-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 863-866
doi:10.5923/j.ajmms.20241404.13
Received: Mar. 3, 2024; Accepted: Mar. 23, 2024; Published: Apr. 2, 2024

Endoscopic Diagnosis and Treatment Algorithm of Acute Biliary Pancreatitis
Allanazarov Allanazar Khudashkurovich, Tadjitdinova Guzal Gayratovna
Urganch Branch of Tashkent Medical Academy, Urgench, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article includes 57 patients aged 19 to 84 years with cholelithiasis and acute biliary pancreatitis, the average age is 54.8+12.4 years, of which 34 are women (59.7%) and 23 are men (40.3%). The results obtained make it possible to use the algorithm for the diagnosis and treatment of acute biliary pancreatitis to more effectively identify and eliminate the cause of the disease in the early stages, relieve mechanical jaundice syndrome and prevent the development of fatal forms of acute biliary pancreatitis and its complications. Simultaneous use of endoscopic diagnostics and endosurgery in patients with cholelithiasis and acute biliary pancreatitis shows the possibility of achieving good results and reduces the range of contraindications to surgery in such tumors.
Keywords: Laparoscopy, Gallstone disease, Mechanical jaundice, Acute biliary pancreatitis, Endoscopic papillosphincterotomy
Cite this paper: Allanazarov Allanazar Khudashkurovich, Tadjitdinova Guzal Gayratovna, Endoscopic Diagnosis and Treatment Algorithm of Acute Biliary Pancreatitis, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 863-866. doi: 10.5923/j.ajmms.20241404.13.
Article Outline
1. Introduction
- Acute pancreatitis (AP) has a tendency to increase, and according to world statistics, it is from 200 to 800 cases per 1 million people per year. Among them, the form of acute pancreatitis with a necrotic focus occurs in 15-20% of patients.Endoscopic retrograde cholangiopancreatography (ERXPG) with endoscopic papillosphincterotomy (EPST) is indicated only for patients with signs of mechanical jaundice and dilatation of the bile ducts, or when conservative measures are ineffective for 48 hours [6,7]. Other authors emphasize the need to allow endoscopic retrograde cholangiopancreatography (ERXPG) in the first stage of biliary hypertension, followed by endoscopic papillosphincterotomy (EPST), which is certainly not possible in emergency surgery [1,2,3]. Therefore, visual assessment of the condition of the large papilla of the duodenum and methods of determining indications for endoscopic papillosphincterotomy without contrast X-ray examinations are of particular importance.As a result of endoscopic papillosphincterotomy, the sphincter apparatus of the large papilla of the duodenum is partially destroyed [4,5]. Therefore, the problem of studying the long-term results of the use of endoscopic papillosphincterotomy in patients with acute biliary pancreatitis is the extent to which sphincter dysfunction affects health-related quality of life [7,8,9].The purpose of the study. Improving the diagnosis and treatment outcomes of patients with acute biliary pancreatitis through early diagnosis and development of an endo-surgical treatment algorithm [10,11].
2. Research Materials and Methods
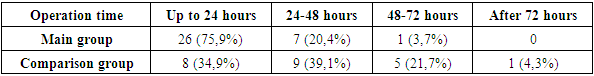
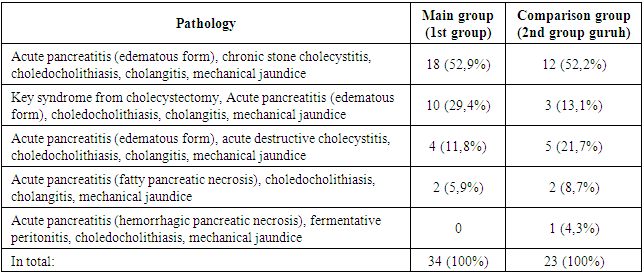
- The results of treatment of patients treated in the thoracic and endo-surgery department of the multidisciplinary medical center of the Khorezm region were analyzed in order to achieve the set goal and solve the tasks. Patients with gallstone disease and acute biliary pancreatitis admitted to the thoracic and endo-surgery department in 2016-2023 were accepted as research subjects. 57 people aged 19 to 84 years, average age 54.8+12.4 years, including 34 women (59.7%) and 23 men (40.3%). In 6 patients (10.5%) the destructive form of O'BP was determined. Hypertension (13.5%), coronary artery disease (12.4%) and diabetes (5.6%) prevailed among co-morbidities. Patients were selected based on the analysis of the registration logs of research results, with the method of continuous control for comparative assessment of changes in the large duodenal suction zone in OP and to improve the classification of changes detected in OP in this zone.In a controlled long-term prospective clinical study, treatment outcomes were compared between endoscopic (group I, primary, n = 34) and standard (group II, control, n = 23) treatment groups.
3. The Results of Our Research
- Reactive gastro-duodenitis (100%), decreased gastroduodenal motility (74%), duodeno-gastric reflux (60%), pyloric and insufficiency of cardiac sphincters (68%), lymphangioectasia (55%), acute gastroduodenal ulcers (25%) were detected.The main endoscopic symptom of acute biliary pancreatitis is the incomplete drainage of the stomach and pancreatic juice into the duodenal cavity as a result of obturation of gallstones in the large duodenal duct; Because of this, its surface is smooth and shiny, the volume and tension of the large duodenal tube increases sharply. With a pronounced bulge, the large duodenal tube occupies 2/3 of the duodenum. The elasticity of the mucous membrane covering the large duodenal tube has decreased. According to endo-palpation, the papilla has a dense consistency and practically does not move when pressure is applied to it. Longitudinal folds, which are the contour of the intraduodenal part of the common bile duct, are thickened and tense. In a number of cases, scarring is observed as a result of pushing a stone or a stone in the mouth of the large duodenal tube. According to our data, in 100% of cases in O'BP there is obstruction of the large duodenal duct with stones, in 76% - scar papillostenosis, in 64% - hypertension of the intramural part of the common bile duct, narrowing of the parapapillary area In 22%, 6% - parapapillary diverticulum, large duodenal duct (KDS) adenoma - 4%, 3% - cases after gastrectomy according to Billrot II.Combined endoscopic papillosphincterotomy (EPST) was performed after detecting stone obstruction of the CDS. First, the dissection needle or the end electrode was cut and opened along the upper part of the KDS in the direction of the longitudinal fold to the ampullae cavity at 11-12 o'clock. The tissues under the stone were completely separated. In this case, the stone that affected the ampulla of KDS is removed in most cases, in some cases deep papillostenosis was caused by obturation of KDS with microliths, "slag" or thickened bile fluid.Endoscopic retrograde cholangiography (ERXG) showed ampullary compartment concretions (100%), common bile duct dilatation (100%), common bile duct concretions (33%), isolated choledochal stones (22%), multiple choledocholithiasis (11%), complicated choledocholithiasis (2%), Mirizzi syndrome (1%), cholecystolithiasis (10%), distal choledochal stenosis (14%), cholangitis symptoms (84%), long bile "False grass bag" in the form of a sack bag - was detected in (3%) cases.Thus, the above-mentioned endoscopic technologies allow effective detection and treatment of acute biliary pancreatitis in patients at an early stage. In this case, the high efficiency of the treatment is achieved by the minimal trauma of the endoscopic operation and by performing additional cholangioscopy to identify the remains of stones in the common bile ducts and remove them immediately. Based on the obtained results, we created the following algorithm for the diagnosis and treatment of acute biliary pancreatitis.Algorithm of endoscopic diagnosis and treatment of acute biliary pancreatitis caused by obstruction of the duodenum and common bile duct.
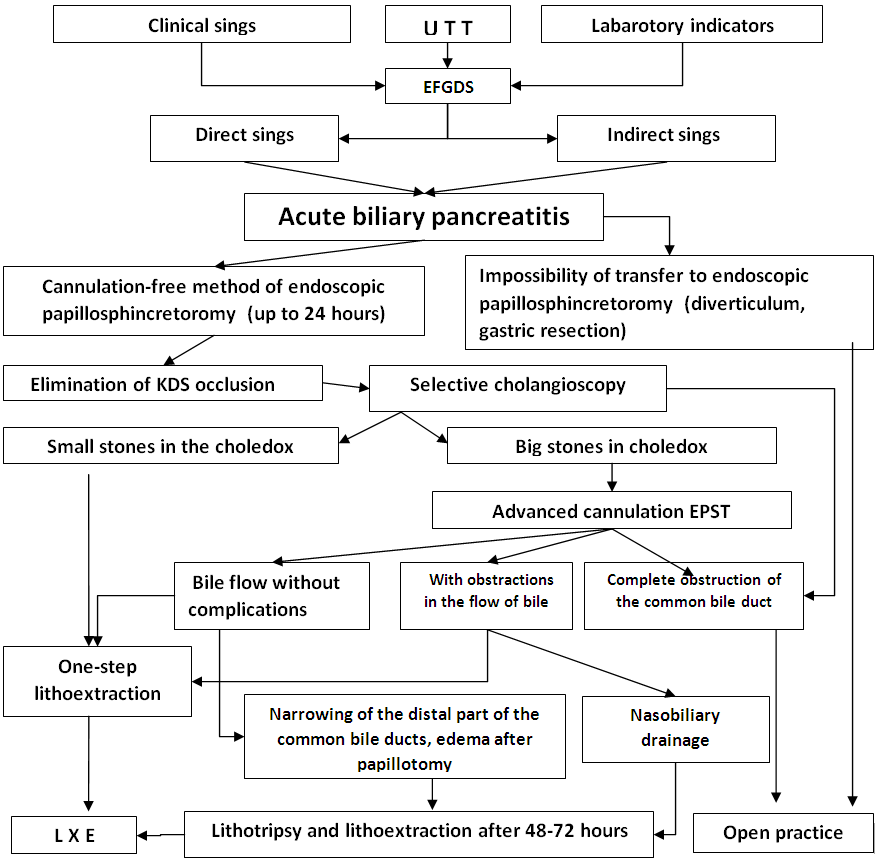 | Figure 1. Acute biliary pancreatitis |
|
|
4. Conclusions
- 1. The main reason for the development of acute biliary pancreatitis is the obstruction of the large papilla of the duodenum and the common bile duct with stones. In such cases, endoscopic examinations revealed the complete absence of bile and pancreatic juice in the duodenum.2. The optimal period for the use of endoscopic methods for the diagnosis and treatment of acute biliary pancreatitis is the first 24 hours after the onset of clinical symptoms of the disease. An indication for combined endoscopic papillosphincterotomy is the absence of bile flow to the duodenum, gallstones and acute occlusion of the common bile ducts and large papilla of the duodenum.3. Using the algorithm for diagnosis and treatment of acute biliary pancreatitis allows to more effectively identify and eliminate the cause of the disease in the early stages, stop the obstructive jaundice syndrome and prevent the development of fatal forms of acute pancreatitis and its complications. The use of endoscopic methods allows reducing the length of stay of patients in the hospital from 22.1 6.3 to 8.6 2.2 days, and the mortality rate - from 9.3% to 3.3%.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML