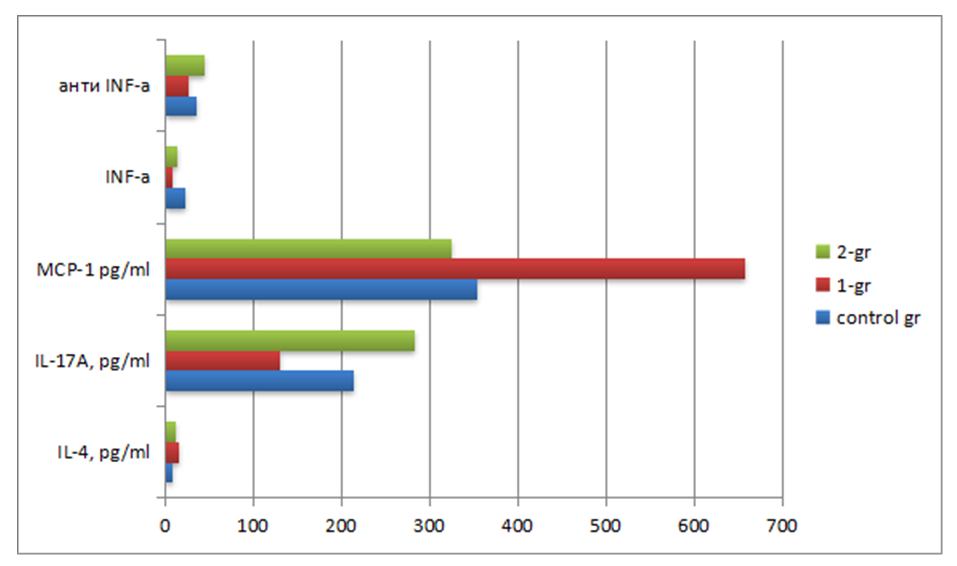 | Figure 2. Immunity indicators in children with respiratory allergies |
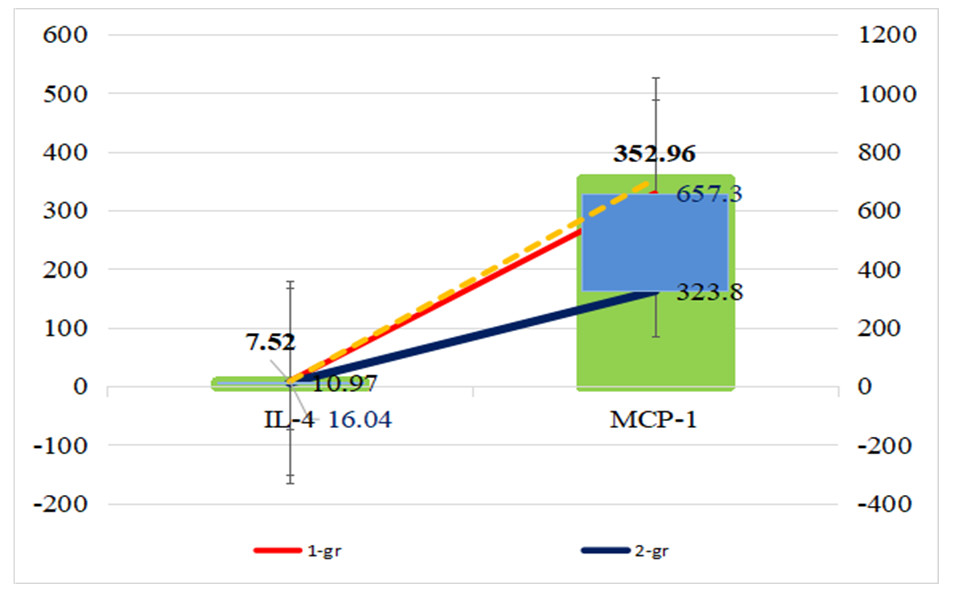 | Figure 3. Interleukin-4 and MCP-1 in respiratory allergies in children |
4. Conclusions
- The study of MSR-1 as an important element of the body's response to structural damage is relevant. The study of chemokines and interleukins in respiratory allergies in children allows for early diagnosis, differential diagnosis of respiratory allergies in children and prognosis of the transformation of respiratory allergies into bronchial asthma.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML