-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 850-853
doi:10.5923/j.ajmms.20241404.10
Received: Mar. 7, 2024; Accepted: Mar. 29, 2024; Published: Apr. 2, 2024

Miscarriage in Patients with Luteal Phase Deficiency
Asatova M. M., Akhrorova Sh. O.
Republican Specialized Scientific and Practical Medical Center for Obstetrics and Gynecology, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article discusses the problem of miscarriage due to hormonal changes, in particular luteal phase deficiency, which leads to impaired embryo implantation and early pregnancy loss. Also, the frequency of miscarriage was assessed depending on the pathogenetic mechanisms of the formation of luteal phase deficiency. The study included 63 women with a history of recurrent miscarriage. The patients underwent clinical, anamnestic, gynecological and hormonal examinations. The results of the studies showed that the leading cause of luteal phase deficiency from endocrine causes is pathology of the thyroid gland and accounts for 61.9%.
Keywords: Miscarriage, Luteal phase deficiency, Hypothyroidism, Hyperprolactinemia
Cite this paper: Asatova M. M., Akhrorova Sh. O., Miscarriage in Patients with Luteal Phase Deficiency, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 850-853. doi: 10.5923/j.ajmms.20241404.10.
Article Outline
1. Introduction
- Recurrent pregnancy loss (RPL) or miscarriage is one of the important clinical conditions in reproductive medicine, requiring not only diagnostic testing and therapeutic intervention, but also assessment of the risk of relapse [1,2,4,6,7].The rate of miscarriage currently makes up 20% in the general population. 80% of miscarriages occur before 12 weeks of gestation, with miscarriage rates dropping sharply after the first trimester. A miscarriage that occurs after a positive result of human chorionic gonadotropin (HCG) test or elevated serum beta-hCG level but before ultrasound or histological confirmation is defined as a biochemical loss occurring before 6 weeks of gestation, whereas a clinical miscarriage is a loss at positive ultrasound examination or histological signs of intrauterine pregnancy [3,5,7,8,10].Various etiological factors responsible for recurrent miscarriage include anatomical, genetic, endocrinological, immunological, infectious and other reasons. In the etiology of early pregnancy loss, the leading role belongs to hormonal disorders in the pregnant. Endocrinological disorders can be caused by polycystic ovary syndrome, hyperprolactinemia, luteal phase deficiency, thyroid dysfunction, hyperandrogenism, which contribute to miscarriage. Luteal phase deficiency syndrome (LPD) occurs in 70% of women suffering from miscarriage, either as an underlying cause or as a consequence of recurrent miscarriage [2,9,11,15,16]. Hyperandrogenism also occupies a significant place among the causes of miscarriage and averages 21-48%. One of the endocrine factors of miscarriage may be dysfunction of the thyroid gland. Hypo and hyperthyroidism lead to suppression of ovarian function and the development of luteal phase defect. With hyperprolactinemia, approximately 25% of patients have ovulatory cycles accompanied by LPD. The most common endocrine factor in miscarriage is LPD. Luteal phase deficiency is insufficient production of progesterone by corpus luteum (yellow hormone-secreting body), and these two concepts, LPD and miscarriage are inextricably linked. The ineffectiveness of ongoing measures of conservation therapy for RPL largely depends on the failure to clarify the main reasons for the formation of LPD [12,13,14]. Luteal phase deficiency is more often associated with chronic endometritis due to intrauterine interventions in women with recurrent pregnancy losses; therefore, the real-time polymerase chain reaction method “Femoflor-screen” was included in the article.Purpose of the study: to evaluate the pathogenetic mechanisms of the formation of luteal phase deficiency in women with miscarriage.
2. Materials and Methods of the Study
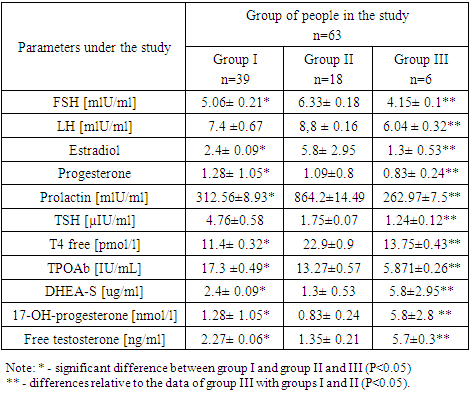
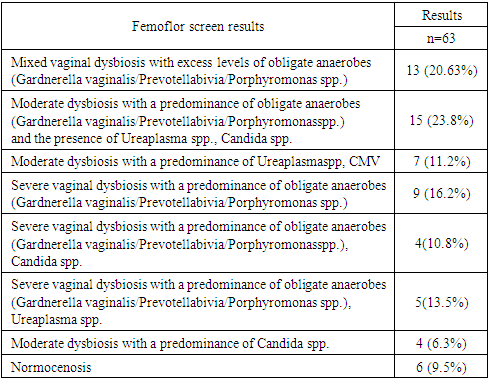
- The study included 63 non-pregnant women aged 18 to 35 years. The inclusion criteria were: women with a history of recurrent miscarriage and changes in the results of hormonal studies at the stage of preconception preparation, who came to the advisory clinic of the Republican Specialized Scientific and Practical Medical Center for Obstetrics and Gynecology of the Ministry of Health of the Republic of Uzbekistan. Exclusion criteria were: smoking, pregnancy, systemic autoimmune diseases, antiphospholipid syndrome, diabetes, uterine malformations, uterine fibroids.The participants in the study underwent an analysis of anamnestic information, a gynecological examination, a blood test collected on an empty stomach from 8 to 10 a.m. from the ulnar vein for the content of FSH, LH, Prolactin, TSH, TPOAb, T4 free, DHEA, 17-OH-progesterone, Estradiol, Progesterone, Free testosterone.As part of the study, microbiological analysis of vaginal discharge from its posterior fornix was also performed. Bacterioscopy was performed after Gram staining of vaginal smears. The results were assessed by the absence or presence of signs of inflammation. Using a cultural study, the presence of growth and sensitivity to antibiotics of facultative anaerobic microflora was clarified. To assess the microbiocenosis of the vagina, the real-time polymerase chain reaction method “Femoflor-screen” was used, with the help of which the total bacterial mass, the number of Lactobacillus spp., facultative anaerobic microorganisms, 8 taxa of obligate anaerobic microflora, mycoplasma, fungi of the genus Candida, viruses (HSV-2, CMV, HSV-1) were determined, as well as colposcopy, ultrasound examination of the uterus and appendages were conducted.Statistical processing of the research results was carried out with the help of generally accepted methods using a personal computer, Microsoft Word 2016, Microsoft Excel.
3. Results and Discussions
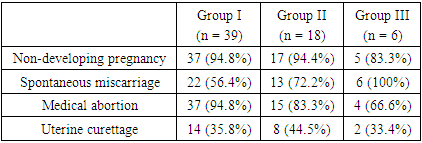
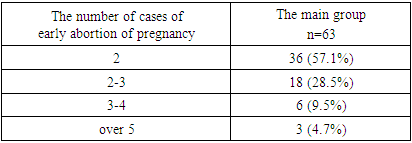
- A total of 63 patients with recurrent miscarriage were examined. The average age of the patients was 25.8±3.28 years. The average age at menarche was 13±2 years for the majority of subjects. The average age at the onset of sexual activity was 17.5±9.5 years.The main complaints when surveying patients of all groups were: 49 (77.8%) noted discharge from the genital tract; 17 (26.9%) noted pain in the lower abdomen and lower back; 16 (25.3%) noted menstrual irregularities; Patients from group 1 complained of drowsiness, fatigue, dry skin and constipation; in group 2, almost half of patients had discharge from the nipples and headaches. Group 3 of patients showed signs of virilization (tall stature, broad shoulders, narrow hips, hirsutism).
|
|
|
|
4. Conclusions
- Thus, the results of the studies indicate that the leading cause of the formation of luteal phase deficiency from endocrine factors is pathology of the thyroid gland (61.9%).Hyperprolactinemia was detected in 28.5% of patients, the remaining proportion was occupied by patients with congenital dysfunction of the adrenal cortex and amounted to 9.5%. Often, the results of hormonal studies are not very informative, as they are subject to daily fluctuations, which pushes us to further in-depth study of this pathology.According to data obtained from PCR using the real-time Femoflor screen method, vaginal dysbiosis was confirmed in 57 (90.4%) patients. The leading place was occupied by obligate anaerobic microorganisms (Gardnerella vaginalis/Prevotellabivia/Porphyromonas spp.). In 2nd place are Uresplasmaspp., then Candidaspp. In 6 women, normocenosis was detected with the level of Lactobacillus spp.Based on the results, we can conclude that miscarriage is often accompanied by vaginal dysbiosis due to intrauterine interventions. Clarification of the mechanisms of formation of LPD in case of miscarriage, which can be identified and the correct etiotropic treatment prescribed, which is the prevention of early perinatal losses.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML