Shokirova Sadokathon Muhammatsolievna
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Shokirova Sadokathon Muhammatsolievna, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
In this study, women with non-endocrine factors of infertility (tube - peritoneal and endometriosis) without tumor-like formations or functional ovarian cysts, with PCOS (Polycystic Ovarian Syndrome) background and complaining of infertility against PCOS background were studied being divided into groups. The age gradation of the examined women was significant in the groups. Anamnestic data showed that the age of menarche in all groups of women corresponds to the indicators of a healthy population. In women with PCOS, menstrual disorder in the oligomeric type was found, and the duration of the menstrual cycle was from 36 to 240 days. According to the results of hormonal and ultrasound examination, anovulation was noted in these patients. The obtained results allow predicting the development of infertility in patients with PCOS. Risk factors for the development of infertility in women with PCOS: age older than 30 years, history of infertility, no ovarian surgery, high body mass index (obesity), ovarian volume less than 3 cubic cm, antral follicular number less than 5, PI in ovarian stromal arteries and Low IR indicators were found.
Keywords:
Infertility, Endocrine system, Endometriosis, Polycystic ovary syndrome, Age gradation, Menstrual cycle, dopplerometry, Antral follicular, Stromal artery, Tumorous ovary, Hyperandrogenism syndrome, Prospective analysis, Ovarian cysts, Gonadotropins, Sex steroids, Ovulation, Oligomenorrhea, Amenorrhea, Anovulation, Gastogens, Spontaneous menstruation
Cite this paper: Shokirova Sadokathon Muhammatsolievna, Clinical Prediction of the Development of Infertility in Women with Polycystic Ovary Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 879-884. doi: 10.5923/j.ajmms.20241404.17.
1. Introduction
All over the world, women are one of the main branches of the chain of life. Because women play a major role in the continuation of the human race. A woman becomes pregnant and gives birth to a child one or more times based on the complex structure and uniqueness of her body. Millions of women around the world become mothers every year, but there are women in society who are deprived of such happiness. There are various causes and factors of female infertility. They can be external and internal influences, unfortunate events that happened during life. Among such causes and factors, the most important are various hereditary and acquired diseases. In our research, we have studied several diseases and factors that cause female infertility. We have obtained a number of results mainly by analyzing women's gynecological diseases and studying them in depth, as well as conducting observations and examinations. On the basis of our results, we developed criteria for clinical prediction of the causes of infertility in women directly related to the ovaries, that is, ovarian diseases. We conducted our research mainly by studying the medical history of several women who were treated for infertility with polycystic ovary syndrome and obtaining analysis from them.Polycystic ovary syndrome is an endocrine pathology of the female body, which is characterized by a violation of the menstrual cycle with the absence of ovulation and, as a result, an increase in the level of male sex hormones - androgens [8,9,5,7,10,11]. The disease is also called Stein-Leventhal syndrome or non-tumor ovarian hyperandrogenism syndrome. According to international medical statistics, the prevalence of polycystic ovary syndrome varies between 2.5-8%, and the incidence among teenagers is 3 times less than that of girls and women aged 20-45. The highest incidence was observed in women aged 25-30.
2. Materials and Methods
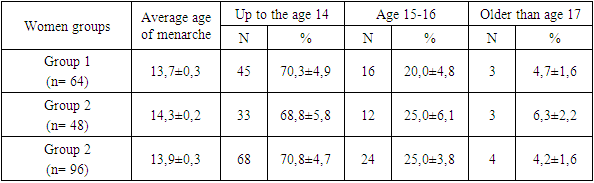
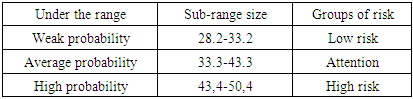
We conducted a prospective analysis among 208 women with infertility in order to achieve the research goal and objectives. The age range was from 20 to 40 years, with a mean age of 29.9±0.5 years, that is, all examined women were of active reproductive age. During the examination, women diagnosed with infertility were divided into 3 groups:Group 1 - 64 women with non-endocrine factors of infertility (tube - peritoneal and endometriosis) without tumor-like formations or functional ovarian cysts;Group 2 – 48 pregnant women with PCOS (Polycystic Ovarian Syndrome);Group 3 - 96 women diagnosed with infertility on the background of PCOS.Patients in groups 1 and 2 had a regular ovulatory menstrual cycle against the background of normal indicators of gonadotropins and sex steroids.All women in group 3 had oligomenorrhoea or amenorrhoea, menstrual cycle disorder of chronic anovulation type, primary or secondary infertility in pregnancy anamnesis. All patients underwent a traditional clinical examination, including anamnesis data, the nature of the menstrual cycle, reproductive function, and a general and gynecological examination. During spontaneous menstruation or when the menstrual cycle was induced with progestogens or COCs, on days 2–4 of the menstrual response, ultrasound examination was performed using a 6.5 mHz transvaginal transducer on the Sonolme Sienmo (Siemens, Germany) machine. The following parameters were determined for each ovary: ovarian volume, number of antral follicles with a diameter of 2-10 mm, dopplermetric indicators of intraovarian blood flow. At the time of examination, all women complained of not becoming pregnant during regular sexual intercourse without using contraceptives for at least 12 months. Age gradation of the examined women did not have significant differences in groups, the average age in group 1 was 26.7 ± 0.4 years, in group 2 - 28.5 ± 0.3 years, and in group 3 - 26.5 ± 0.5 years. The duration of infertility in group 1 is 2.2±0.3 years, in group 2 - 2.8±0.4 years, in group 3 - 2.6±0.3 years. Anamnestic data showed that the age of menarche in all groups of women corresponded to the indicators of a healthy population and averaged 13.7±0.3 years in group 1, 14.3±0.2 years in group 2, and 14.3±0 in group 3, 2 years old. 13.9 ±0.3 years (r>0.05) (Table 1).Table 1. Distribution of women in the compared groups by age of menarche (% of the number of examined)
 |
| |
|
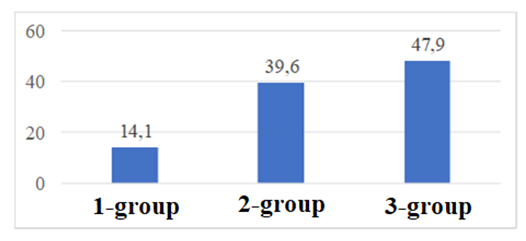
When the characteristics of the menstrual cycle were studied, it was found that oligomeric type of menstrual cycle disorder was found in women with PCOS, and the duration of the menstrual cycle ranged from 36 to 240 days (139.6 ± 1.5 days). According to the results of hormonal and ultrasound examination, anovulation was noted in these patients. Obstetric anamnesis indicators showed that the number of women with first births was similar in all groups. Women with PCOS had a history of severe gestational complications (pre-eclampsia in previous births) and perinatal losses. Infertility was primary in 69% of women in groups 2 and 3 and in 53% of women in group 2. Among the women of groups 1 and 2, the causes of infertility were distributed as follows, the tube-peritoneal factor and endometriosis prevailed, in the 3rd group, in most cases, anovulation was the only cause of infertility, the coexistence of tube-peritoneal factor with anovulation was detected in women who had previously undergone an operation on the ovary. Prior to this study, 47% of women in group 1 and 54% of women in groups 2 and 3 were screened and treated, respectively. The main reasons for previous surgical interventions on the ovaries in women of group 2: endometrioid ovarian cysts - 62.5% (60 women) and retention derivatives (follicular cysts, corpus luteum cysts) - 27.1% (26 women), as well as other good-quality ovarian tumors derivatives (fibroma, teratoma, cystadenoma) - 10.4% (10 women). The size of the removed ovarian cysts ranged from 1 to 5 cm (average 2.4 ± 0.2 cm). Enucleation of ovarian cysts was performed in 20 cases, resection of ovaries in 28 cases. Bilateral ovarian surgery was performed in 26 (54.2%) women, unilateral - in 22 (45.8%) women. In the 3rd group of women with PCOS, ovarian surgery was performed in 22 (22.9%) women, laparoscopic surgery was used in all cases. The performed operations did not lead to the restoration of menstruation and reproductive functions. In the study of accompanying pathology in the examined women, we found that 14.1% of women (9 out of 64) were overweight, in group 2 - 39.6% (19 out of 48 women), and in group 3 this percentage was significantly higher. 3.2 times and was 47.9% (46 out of 94). The resulting data is presented in Chart 1 below.
3. Result and Discussion
As material, a total of 208 cases of women treated with infertility and surgical removal of the ovary were obtained, who underwent outpatient examination at the biopsy department of the Republic of Uzbekistan Center for Pathological Anatomy and the gynecology department of the 2nd maternity complex of Andijan city, and were examined in the MODUS private laboratory.All patients underwent a traditional clinical examination, including anamnesis data, the nature of the menstrual cycle, reproductive function, and a general and gynecological examination. During spontaneous menstruation or when the menstrual cycle was induced with progestogens or COCs, on days 2-4 of the menstrual reaction, an ultrasound examination was performed using a 6.5 mHz transvaginal probe on the Sonolme Sienmo (Siemens, Germany) machine. The following parameters were determined for each ovary: ovarian volume, number of antral follicles with a diameter of 2-10 mm, dopplermetric indicators of intraovarian blood flow. At the time of examination, all women complained of not becoming pregnant during regular sexual intercourse without using contraceptives for at least 12 months. Age gradation of the examined women did not have significant differences in groups, the average age in group 1 was 26.7 ± 0.4 years, in group 2 - 28.5 ± 0.3 years, and in group 3 - 26.5 ± 0.5 years. The duration of infertility in group 1 is 2.2±0.3 years, in group 2 - 2.8±0.4 years, in group 3 - 2.6±0.3 years. When the characteristics of the menstrual cycle were studied, it was found that oligomeric type of menstrual cycle disorder was found in women with PCOS, and the duration of the menstrual cycle ranged from 36 to 240 days (139.6 ± 1.5 days). According to the results of hormonal and ultrasound examination, anovulation was noted in these patients. Obstetric anamnesis indicators showed that the number of women with first births was similar in all groups. Women with PCOS had a history of severe gestational complications (pre-eclampsia in previous births) and perinatal losses. Infertility was primary in 69% of women in groups 1 and 3 and in 53% of women in group 2. Among the women of groups 1 and 2, the causes of infertility were distributed as follows, the tube-peritoneal factor and endometriosis prevailed, in the 3rd group, in most cases, anovulation was the only cause of infertility, the coexistence of tube-peritoneal factor with anovulation was detected in women who had previously undergone an operation on the ovary.The main reasons for previous surgical interventions on the ovaries in 2 groups of women: endometrioid ovarian cysts - 62.5% (60 women) and retention formations (follicular cysts, corpus luteum cysts) - 27.1% (26 women), as well as other benign ovarian formations (fibroma, teratoma, cystadenoma) - 10.4% (10 women). The size of the removed ovarian cysts ranged from 1 to 5 cm (average 2.4 ± 0.2 cm). Enucleation of ovarian cysts was performed in 20 cases, resection of ovaries in 28 cases. Bilateral ovarian surgery was performed in 26 (54.2%) women, unilateral - in 22 (45.8%) women. In the 3rd group of women with PCOS, ovarian surgery was performed in 22 (22.9%) women, laparoscopic surgery was used in all cases. The performed operations did not lead to the restoration of menstruation and reproductive functions. In the study of accompanying pathology in the examined women, we found that 14.1% of women (9 out of 64) were overweight, in group 2 - 39.6% (19 out of 48 women), and in group 3 this percentage was significantly higher. 3.2 times and was 47.9% (46 out of 94). 1 – diagram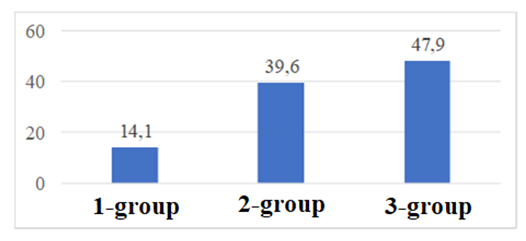 | Diagram 1 |
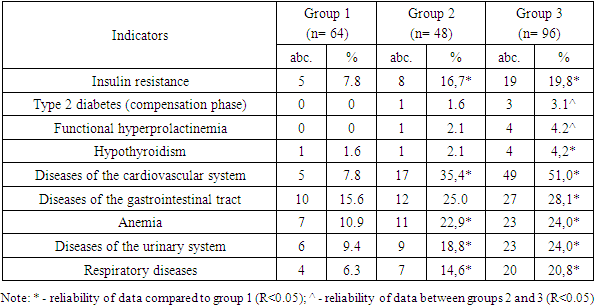
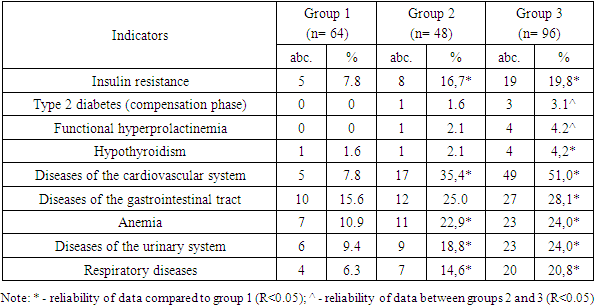
High body mass index indicators are one of the factors that have a negative impact on the course of the disease. The average BMI in group 1 was 25.1±1.3 kg, in group 2 - 28.9±1.8 kg, in group 3 - 31.2±2.1 kg. When comparing TVI indicators, it was proved to be significantly higher in women of groups 2 and 3 (R<0.05-0.01, respectively). It can be noted that during the interview, women in group 3 did not record positive results when trying to reduce their weight. The somatic condition of the examined women is characterized by the presence of diseases of the cardiovascular system, which are significantly more frequent in groups 2 and 3 (R<0.05). Gastrointestinal diseases are also significantly more common in patients with PCOS (R<0.305). It was found that patients in groups 2 and 3 have more frequent diseases of the urinary system and respiratory organs than in group 1 (R<0.05). Also, in these groups, anemia was more often recorded in a somatic state compared to group 1 (R<0.05).Table 2. Somatic condition of the examined women
 |
| |
|
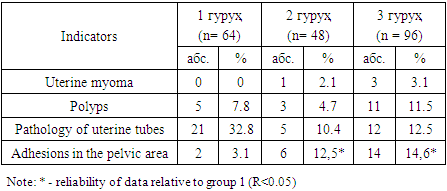
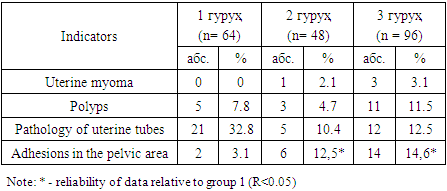
In women in groups 2 and 3, insulin resistance with endocrine pathology was noted significantly more often, their percentage was 16.7% and 19.8%, respectively, while in group 1 this percentage was almost 2.5 times lower (r<0.05). Type 2 diabetes and functional hyperprolactinemia were found only in women with PCOS (r<0.05). Adhesions in the pelvic area prevailed among gynecological diseases in women with PCOS (12.5% and 14.6% in groups 2 and 3, respectively). Polyps and pathologies of fallopian tubes were also recorded in women of this group. The obtained data are presented in Table 3.Table 3. Frequency of occurrence of gynecological diseases in examined women
 |
| |
|
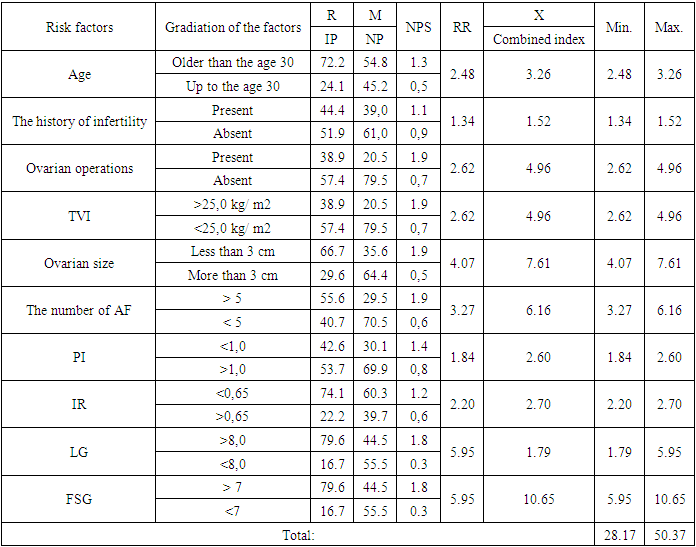
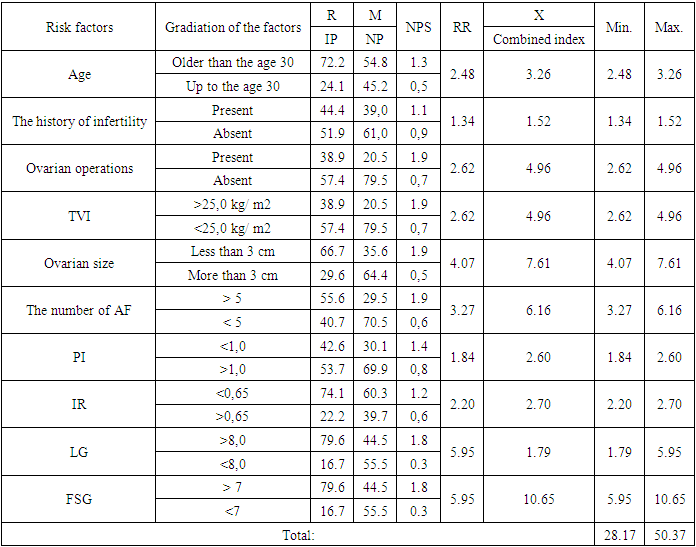
Thus, we identified characteristic features for predicting pregnancy in PCOS, identified important risk factors: age under 30 years, presence of high TVI, aggravated somatic condition, presence of gynecological diseases. We developed a prognostic matrix for the development of infertility in patients with PCOS. The basis for the development of the prognostic scale is a modification of the probabilistic Bayes method - the method of normalized intensive indicators (NIP) [Shigan E.N. Forecasting and modeling methods in socio-hygienic research. - M., 1986. - 207 p.] with the calculation of prognostic, weight indices, normalized intensive and integral indicators. In order to create a prognostic matrix, comparative indicators of the predicted event were obtained according to the gradations of the most important factors. The importance of the factors and their levels is the relative risk indicator (relative risk - RR), which is the product of the NIP and the weight of the factor. The importance of factors and their gradations were determined using the relative risk index (R). This indicator is the ratio of the maximum intensity indicator (c) to the minimum (d) in each individual factor (R = c / d). If the factor does not affect, it is equal to one. The higher the R, the greater the importance of the factor for the development of infertility in women with PCOS. Subsequently, logistic regression analysis with stepwise selection was performed to identify independent predictors of infertility in women with PCOS, which included the following parameters: age, anamnestic data, gynecological examination, laboratory signs of ovarian reserve (FSG and LG) and ultrasound examination. (ovarian size and number of antral follicles). The results are presented in Table 4.Table 4. A predictive matrix for the development of infertility in patients with PCOS
 |
| |
|
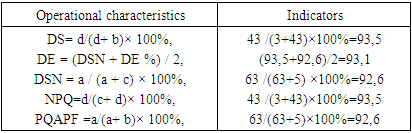
In addition to the prognostic table, based on the obtained set of factors, we determined the range of possible quantities for the development of infertility in patients with PCOS. The possible risk range was determined as follows. In the prognostic table, we find the minimum quantities of the prognostic coefficient (X) for each factor and summarize them. This value is the initial quantity of the risk of this pathology. For example, for a comprehensive evaluation of the development of infertility in patients with PCOS, table 5 shows the minimum and maximum quantities of prognostic indices (X) for all factors: the minimum quantity is 28.2; the maximum quantity is 50.4. In this case, the range of development of infertility in patients with PCOS is in the range of 28.2-50.4. It follows that the higher the quantity of the standard integrated indicator due to the influence of the set of factors under study, the higher the probability of infertility in patients with PCOS and the more reason to include it in the risk group. In this regard, we determined the range of possible risk (28.2-50.4), as well as sub-ranges: weak (28.2-33.2), medium (33.3-43.3) and high (43.4 -50.4) risk of developing infertility in patients. with PCOS. Thus, the threshold quantities of the final prognostic coefficients and the risk group for the occurrence of an unfavorable reproductive prognosis were determined (Table 5).Table 5. Quantity of lower ranges and groups of individual forecasts of the risk of adverse reproductive prognosis
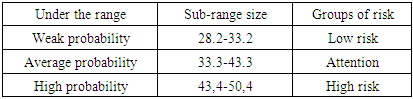 |
| |
|
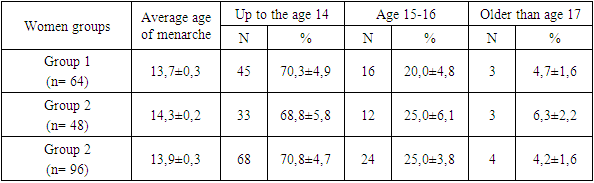
To determine the diagnostic value of the model for evaluating the development of infertility in patients with PCOS, the following were calculated: diagnostic specificity (DS), diagnostic efficiency (DE), diagnostic sensitivity (DSN), negative predictive quantity (NPQ), predictive quantity according to positive formulas (PQAPF):DS = d/(d+ b)× 100%,DE = (DSN + DE%) / 2,DSN = a / (a + c) × 100%,NPQ=d/(c+ d)× 100%,PQAPF=a/(a+ b)× 100%,where a is a real positive result,b - false positive result;c - false negative result;d - a true negative result.We analyzed data from 144 women with PCOS to test a prognostic matrix for comprehensive assessment of complication risk. Thus, when calculating the size of the lower range, 46 women were assigned to the favorable prognosis group, 35 to the focus group, and 65 to the unfavorable prognosis group. In the observation dynamics, in the group with a favorable prognosis, infertility developed in 3 women (6.5%) - a false negative result, pregnancy occurred in 43 women (93.5%) - a true negative result; in the group of high-risk women, 5 (7.7%) women recorded pregnancy - a false positive result, 63 women (92.3%) suffered from infertility - a true positive result 6 - in the table.Table 6. Diagnostic quantity to ensure the safety of recommendations for developing infertility in patients with PCOS
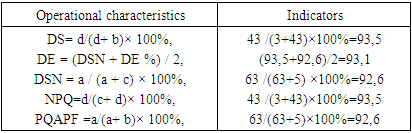 |
| |
|
According to the obtained data, shown in Table 6, DS is 93.5%, DSN - 92.6% and DE - 93.1%. Thus, one of the important components of an effective strategy for predicting the development of infertility should be an algorithm for comprehensive identification of clinical signs of this pathology in patients with PCOS. Identification of risk factors suggested in patients with PCOS implies greater clinical severity and higher risk of infertility. Also, one of the important components of an effective strategy for predicting the development of infertility should be an algorithm for comprehensive identification of clinical signs of this pathology in patients with PCOS. Identification of risk factors suggested in patients with PCOS implies greater clinical severity and higher risk of infertility.In conclusion, 45% of patients with infertility problems underwent surgery for benign ovarian cysts (endometrioid cysts, functional cysts, teratomas, etc.), and 63% of them underwent resection of both ovaries mainly laparoscopically. The results obtained from our studies allow us to predict the development of infertility in patients with PCOS. Risk factors for the development of infertility in women with PCOS: age older than 30 years, history of infertility, no ovarian surgery, high body mass index (obesity), ovarian volume less than 3 cubic cm, antral follicular number less than 5, PI in ovarian stromal arteries and Low IR indicators were found.
References
| [1] | Adamyan L.B., Kulakov V.I. Endometriosis. -M.: Medicine, 2018. 317 p. |
| [2] | Baskakov V.P., Tsvelev Yu.V., Kira E.F. Endometrioid disease. SPb.: Publishing house H-J1, 2012. - 448 p. |
| [3] | Belkina A.A. Tubal-peritoneal infertility in women // Problems of reproduction. 2010. |
| [4] | Damirov M.M. Adenomyosis: clinic, diagnosis and treatment. M.: Tver: Triada, 2012. - 294 p. |
| [5] | Pshenichnikova T. Ya. Infertility in marriage. M. : Medicine, 2011. - S. 200-206. |
| [6] | Transvaginal color Doppler: infertility, assisted reproduction, obstetrics / ed. A. Kuryak, A. Mikhailova, S. Kupeshic. SPb. : Petropolis, 2011. - S. 44-68. |
| [7] | Hudson B., Pepperell RJ. Infertility problem. M. : Medicine, 2013. -S. 7-14. |
| [8] | Kalenitskaya JI.B., Kurganov S.A., Makhotina N.E. Dopplerography of the cervix in the ZD-TVUS mode for planning organ-preserving operations // Ultrasonic and functional. diagnostics.. 2008. - No. 2. - S. 77 - 78. |
| [9] | Medvedev M.V., Ozerskaya I.A. Ultrasound examination of the fallopian tubes // Clinical guide to ultrasound diagnostics. M., 2007. - T. 3. - S. 175 - 200. |
| [10] | Controversies in Obstetrics and Gynecology: Intern. Congr. Paris, 2011. |
| [11] | Deichert U., Schleif R., van de Sandt M., Juhnke J. Transvaginal hystero-salpingo contrast sonography (HyCoSy) compared with conventional tubal diagnostics // Human Reproduction. - 2009. - Vol. 4. - P. 418 - 424. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML