-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 911-916
doi:10.5923/j.ajmms.20241404.24
Received: Mar. 14, 2024; Accepted: Mar. 28, 2024; Published: Apr. 10, 2024

Evaluation of the Effectiveness of PRP Therapy in Repair Processes Suture on the Uterus after Cesarean Section
J. M. Gafurov1, D. D. Saidjalilova2, B. B. Kurbanov3
1Republic Perinatal Center, Tashkent, Uzbekistan
2Tashkent Medical Academy, Uzbekistan
3Tashkent Pediatric Medical Institute, Uzbekistan
Correspondence to: J. M. Gafurov, Republic Perinatal Center, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Purpose of the study: to evaluate the effect of platelet auto-plasma administered intra operatively on the processes of reparative regeneration and the formation of a full-fledged scar on the uterus after cesarean section. We studied 116 pregnant women in the period 2022-2023, who were delivered by cesarean section. We can conclude that using of platelet auto-plasma promotes the formation of a full-fledged scar on the uterus after cesarean section.
Keywords: Cesarian section, Pregnancy, Autoplasma
Cite this paper: J. M. Gafurov, D. D. Saidjalilova, B. B. Kurbanov, Evaluation of the Effectiveness of PRP Therapy in Repair Processes Suture on the Uterus after Cesarean Section, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 911-916. doi: 10.5923/j.ajmms.20241404.24.
Article Outline
1. Background
- According to WHO, over the past thirty years, the proportion of caesarean sections (CS) has increased worldwide, reaching its highest level in the current decade, and has approached 25-30%, reaching 40-50% in large perinatal centers [1-6]. In the general population of women of reproductive age, 15-42% has a history of CS [7-9]. The CS operation, despite its technical simplicity, is a surgical procedure that has a considerable number of intra- and postoperative complications. [10-15]. The postpartum period, even with a physiological course, is favorable for the development of infectious complications; with surgical delivery, it is “superimposed” by the postoperative period and associated additional significant risk factors (blood loss, edema, ischemia, tissue destruction in the suture area, the presence of microhematomas, foreign suture material) [16,7]. Abdominal delivery causes up to 89.6% of all endometritis [17-19]. Assessment of reparative processes after CS in the body as a whole, restoration of the operated uterus and analysis of the outcomes of these processes are of great importance, including in understanding the formation of an incompetent suture/scar on the uterus after [18,20].Along with the increase in the frequency of abdominal births and their complications, the question of the possibility of delivery of women with a uterine scar through the natural birth canal is becoming increasingly urgent, but this requires the presence of a full-fledged uterine scar [16,3,21]. The main conditions for optimal tissue regeneration and the formation of a complete scar are good blood circulation in the wound, excluding the development of ischemia and tissue hypoxia in the suture area, and a minimal inflammatory reaction, which is determined by the method of restoration of the dissected uterine wall and the type of suture material [6,22,15,18]. There are very few data in the literature on methods of influencing the reparation activity and the formation of a full-fledged scar [3,23]. Studies of the process of wound repair on the uterus have made it possible to expand the existing understanding of the course of the wound process and continue the search for technologies to activate full tissue repair [6,25]. For this purpose, such techniques as argon plasma coagulation of tissues [18], collagen membrane implantation [11], and modern cellular technologies [20] are used.PRP therapy (plasma therapy) is the use of your own blood plasma, which is enriched with platelets (PRP - Platelet Rich Plasma). Autologous platelet-rich plasma (APRP/PRP) was first used for hemostasis during surgery and platelet transfusion in certain thrombocytopenic conditions [3]. In 1985, David Knighton first used platelet-rich plasma to treat chronic trophic ulcers [3]. As it turned out, APRP is safer than cell-based regenerative therapy. Since 1998, independently of each other, several American research groups began to conduct research on APRP to accelerate wound healing and tissue restoration in maxillofacial surgery. APRP/PRP is often used in various fields of medicine and has expanded from stimulating bone regeneration, healing wounds and ulcers, and musculoskeletal injuries to increasing the ability to engraft various types of transplants in dentistry. Due to the natural properties of platelet-enriched plasma, its introduction into the human body is one of the promising procedures in tissue repair. APRP contains α-granules, from which, after activation, many factors are released, such as transforming growth factor - beta (TGF-β), vascular endothelial growth factor (VEGF) and epidermal growth factor (EGF), as well as adhesive molecules and cytokines that stimulate reparative and anabolic processes in damaged tissues, as well as having an anti-inflammatory effect [17]. Considering the universal mechanism of action of platelet auto-plasma, it is used in various branches of medicine: dentistry, ophthalmology, traumatology, combustiology, sports medicine, and cosmetology. However, the effect of platelet autoplasma on the regeneration of damaged uterine tissue during CS surgery and the formation of a uterine scar has not currently been studied.
2. Purpose of the Study
- To evaluate the effect of platelet auto-plasma administered intra-operatively on the processes of reparative regeneration and the formation of a full-fledged scar on the uterus after cesarean section.
3. Material and Methods of Research
- 116 women were examined in the period 2022-2023, who were delivered by cesarean section at the Republican Perinatal Center. Depending on the management, the patients were divided into groups: the main group consisted of 45 women who were injected with platelet auto-plasma during a cesarean section after suturing the incision on the uterus; the comparison group consisted of 71 women who did not receive platelet auto-plasma during surgery. Prior to the study, the voluntary informed consent of the patients was obtained. The criteria for inclusion in the study were: delivery by CS, longitudinal position of the fetus, dilation of the uterine cervix no more than 5 cm in case of emergency surgery. Exclusion criteria were: history of uterine surgery (caesarean section, myomectomy), uterine fibroids with a diameter of more than 5 cm, localized in the body of the uterus or in the isthmus, severe preeclampsia, inflammatory diseases of the female genital organs, acute infections of extra-genital localization, multiple pregnancy, premature birth. The examination of pregnant women, involved in the study was carried out in accordance with the National Standard for Management of Pregnancy and Childbirth. A comparative analysis of the course of previous and current pregnancies, childbirth and the postpartum period, as well as laboratory, instrumental and functional research methods was carried out. The direct method of using platelet auto-plasma (PAP) was as follows. To obtain PAP before surgery, 15 ml of venous blood was taken into special tubes, followed by centrifugation for five minutes at a speed of 1500 rpm. The volume of platelet-rich plasma obtained was about 12 ml. Statistical processing of the results was carried out with the determination of quantitative characteristics of the arithmetic mean (M), error of the arithmetic mean (m), and standard deviation. To assess the reliability of differences in the distribution of qualitative values, the criterion of agreement χ² (chi-square) and the magnitude of confidence intervals (p) were calculated.
4. Research Results
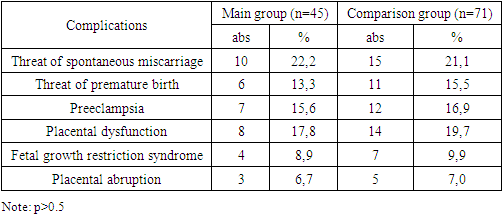
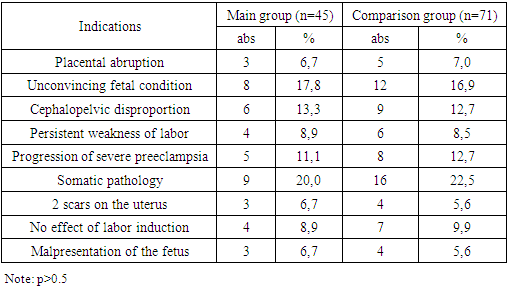
- The average age of the patients who took part in the study was 25.6+5.4 years in the main group, and 26.1+5.1 years in the control comparison group (p>0.05). According to the presented results, the majority of patients were aged 21-30 years and there was no significant difference between the groups in the age of the patients (p>0.05). A study of the somatic history showed that in both groups, iron deficiency anemia was most often detected (in 20% of patients in the main group and in 15.5% in the comparison group). To a lesser extent, diseases of the gastrointestinal tract (chronic gastritis, cholecystitis in remission), diseases of the genitourinary system (chronic pyelonephritis in remission) are noted. Varicose veins were observed in 13.3% and 9.9%, respectively. Among the diseases of the nervous system, epilepsy was encountered, which was an indication for CS. Another indication was high myopia or eye surgery. A study of the anamnesis revealed that 5 patients (11.1%) of the main group and 6 women (8.5%) of the comparison group had surgical interventions on the abdominal organs for appendicitis, ectopic pregnancy, ovarian apoplexy and ovarian tumor formations. When analyzing gynecological diseases in the groups, a history of vaginitis and bacterial vaginosis, cervical pathology, and menstrual cycle disorders were more common. Cervical pathology included ectropion (3 patients in each group) and cervical polyp (2 patients in the main group and 1 in the control group), for which surgical treatment - removal of the polyp and diathermoconization was performed. Equally often in both groups (11.1% and 7.04%, respectively), patients had a history of suffering from inflammatory diseases of the pelvic organs. In total, 26.7% of patients in the main group and 22.5% in the control group had a history of gynecological diseases.The study of obstetric history showed that in both study groups primiparas predominated: in the main group they accounted for 93.3% (42 patients), in the control group – 91.6% (65 patients). The remaining women were multiparous. In addition, the women studied had a history of spontaneous miscarriages in 3 (6.7%) women in the main group and 7 (9.9%) women in the comparison group.A study of the course of this pregnancy (Table 1) showed that gestation was often complicated by the threat of miscarriage, which was equally common in the study groups (22.2% and 21.1%, respectively). Preeclampsia was observed more rarely in 15.6% and 16.9% of women, respectively. Placental insufficiency was noted in 17.8% of women in the main group and in 19.7% in the comparison group. Fetal growth restriction syndrome was detected in 4 (8.9%) and 7 (9.9%) women in the study groups, respectively. Such a serious complication of pregnancy as placental abruption occurred in 3 (6.7%) women in the main group and in 5 (7.0%) women in the comparison group, which was one of the indications for cesarean section (Table 2).
|
|
|
|
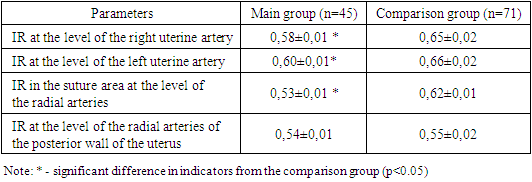
5. Conclusions
- 1. The introduction of platelet autoplasma into the suture area of the uterus has a positive effect on the healing of the uterine scar and makes it possible to accelerate the process of reparative regeneration.2. The use of platelet autoplasma promotes the formation of a full-fledged scar on the uterus after cesarean section by increasing angiogenesis, improving vascularization of the uterus and the scar area.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML