-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 894-896
doi:10.5923/j.ajmms.20241404.19
Received: Feb. 25, 2024; Accepted: Mar. 23, 2024; Published: Apr. 3, 2024

Analysis of Inflammatory Markers in Patients with Ulcerative Colitis
Аbdullayeva U. K.1, Karimov M. M.2, Sobirova G. N.3
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Republican Specialized Scientific and Practical Center for Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
3Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study included 128 patients treated ulcerative colitis in the Gastroenterology Department of Bukhara regional Multidisciplinary Medical Center during 2021-2023 and 20 health professionals as a control group. Patients were diagnosed with serum immunoferment analysis using TNF-α, IL-6, IL-17A, TGF-β2 and its importance was studied. The results of the study showed an increase in TNF-α, IL-6, IL-17A and a decrease in TGF-β2 in severe types of ulcerative colitis, and found that it could be used in diagnosis as a poor prognostic marker.
Keywords: Ulcerative colitis, TGF-β2, IL-6, IL-17A, TGF-β2
Cite this paper: Аbdullayeva U. K., Karimov M. M., Sobirova G. N., Analysis of Inflammatory Markers in Patients with Ulcerative Colitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 894-896. doi: 10.5923/j.ajmms.20241404.19.
1. Introduction
- Ulcerative colitis is a chronic cause of unclear inflammation of the large intestine, a continuous superficial inflammation of the mucous membrane, as well as a disease that spreads to varying degrees from the rectum to the upper parts of the large intestine. Ulcerative colitis has the property of relapsing and remitting. Distinguishing signs of ulcerative colitis include a call to urinate and a bloody diarrhea that comes in conjunction with a call to the exit of the litter [1]. Despite the fact that the etiology of ulcerative colitis remains under debate, many data have proven that an autoimmune process lies on the basis. Most patients have common similarities with a number of autoimmune disorders such as involvement of limb damage in the process, with extra-intestinal symptoms of ulcerative colitis observed [2].A distinctive feature of the epidemiology of ulcerative colitis is the spread of this disease among young people of working age in recent years. European studies have described the impact of ulcerative colitis on the quality and level of life of patients, their work training, their relationship with those around them [3]. More than 25% of patients around the world have problems with frequent toilet access or the need for a garbage collector in their work. Late diagnosis of the disease, severe and severe forms of the disease indicate its high lethality [4].Like other inflammatory bowel diseases, there is still no clear cause of ulcerative colitis. The disease is formed as a result of the concomitant arrival of several factors, including a hereditary predisposition, congenital and acquired diseases of the immune system, violation of the intestinal normative microflora and harmful environmental influences. Those of greater importance in them received inflammation TNF-α, IL-6 and anti-inflammatory IL-4 and TGF-β2. TNF-α stimulates the production of IL-6, so that the function of IL-6 is compatible with its activator [5]. Of the anti-inflammatory interleukins, TGF-β2 is a multifunctional anti-inflammatory cytokinin involved in metabolic reactions, apoptosis and migration, stratification processes in target-cells. Every cell in the body, including epithelial, endothelial, nerve and connective tissue cells, produces TGFß. In ulcerative colitis, the synthesis of TGFß2, which denotes regeneration, is reduced as a result of impaired cellular integrity [6]. Assessment of the severity of ulcerative colitis is important for management of treatment and predicting the consequences of the disease. Literature analysis has shown that interleukins analysis in patients with ulcerative colitis has been carried out in large numbers, but given that they can all increase in other diseases, there is a need to develop a special diagnostic method that assesses the severity of the disease [7].
2. Material and Methods
- The study was carried out in the Department of Gastroenterology of the Bukhara regional Multidisciplinary Medical Center in 2021-2023. The study included 128 patients diagnosed with yak in accordance with the criteria for inclusion, treated in stationary and outpatient conditions, and 30 healthy individuals as a control group.Initially, anamnestic data was collected in all patients.The condition of the colon mucosa in Yak was carried out in the ENDOMED medical and Diagnostic Clinic using Fujifilm 4450hd videoprocessor, Fujinon ec-530fl videocolonoscope (Japan).Yak Lamb severity was determined by the endoscopic activity level (Schroeder) of the disease in accordance with Yak's Meyo activity level.The study applied mesons developed by the Russian society of gastroenterologists and coloproctologists based on the recommendations of the joint European consensus with Truelove-Witts mesons to assess the severity of lambs in the disease classification.All cytokines were conducted with immunoferment analysis in the autormat analyzer MINDRAY MR-96A (China).The study analyzed interleukins in terms of disease activity levels, severity levels, clinical variants, and duration of the disease.
3. Results
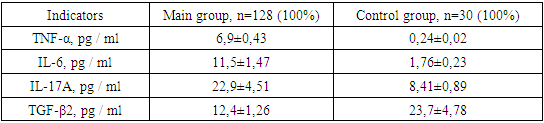
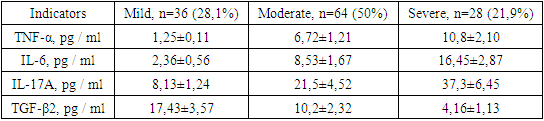
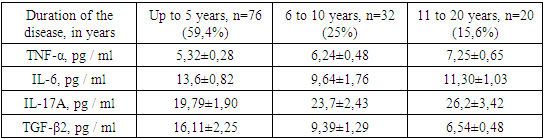
- Patients with ulcerative colitis were diagnosed with serum inflammation-calling TNF-α, IL-6, IL-17A, Calprotectin, and anti-inflammatory TGF-β2. Based on the results of serum-detectable inflammatory marker analysis, it was observed that primary group patients showed nearly 30 increases in TNF-α compared to individuals in the control group, with IL-6 6.5 times, IL-17A 2.7 times, and TGF-β2 almost 2 times (Table 1).
|
|
|
|
|
4. Conclusions
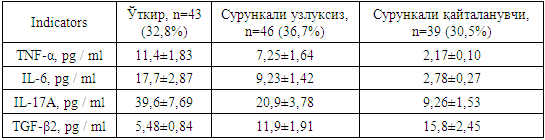
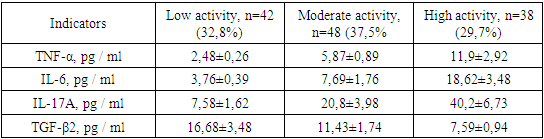
- Hence, ulcerative colitis has been observed to have decreased levels of inflammation-calling markers (serum-detectable TNF-α, IL-6, IL-17A, anti-inflammatory cytokine (TGF-β2) primarily responsible for regeneration, as weight levels, activity levels increase. Such a result is an increase in markers that call inflammation in the acute type of disease, a decrease in anti-inflammatory markers, and in chronic continuous and chronic relapsing types, the opposite result is observed. The results obtained make it possible to use TNF-α, IL-6, IL-17A, TGF-β2 as always available, non-traumatic methods for determining the level of cytokine and assessing the severity of the inflammatory-destructive process in patients with ulcerative colitis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML