-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 926-933
doi:10.5923/j.ajmms.20241404.27
Received: Mar. 16, 2024; Accepted: Mar. 26, 2024; Published: Apr. 10, 2024

Radiological Differential Diagnosis of Pulmonary Edema: in Patients with Interstitial Pneumonia and Ischemic Heart Disease
Adkham Ilkhamovich Ikramov1, Nigora Mukhsumovna Djuraeva2, Otabek Vaxabovich Ablyazov3, Madina Mirgabtizyanovna Nizamova3, Khanum Valentinovna Abdukhalimova2, Lobar Nasirovna Tursunova1
1Center for the Development of Professional Qualifications of Medical Workers, SU “Republican Specialized Scientific and Practical Medical Center for Surgery named after Academician V. Vakhidova”, Tashkent, Uzbekistan
2SU “Republican Specialized Scientific and Practical Medical Center for Surgery named after Academician V. Vakhidova”, Tashkent, Uzbekistan
3Center for the Development of Professional Qualifications of Medical Workers, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Pulmonary edema, a critical complication in emergency medical scenarios, often leads to terminal states and fatalities. This study investigates specific X-ray and computed tomography (CT) signs for the differential diagnosis of hemodynamic and membranogenic pulmonary edema in emergency patients with diverse pathologies. Methods: Clinical and radiological data from 30 patients with acute pulmonary edema were analyzed. Two groups were formed based on the type of pulmonary edema: interstitial pneumonia-related membranogenic edema (Group 1) and coronary heart disease-related cardiogenic edema (Group 2). X-ray and CT scans were performed and compared with the clinical progression. Results: Group 1, predominantly with membranogenic edema, exhibited interstitial pulmonary edema on X-ray (80%), progressing to alveolar edema. CT scans revealed asymmetrical ground glass appearance, often with zones of consolidation. Group 2, with cardiogenic edema, presented enhanced interstitial patterns, evolving into alveolar edema with central distribution on CT. Effusions and heart chamber dilation were noted in Group 2. Conclusion: Comprehensive and timely diagnosis plays a crucial role in unraveling the pathophysiological intricacies of pulmonary edema. CT emerges as a highly effective tool, achieving a notable 96–98% accuracy in differentiating between cardiogenic and non-cardiogenic edema. The significance of detailed imaging is underscored by the distinct radiographic patterns observed in each group. Specifically, CT illuminates unique features of alveolar pulmonary edema, enhancing its role in the differential diagnosis. Moreover, the correlation between CT findings and clinical dynamics, along with specific nosologies, provides valuable insights into the nature and severity of pulmonary edema.
Keywords: Pulmonary edema, Computed tomography (ct), Cardiogenic, Non-cardiogenic, Alveolar edema
Cite this paper: Adkham Ilkhamovich Ikramov, Nigora Mukhsumovna Djuraeva, Otabek Vaxabovich Ablyazov, Madina Mirgabtizyanovna Nizamova, Khanum Valentinovna Abdukhalimova, Lobar Nasirovna Tursunova, Radiological Differential Diagnosis of Pulmonary Edema: in Patients with Interstitial Pneumonia and Ischemic Heart Disease, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 926-933. doi: 10.5923/j.ajmms.20241404.27.
1. Introduction
- Relevance of the Problem: Pulmonary edema is a common complication of several urgent medical conditions in the emergency medical system and often leads to the development of a terminal state and the death of the patient. The pathogenesis of pulmonary edema is well-known at present. Balanced fluid exchange through the microvessel walls in the lungs is the foundation for adequate gas exchange and protects against edema. Pulmonary edema is a complex process involving disruptions in the body's fluid-electrolyte and colloid-osmotic balances. Depending on the primary cause, four types of pulmonary edema can be distinguished: hemodynamic (cardiogenic), membrane-related (non-cardiogenic), central, and mixed [1,6].Hemodynamic (cardiogenic) pulmonary edema, as a rule, is a consequence of left ventricular failure in hypertension, heart defects, myocardial infarction, due to impaired hemodynamics of the pulmonary circulation (pulmonary congestion and increased pulmonary capillary pressure) [3]. The main cause of the development of cardiogenic pulmonary edema is acute left ventricular failure associated with a decrease in myocardial contractility [6].Membranogenic (non-cardiogenic) edema implies deep disturbances in the permeability of pulmonary capillaries with the release of fluid with a high protein content, including fibrin, into the lumen of the alveoli. The classic manifestation of this type of edema is acute respiratory distress syndrome (ARDS). Acute respiratory distress syndrome (ARDS) is a clinical syndrome characterized by non-cardiogenic edema of the lung tissue with severe impairment of gas exchange and respiratory mechanics, ventilation/perfusion ratio in the lungs [5]. The development of ARDS can be caused by both “direct” damaging factors - aspiration of aggressive substances, trauma, inhalation of irritating gases, and “indirect” factors, which include inflammatory mediators that have a damaging effect on the endothelium of the microcirculatory bed [4,5]. Reactions occurring in lung tissue during ARDS are always universal and nonspecific [6,7]. Today it is becoming clear that ARDS is a non-homogeneous, polyetiological disease, has complex, not fully understood mechanisms of pathogenesis and requires differentiated and individual treatment in each specific clinical situation [2].In many manuals, articles, reviews, the X-ray picture is called one of the leading criteria for diagnosing severe pneumonia, viral-bacterial pneumonia, viral pneumonia, ARDS, but the wording in the section “Changes in the lungs” is very sparse - “bilateral infiltrates”, “diffuse damage”, “extensive areas of consolidation,” which requires consideration of more detailed X-ray and CT semiotics of ARDS [4].The differential diagnosis between cardiogenic and non-cardiogenic pulmonary edema is difficult - both conditions have largely similar clinical and radiological manifestations [6,8].The purpose of the study was to identify specific X-ray and computed tomography (CT) signs that allow for differential diagnosis of hemodynamic and membranogenic pulmonary edema upon admission of emergency patients to a multidisciplinary hospital with various pathologies.
2. Patients and Methods
- Patient Selection and DemographicsAn extensive analysis of clinical and radiological data was carried out in 30 patients (18 men and 12 women) from the therapeutic and cardiology departments with acute pulmonary edema syndrome. The average age of patients was 47.3±18.4 years.Group Division and CharacteristicsThe patients were divided into two conditional groups depending on the type of pulmonary edema. The first group included 15 patients (10 men and 5 women) who were treated for interstitial pneumonia, severe forms of pancreatic necrosis, and massive blood loss with the development of membranogenic pulmonary edema. The second group comprised 15 patients (8 men and 7 women) with various manifestations of coronary heart disease (CHD), including acute and recurrent myocardial infarction with the development of the classic picture of cardiogenic pulmonary edema.Imaging Techniques and Comparative AnalysisX-ray examination was carried out using digital X-ray apparatus: Apelem "Platinum 2" (France), "MobiRen-MTU" (Uzbekistan). Multislice computed tomography (MSCT) of the chest organs was performed using Aquilion Prime 160 MSCT device (Canon Medical System) and MSCT 640 "Aquilion one" Genesis version (Canon). Radiological studies were compared with the clinical picture at various stages of the disease.
3. Results
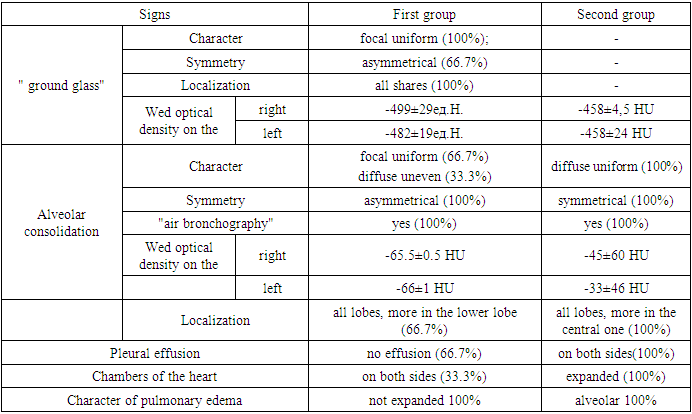
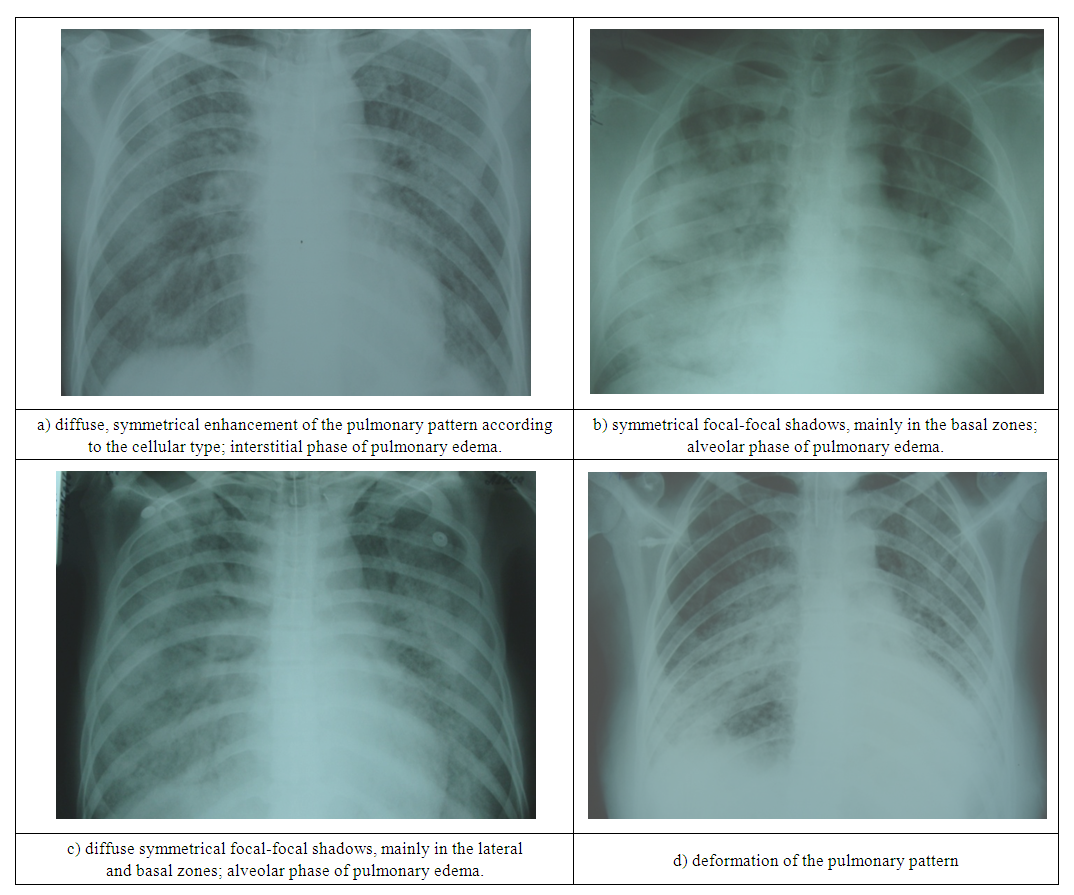
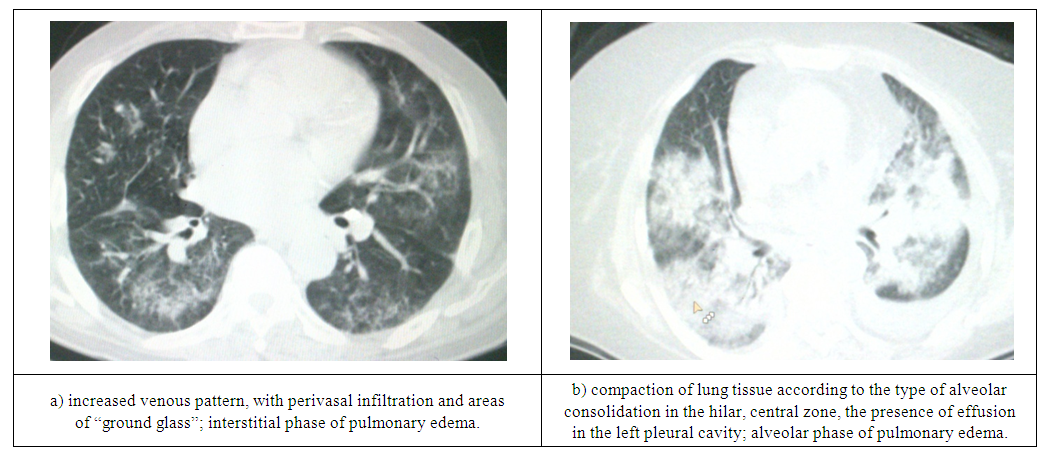
- The first group of the study included 15 people, of whom 9 were men and 6 women. The average age of the patients was 39.4±16.6 years. Death was recorded in 11 patients (73.3%).According to the data obtained, in the clinical picture of patients of the first group, already upon admission to the hospital, all symptoms were dominated by signs of respiratory failure, which was manifested by increased heart rate, shortness of breath, cyanosis, and a compensatory increase in blood pressure.In parallel with the development of the clinical picture, the patients underwent X-ray examination and computed tomography. In 3 patients (20%) in the first or third day from the onset of respiratory failure, the X-ray picture was practically not manifested in anything; in 12 patients (80%) in the phase of interstitial pulmonary edema, a diffuse increase in the pulmonary pattern was noted, predominantly of a fine-mesh type, root pattern was characterized by little structure, the sinuses were free, the borders of the heart were not expanded (Fig. 1a). Taking into account the radiological studies performed, in 3 patients (20%) with ARDS, no pathological changes were noted on the radiographs, but the clinical picture was consistent with this pathology. This was the indication for CT scanning. In all patients in this group, the “ground glass” was asymmetrical, diffuse, spreading throughout all lobes of both lungs. (Table 1), more pronounced in the peripheral zone and posterior segments. When performing densitometric analysis of lung tissue, in areas of “ground glass”, an increase in density was noted on the right to -499±29 units N., on the left to -482±19 units N. The effusion in the pleural cavity was not detected, the heart chambers in almost all patients were not dilated (Fig. 2a).
|
|
 | Figure 1. Chest radiographs of membranogenic pulmonary edema |
 | Figure 2. Computed tomograms of the chest organs for membranogenic pulmonary edema |
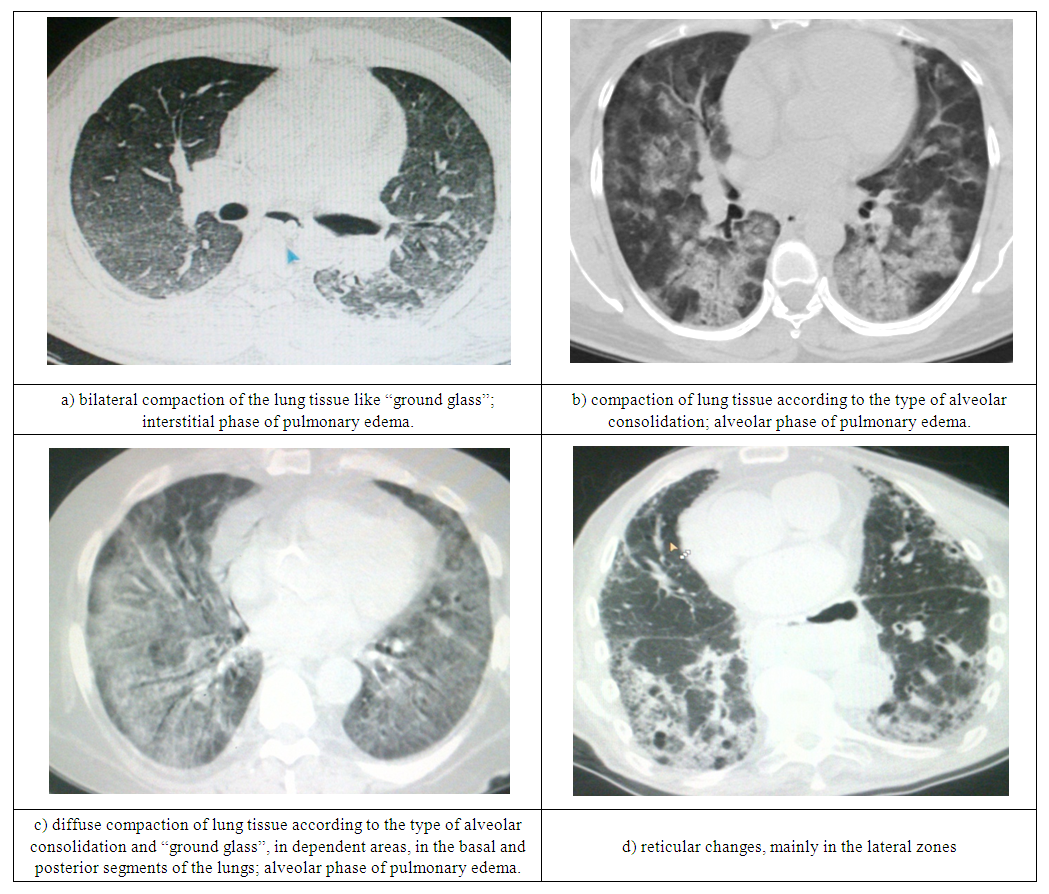
 | Figure 3. X-rays of the chest organs with hemodynamic pulmonary edema |
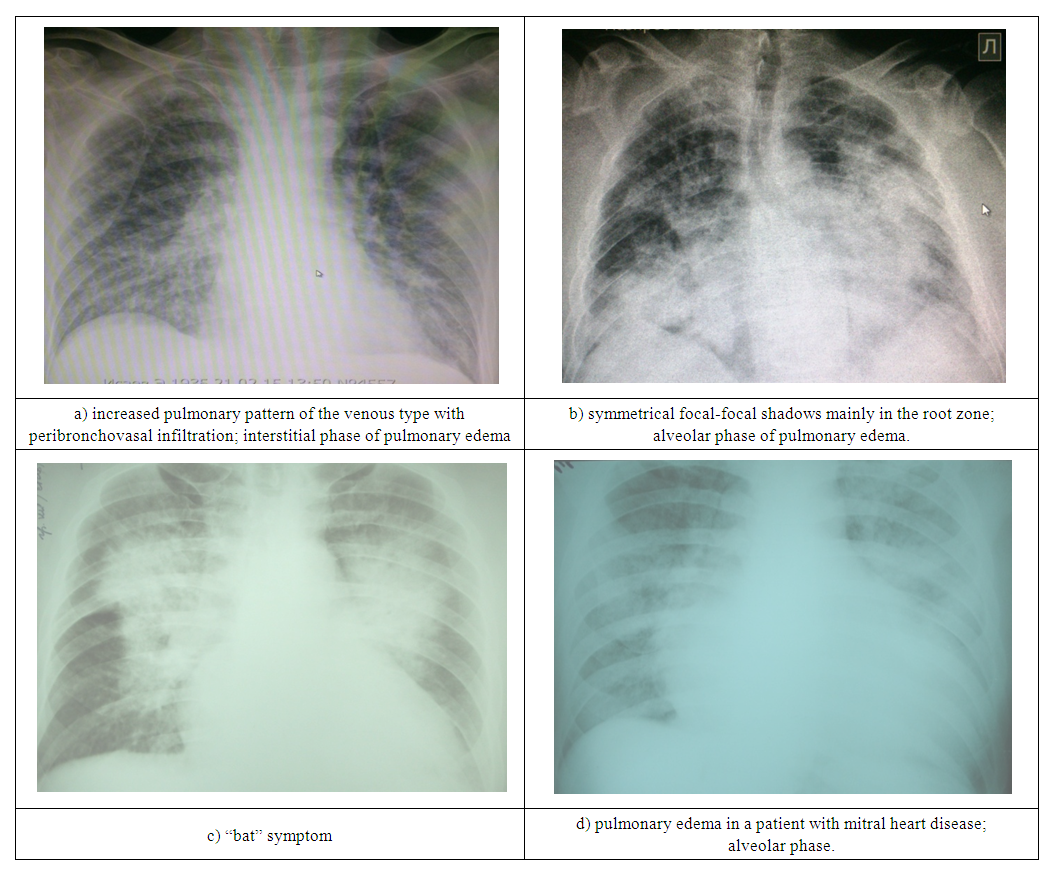
 | Figure 4. CT of the chest organs for hemodynamic pulmonary edema |
4. Conclusions
- 1. Comprehensive diagnosis of pulmonary edema in the early stages of development allows us to identify the main stages of the pathological process, assess its dynamics and, in most cases, clarify the pathophysiological mechanism of the occurrence of edema.2. Computed tomography makes it possible to timely diagnose pulmonary edema and establish its nature in case of cardiogenic edema in 96%, and in case of respiratory distress syndrome – in 98% of cases.3. The general x-ray picture of the first group of patients was characterized by interstitial pulmonary edema (80%) and in 20% of cases no changes were noted on the x-ray. In patients of the second group, interstitial edema was observed in 80% of cases, and venous congestion was noted in 20% of cases. The alveolar stage of pulmonary edema in patients of the first and both groups was diagnosed in 80% of cases.4. In patients of both groups, on CT in the interstitial phase, the “ground glass” appearance of pulmonary edema was symmetrical, uniform, diffuse, spreading throughout all lobes of both lungs. Moreover, in patients of the first group the process was 100% asymmetrical, and in patients of the second group it was symmetrical in 100% of cases. Against the background of ground glass in patients of the first group, zones of consolidation were determined in 33% of cases. No consolidation zones were observed in patients of the second group. The pulmonary pattern was changed in 100% of cases in patients of the second group, while in patients of the first group the pulmonary pattern was not changed. Effusion in the pleural cavity and pericardial cavity was not detected in patients of the first group, but in patients of the second group there was effusion in 66.7% of cases. Dilation of the heart chambers was recorded in all patients of the second group; in patients of the first group, the heart chambers were not dilated.5. During the phase of alveolar pulmonary edema, patients with ARDS and cardiogenic pulmonary edema were characterized by alveolar compaction; this sign was recorded in 100% of cases. According to the prevalence of the process for patients with ARDS, it is typical to spread throughout all lobes of both lungs, but more in the lower lobe (66.7%) due to the gravitational gradient. And for patients with cardiogenic edema, it is typical to spread throughout all lobes of both lungs, but more centrally (100%). The average optical density of the alveolar compaction in patients of the first group on the right was -65.5±0.5 units N., which is 19.5 units N. more than in patients of the second group, and on the left this indicator was -66±1 units N., which is 33 units N. more than in patients of the second group.6. The dependence of the obtained CT data on the dynamics of the clinical picture and the specific nosology that determined the development of the pathological process was revealed. Patients of the first group, as a rule, were admitted with an acute, new-onset pathology (interstitial pneumonia); the dynamics of the clinical picture depended on the severity of the disease and the rate of development of pathological processes in the body. Patients of the second group had a history of coronary heart disease, with a long course, changes in hemodynamics, restructuring of the heart muscle, and congestion in the pulmonary circulation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML