Radjabova Azizakhanum Farmanovna
Bukhara State Medical Institute named after Abu Ali Ibn Sina, Bukhara, Uzbekistan
Correspondence to: Radjabova Azizakhanum Farmanovna, Bukhara State Medical Institute named after Abu Ali Ibn Sina, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The development of clinical immunology has become of great importance in understanding the pathogenesis of diseases of various etiologies. Knowledge of pathogenesis ensures accurate diagnosis and timely treatment, increases the medical, social and economic effect. In the course of our research, we sought to determine and evaluate the influence of the parameters of humoral immunity and cytokine status on the immune system of patients with chronic diseases of the gastrointestinal tract in clinical immunology in order to determine the course and prognosis of chronic generalized periodontitis in patients with peptic ulcer disease of the gastrointestinal tract. In patients with gastrointestinal ulcer disease (18-69 years old), the diagnosis of chronic generalized periodontitis was verified, oral fluid was collected for analysis, and the parameters of humoral immunity and cytokine status were assessed.
Keywords:
Periodontium, Periodontitis, Cytokines, Cytokine status, Immunoglobulin, Local immunity, Oral fluid, Humoral immunity, Immune response
Cite this paper: Radjabova Azizakhanum Farmanovna, Results of Immunological Study before and After Treatment of Patients with Chronic Diffuse Periodontitis on the Background of Gastrointestinal Disease Ulcer, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 813-818. doi: 10.5923/j.ajmms.20241404.03.
1. Introduction
Against the background of common somatic diseases, one of the most difficult problems of dentistry remains due to difficulties in the diagnosis and treatment of diseases of the oral mucosa. Against the background of diseases of the digestive tract, the prevalence of inflammatory diseases of the oral cavity among the general population is 30-35%, while in diseases of the ulcerative intestine it increases by 40-50%.According to the classification of the European Health Organization, when diagnosed, diseases of the stomach and duodenum wound remain relevant among diseases of the digestive tract caused by a particular cause. The prevalence of diseases of the gastrointestinal tract is in the range of 250 to 300 per 100,000 inhabitants. In European countries, their steady growth is observed [1,2,3,4]. Differential diagnosis of these diseases can be difficult when accompanied by inflammation of the large intestine, where the endoscopic and histological symptoms of both nosologic forms are partially manifested and coincide. Correct diagnosis will be necessary due to the peculiarities of the choice of drugs, treatment and the scale of surgical intervention [5,6,7,8].In the development of recurrent chronic inflammatory processes in the oral cavity, pathological diseases of the intestine at all levels create the necessary conditions. All symptoms of periodontitis and other oral diseases that are spread in the oral cavity of patients with a sore background are common [9,10].The latest research results of the oral mucosa (LROM) confirm the hypothesis of an autoimmune process in diffuse parodontitis. To make the right diagnosis, an effective examination to construct an effective treatment algorithm, and the elimination of treatment methods [11,12,13,14].
2. Research Materials and Methods
Our research was carried out on the basis of the Bukhara regional Multidisciplinary Medical Center in 2020-2021 and in patients with gastrointestinal ulcer disease. During our study, a total of 582 patients with gastrointestinal ulcer disease were examined in Bukhara city and district polyclinics with a residence address "d". Of these, 150 patients aged 18-69 with chronic diffuse periodontitis with gastrointestinal ulcer disease were selected for research purposes. Of this, 58 were male patients and 92 were female patients. 30 patients with chronic diffuse periodontitis but not gastrointestinal ulcer disease were also involved, as well as 30 healthy volunteers for the control group.During the study, we divided our observation group patients into 3 large groups:The main group-patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease, were divided into groups I, II and III, depending on the method of treatment;Comparison group-patients with chronic diffuse periodontitis without gastrointestinal ulcer disease, divided into Group I, Group II and Group III, depending on the method of treatment;The control group is a group of healthy volunteers.
3. Analyzes and Results
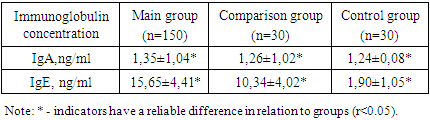
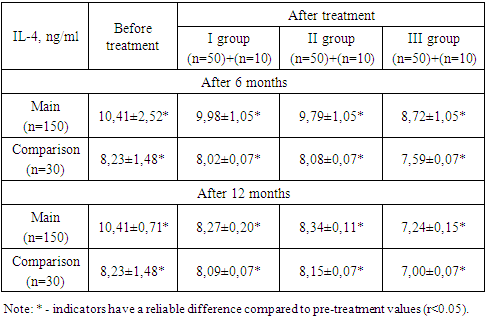
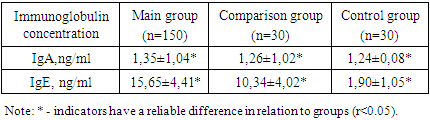
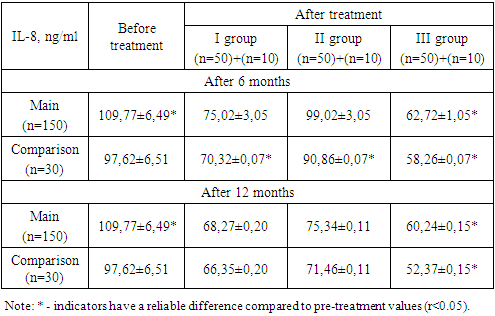
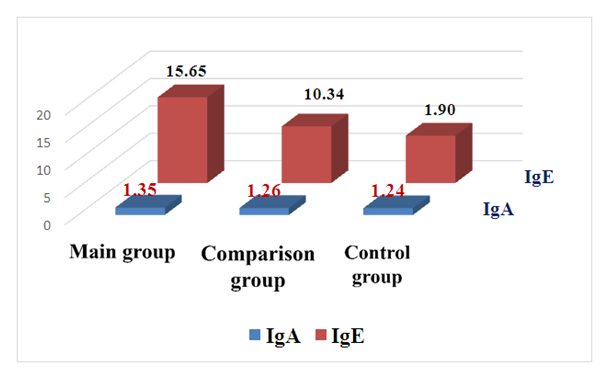
In patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease, a concentration of cytokines was found. During the study, oral fluid was taken from patients for this and studies were carried out using IFA. In this, test-systems made from the Tamon" tsitokin " LLC (Spb, RF) were used. With them, the concentrations interleukin-4 (IL-4) and interleukin-8 (IL-8) were determined.In order to determine the Holt of humoral immunity in patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease, patients were identified using IGA and IgE concentration IFA in oral fluid. In this, the test-kits" vektor Best " (Novosibirsk, RF) LLC were used.In order to make comparative analysis of the results of the study easy, at the initial stage, the general indicators of chronic disseminated periodontitis in patients against the background of gastrointestinal ulcer disease were brought up in comparison with the control group. The results obtained showed that the concentration of immunoglobulins in the oral fluid of all studied patients was significantly higher in observation groups and in comparison with the control group.Table 1. Indicators of the concentration of immunoglobulins in the oral fluid of patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study
 |
| |
|
 | Figure 1. Immunoglobulin concentration indicators |
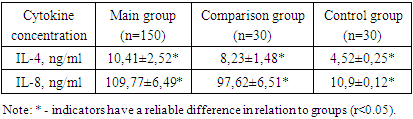
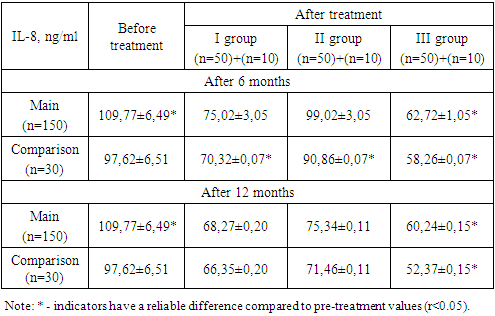
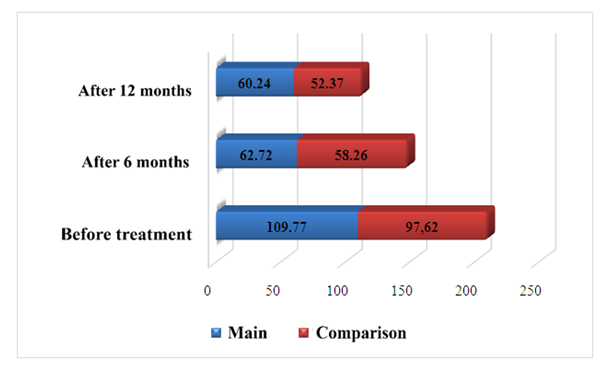
IgA levels were found to be significantly higher at 0.11 ng/ml compared to control group indicators in the main group of patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease-1.24±0.09 ng/ml (p0,05) versus 1.35±0.08 ng/ml, respectively. Given IgA's 10% presence of all immunoglobulins, participation in anti-inflammatory primary and secondary immune response, its primary role in providing local immunity, it can be substantiated that they increase quantitatively. The presence of IgA in large quantities in the serum of the patient indicates a high level of production on the surface of the mucous membrane. This increase in immunoglobulin is a target of activation of the body's immune system, including local immune factors.IgE is characterized by being found in vertebrates unlike other immunoglobulins, providing the body's individual immune response to an antigen (excitatory) that has fallen into the body, having certain biological activity (allergies) not participating in primary and secondary immune responses like other immunoglobulins, the patient being found in very low amounts in serum (0.4% of all immunoglobulins). It is also undeniable that there are other infections in the body based on clinical-laboratory tests, taking into account the high IgE content in most cases.The results obtained showed that patients showed an increase in IGE in oral fluid by 13.75 ng/l compared to control group parameters - 1.90±1.05 g/l (p0,01) against 15.65±4.41 g/l, respectively. Thus, patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease belong to the control group of the main immunoglobulin concentrations in the oral fluid, healthy people who did not have this pathology in their Anamnesis were distinguished by a convincing high in comparison with parameters, during the study IGA was significantly more than 0.11 ng/ml (p0,005) and IgE 13.75 ng/ml (p0, 05).It is known that cytokines are molecules of a small peptide nature, with high information content, carrying information among special and non-special immune system cells, providing a primary and secondary immune response, as well as controlling. Quantitative changes in anti-inflammatory and anti-inflammatory cytokines indicate the level of development of the inflammatory process, acquired pathology in the body and pathological conditions.Among the anti-inflammatory cytokines, delimitation of this pathological process, interleukin-4 (IL-4), which is important in ending the immune response, induces differentiation of Th0-cells (initial T-helpers) into Th2-cells, as well as one of the cytokines that apply inflammation, interleukin-8 (IL-8), were identified. The results obtained showed that IL-4 and IL-8 were within the generally accepted norm or reference indicators in control group humans (table 2), showing a result close to one in practical terms - 4.52±0.25 ng/ml and 10.09±0.12 ng/ml respectively over the parameters studied. Table 2. Patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study group are indicators of cytokine status in oral fluid
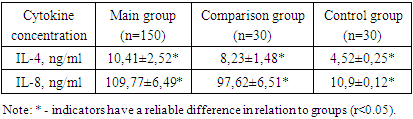 |
| |
|
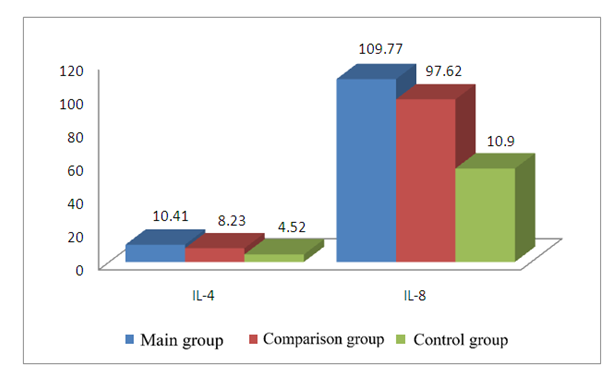 | Figure 2. Cytokine status indicators during the study |
IL-4 was disproportionate in patients with an average increase of 5.89±2.27 ng/ml compared to healthy people of the control group, with multiple increases in IL - 8 cytokine – 109.77±6.49 ng/l-(P0,01) (figure 2).Taking into account the above, anti-inflammatory IL-4 and immunological status-determining IL-8 cytokines were recommended as additional diagnostic and prognostic immunological criteria.
4. Results after Treatment
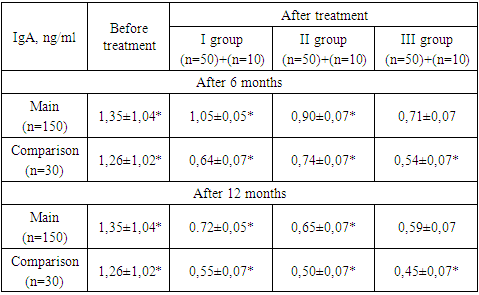
Group 1 of patients of the main group received only antibacterial therapy, group 2 treated only with propolis tincture, and Group 3 treated both antibacterial and propolis tincture with complex treatment. During the study, the drug Lycopide® (Licopid) was used for immunotherapy purposes in the main group of patients (150 people). The results were checked after 6 and 12 months. The results obtained can be said that in all treated patients, the concentration of immunoglobulins in the patient's oral fluid decreased convincingly after treatment. 3-listed in Table view. Table 3. Indications of post-treatment outcomes of IgA (g/l) in oral fluid for patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study
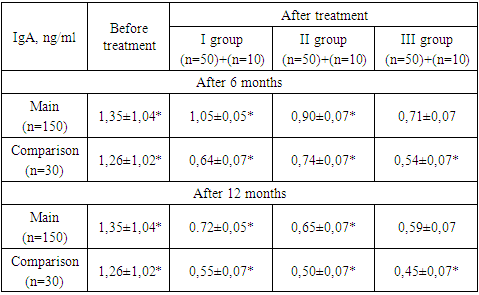 |
| |
|
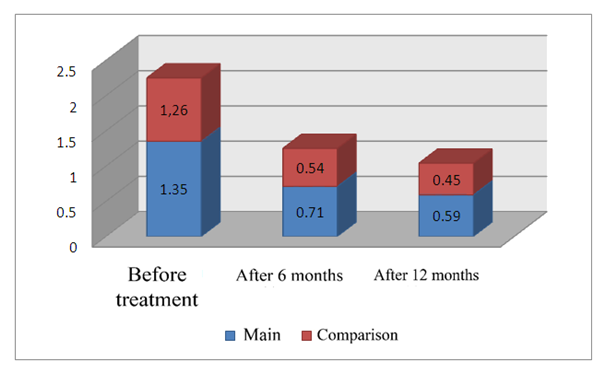
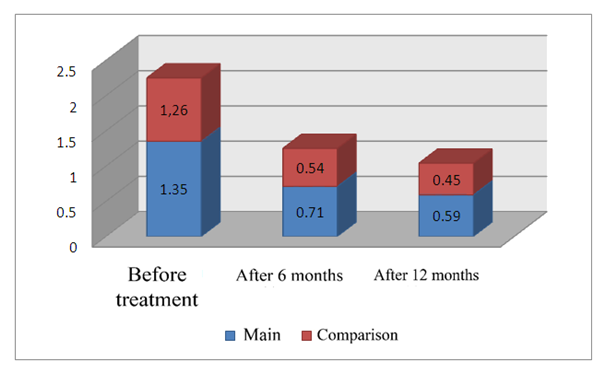 | Figure 3. Results of IgA (ng/ml) in oral fluid in complex treatment in patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease |
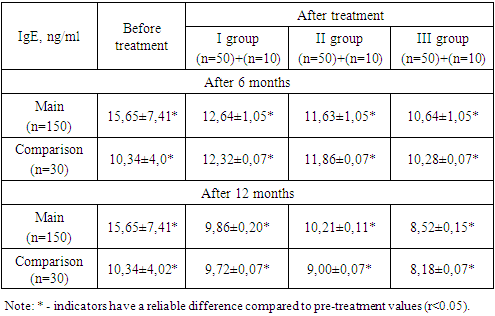
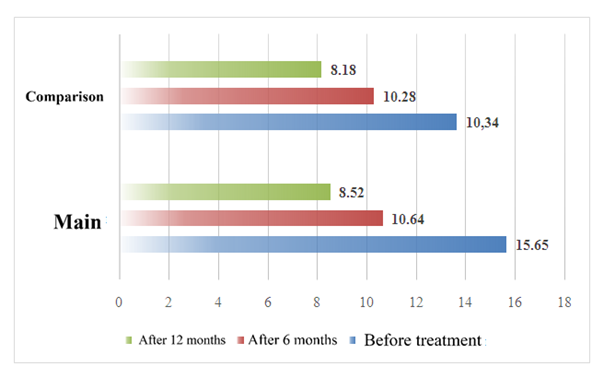
During the study, patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease had an IgA of 1.35±1.04 ng/ml before treatment in the main group of patients. After 6 months of treatment, against the background of antibacterial therapy, group I patients received 1.05±0.05 ng/ml, and against the background of treatment with propolis nastoyka, Group II patients received 0.90±0.07 ng/ml, and against the background of complex treatment with antibacterial therapy + propolis tincture, Group III patients received a positive result of 0.71±0.07 ng/ml (p<0.05) (figure 3). In the study, patients with chronic diffuse periodontitis in the comparison group had IgA, (ng/ml) of 1.26±1.02 ng/ml before treatment. 6 months after the treatment, against the background of antibacterial therapy, 0.64±0.07 ng/ml in Group I patients and 0.74±0.07 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 0.54±0.07 ng/ml (p<0.05). (Figure 3).12 months after treatment in the main group of patients, against the background of antibacterial therapy, 0.72±0.05 ng/ml in Group I patients, and 0.65±0.07 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group patients in Group III patients was 0.59±0.07 ng/ml (p<0.05) (figure 3). (Table 3).12 months later during the study, the comparison group established IGA in patients with chronic diffuse periodontitis, 0.55±0.07 ng/ml in patients with Group I against the background of antibacterial therapy, 0.50±0.07 ng/ml in patients with Group II against the background of propolis tincture, and 0.45±0.07 ng/ml in patients with Group III against the background of complex treatment with antibacterial therapy + propolis tincture (p<0.05). (Figure 3).In the course of the study, patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease had IgE (ng/ml) of 15.65±7.41 ng/ml before treatment in the main group of patients. 6 months after treatment, against the background of antibacterial therapy, 12.64±1.05 ng/ml in Group I patients and 11.63±1.05 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 10.64±1.05 ng/ml (p<0.05) (figure 4). (Table 4).Table 4. Indicators of post-treatment concentration of IgE (ng/ml) in oral fluid for patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study
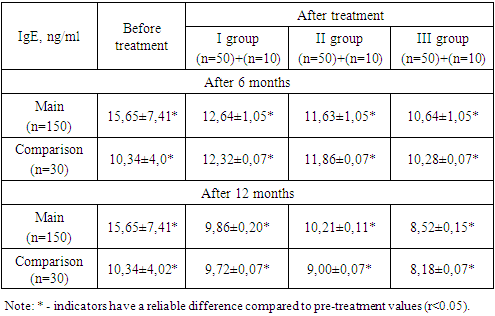 |
| |
|
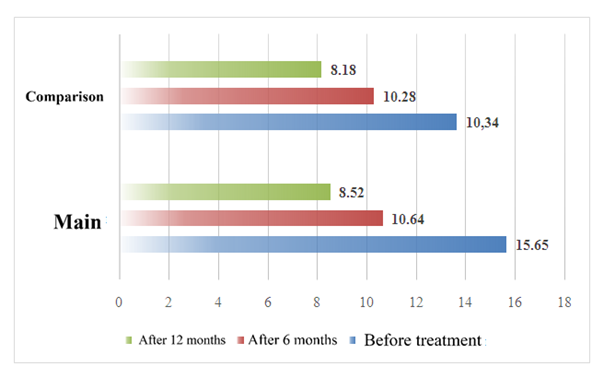 | Figure 4. Results of IgE (g/l) in oral fluid in complex treatment in patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease |
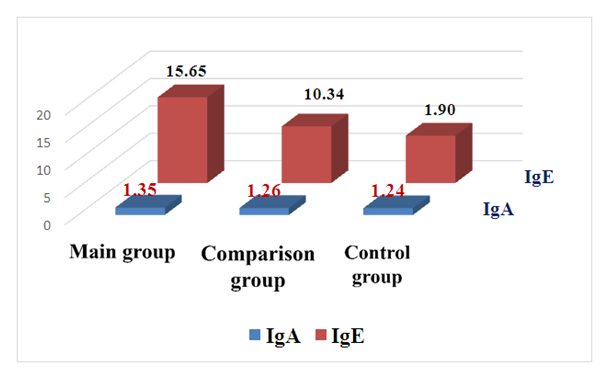
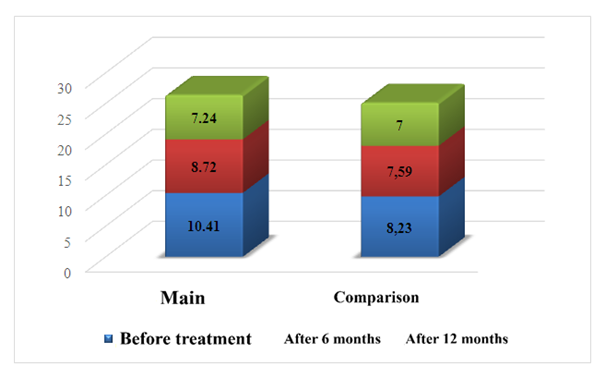
During the study, patients with chronic diffuse periodontitis in the comparison group had an IgE of 10.34±4.02 ng/ml before treatment (ng/ml). 6 months after treatment, against the background of antibacterial therapy, 12.32±0.07 ng/ml in Group I patients and 11.86±0.07 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 10.28±0.07 ng/ml (p<0.05). (Figure 4).12 months after treatment in the main group of patients, against the background of antibacterial therapy, 9.86±0.20 ng/ml in the group I patients, and 10.21±0.11 ng/ml in the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group patients in Group III patients was 8.52±0.15 ng/ml (p<0.05) (figure 4) (table 4).12 months later during the study, IgE in patients with chronic diffuse periodontitis in the comparison group, 9.72±0.07 ng/ml in patients of Group I against the background of antibacterial therapy, 9.00±0.07 ng/ml in patients of Group II against the background of treatment with propolis tincture, and 8.18±0.07 ng/ml in patients of Group III against the background of complex treatment with antibacterial therapy + propolis tincture (p<0.05 (figure 4). We found it necessary to identify anti-inflammatory nterleykin-4 (IL-4) and one of the cytokines that apply inflammation, interleykin-8 (IL-8), even after treatment.The results obtained showed that IL-4 and IL-8 were within the generally accepted norm indicators in observational group patients (table 5), showing a result close to one in practical terms even after treatment - 7.24±0.15 ng/ml and 60.24±0.15 ng/ml (figure 5), respectively, according to the parameters studied.In the course of the study, patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease had IL-4, (ng/ml) of 10.41±2.52 ng/ml before treatment in the main group of patients. 6 months after the treatment, against the background of antibacterial therapy, 9.98±1.05 ng/ml in Group I patients and 9.79±1.05 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 8.72±1.05 ng/ml (p<0.05) (figure 5). 12 months after treatment, against the background of antibacterial therapy, 8.27±0.20 ng/ml in Group I patients and 8.34±0.11 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 7.24±0.15 ng/ml (p<0.05). (Figure 5).In the study, patients with chronic diffuse periodontitis in the comparison group had an IL-4, (ng/ml) pre-treatment of 8.23±1.48 ng/ml. The comparison was 8.02±0.07 ng/ml in Group I patients 6 months after treatment in Group patients against the background of antibacterial therapy, 8.08±0.07 ng/ml in Group II patients against the background of treatment with propolis tincture, and 7.59±0.07 ng/ml in Group III patients against the background of complex treatment with antibacterial therapy + propolis tincture (p<0.05) (figure 5). (Table 5).Table 5. Indicators of post-treatment concentration of IL-4 (ng/ml) in oral fluid for patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study
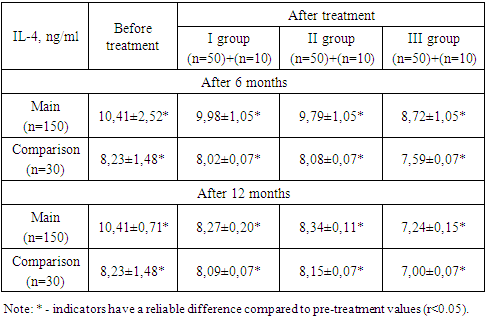 |
| |
|
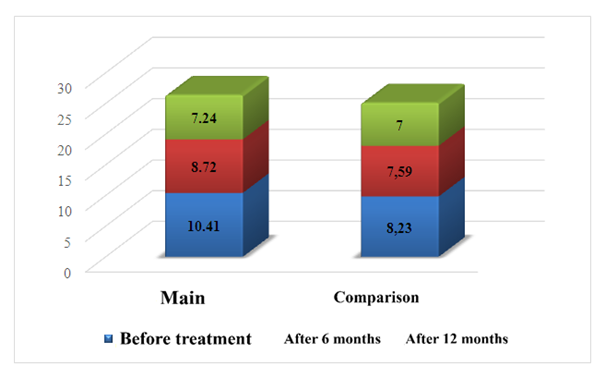 | Figure 5. IL-4 (ng/ml) results in oral fluid against the background of complex treatment in patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease |
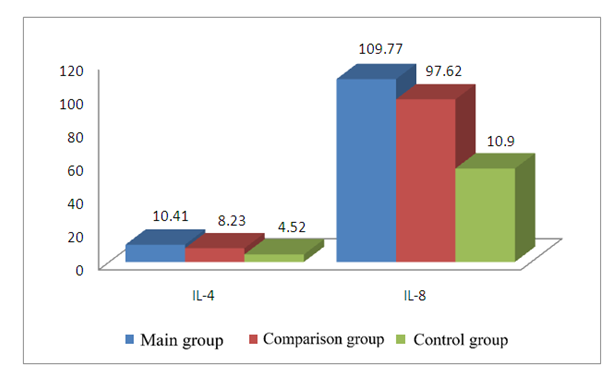
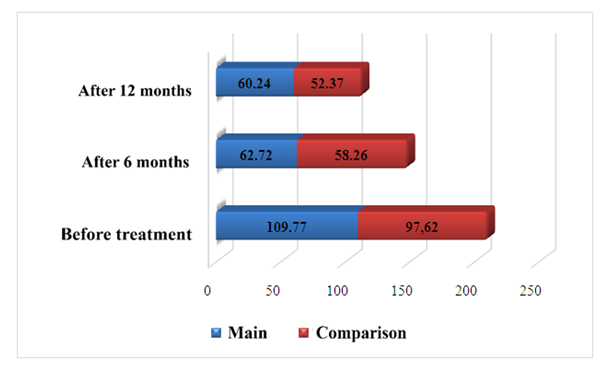
12 months later, in patients with chronic diffuse periodontitis in the comparison group during the study, IL-4, (ng/ml), in patients with Group I against the background of antibacterial therapy, 8.23±1.48 ng/ml, and in patients with Group II against the background of treatment with propolis tincture, 8.09±0.07 ng/ml, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 7.00±0.07 ng/ml (p<0.05). In the course of the study, patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease had IL-8 (ng/ml) at 109.77±6.77 ng/ml before treatment in the main group of patients. 6 months after treatment, against the background of antibacterial therapy, 75.02±3.05 ng/ml in Group I patients and 99.02±3.05 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group III patients was 62.72±1.05 ng/ml (p<0.05) (figure 6).Table 6. Indicators of post-treatment concentration of IL-8 (ng/ml) in oral fluid for patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease in the study
 |
| |
|
 | Figure 6. Results of IL-8 (ng/ml) in oral fluid against the background of complex treatment in patients with chronic diffuse periodontitis against the background of gastrointestinal ulcer disease |
In the study, patients with chronic diffuse periodontitis in the comparison group had a pre-treatment IL-8 (ng/ml) of 97.62±6.51 ng/ml.6 months after treatment, against the background of antibacterial therapy, group I patients received 70.32±0.07 ng/ml, and against the background of treatment with propolis nastoyka, Group II patients received 90.86±0.07 ng/ml, and against the background of complex treatment with antibacterial therapy + propolis tincture, Group III patients received a positive result of 58.26±0.07 ng/ml (p<0.05). 12 months after treatment in the main group of patients, against the background of antibacterial therapy, 68.27±0.20 ng/ml in Group I patients, and 75.3±0.11 ng/ml in Group II patients against the background of treatment with propolis tincture, and against the background of complex treatment with antibacterial therapy + propolis tincture, the positive result in Group patients in Group III patients was 60.24±0.15 ng/ml (p<0.05) (figure 6). After 12 months, the study found IL-8 (ng/ml) in patients with chronic diffuse periodontitis in the comparison group, 66.35±0.20 ng/ml in patients with Group I against the background of antibacterial therapy, and 71.46±0.11 ng/ml in patients with Group II against the background of propolis tincture, and 52.37±0.15 ng/ml in patients with Group III against the background of complex treatment with antibacterial therapy + propolis tincture (p<0.05). Results analysis shows that the comparison shows that complex treatment is effective even after 12 months in Group patients, and the results show a convincing decrease (figure 6).
5. Conclusions
In conclusion, it can be said that during our study, when chronic diffuse periodontitis was observed against the background of gastrointestinal ulcers, patients of both groups experienced a significant decrease in the amount of Ig A and Ig E when a complex treatment was carried out. Also, when chronic diffuse periodontitis of inflammatory applicators and anti-cytokines occurs against the background of gastrointestinal ulcers, the concentration of patients in the oral fluid changes in accordance with the course of the inflammatory process taking place in the body, if the concentration of one of them outweighs the other, this result indicates the course of the inflammatory process. There was a significant decrease in anti-inflammatory IL-4s and inflammatory-calling IL-8s when complex treatment was carried out in both groups.
References
| [1] | Shadieva Sh.Sh. The role of immune mechanisms in patients with inflammatory periodontal pathology // Tibbiyotda yangi kun - Bukhara - 2020 No. 4 (32) - 314-322. (14.00.00. No. 22). |
| [2] | Shadieva Sh.Sh., Abdurakhmanov M.M. The role of Helicobacter pylori infection in the development of functional dyspepsia and inflammatory periodontal diseases // Dentistry - Tashkent -2021 No. 2 (83) - 76-80 pp. (14.00.00. No. 12). |
| [3] | Shadieva Sh.Sh., Giyazova M.M. Combined pathology: periodontal and gastroduodenal diseases // Dentistry - Tashkent -2021 No. 2 (83) - 80-83 pp. (14.00.00. No. 12). |
| [4] | Shadieva Sh.Sh., Habibova N.N. Dynamics of oral microflora in patients with inflammatory diseases of chronic generalized periodontitis and functional dyspepsia // Tibbiyotda yangi kun - Bukhoro - 2022 No. 10 (48) - 9-14 betlar (14.00.00. No. 22) Shadieva Sh.Sh. Dental problems of gastroenterological patients // Cardiorespiratory research Special Issue 1.1 (2021) ISSN: 2181-0974. - P. 103. |
| [5] | Shadieva Sh.Sh. Dental problems of gastroenterological patients and possible ways to solve them // “Current issues in pharmacology from development before their rational application.” Bukhoro. Collection of abstracts May 6-7, 2021 Page 93 – 95. |
| [6] | Shadieva Sh.Sh. State of local immunity of the oral cavity in persons with diseases of the mucous membrane and contamination of the stomach with Helicobacter pylori // International Conference on Science and Education. France 132-133 p. |
| [7] | Radjabova A.F. Basic types of digestion, basic functions of the digestive system // International bulletin of medical sciences and clinical research // - 2023 -Volume 3 / ISSUE 5, May. ISSN: 2750-3399 / R. 67-71. |
| [8] | Radjabova A.F. Digestion in the duodum 12 // Texas Journal of Medical Science. // – Date of Publication: 06-05-2023 / Volume 20/ISSN NO: 2770-2936. P. 67-69. |
| [9] | Radjabova A. F. Features of the dental status of patients with inflammatory bowel diseases // Eurasian Journal of Medical and Natural Sciences // 2022 // Volume 2 // Issue 11, October // ISSN 2181-287X // P. 293 – 298. |
| [10] | Radzhabova A. F. Acute intestinal infections of viral and bacterial etiology. // Web of Scientis: International Scientific Research Jornal // ISSN: 2776-0979 / Volume 3 / Issue 10 / Oct., 2022. P. 881-887. Giyazova Malika Mukhamadovna. Etiopathogenetic aspects and features of damage to the structures of the oral cavity in coronavirus infection //Web of Scientist: International Scientefic Research Journal. -2022. -Vol. 3. - No. 11.- pp. 943-953. |
| [11] | Giyazova M. M. Effectiveness in the Treatment of Changes in the Oral Mucosa of a Patient with Coronavirus // Middle European Scientific Bulletin Academic Journal. – 2022. - T. 28. - P. 55-59. |
| [12] | Giyazova M. M., Sanoeva M. Zh. Neurostomatological features of damage to oral cavity structures during coronavirus infection // Conferences. – 2022. – P. 98-110. |
| [13] | Giyazova M. M. Modern Treatment of Diseases of the Oral Mucosa and Periodontal Under the Influence of Covid 19 // International Journal on Integrated Education. – 2021. – T. 4. – No. 10. – pp. 96-97. |
| [14] | Giyazova M. M. Specificity of the Course and Improvement of Treatment of Diseases of the Oral Mucosa and Periodontal Cavity under the Influence of Covid 19 // "online-conferences" platform. – 2021. – pp. 116-117. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML