-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 786-789
doi:10.5923/j.ajmms.20241403.52
Received: Mar. 4, 2024; Accepted: Mar. 15, 2024; Published: Mar. 29, 2024

Role of Laparoscopy in the Treatment of Liver Echinococcosis Complicated with Peritonitis in Children
Salimov Sh. T. 1, 2, Abdusamatov B. Z. 1, 2, 3, Elmuradov Sh. Kh. 1, 2, Ergashev M. R. 1, 2, Usmanov Kh. S. 1, 2, 3
1Tashkent Medical Academy, Uzbekistan
2Republican Scientific and Practical Center for Minimally Invasive and Endoscopic Surgery of Children, Uzbekistan
3Tashkent Dental Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The goal is to select opportunities to expand the indications for laparoscopic liver echinococcectomy in children and improve the results of surgical treatment of complicated liver echinococcosis in children. Results. From 2009 to 2023, we performed laparoscopic echinococcectomy for hydatid liver disease complicated by peritonitis in 16 patients. Analysis of the results of examination of patients who underwent laparoscopic echinococcectomy of the liver, complicated by peritonitis, which showed a more favorable course of the postoperative period due to the minimal invasiveness of laparoscopic surgery, pain was relieved earlier, intestinal motility was restored more quickly, leukocytosis was early normalized and neutrophilia decreased to normal levels in peripheral blood tests. All this made it possible to reduce the length of hospital treatment. Conclusion. Thus, when performing laparoscopic echinococcectomy complicated by peritonitis, a more favorable course of the postoperative period is promoted.
Keywords: Echinococcosis, Children, Peritonitis, Echinococcectomy, Endoscopy
Cite this paper: Salimov Sh. T. , Abdusamatov B. Z. , Elmuradov Sh. Kh. , Ergashev M. R. , Usmanov Kh. S. , Role of Laparoscopy in the Treatment of Liver Echinococcosis Complicated with Peritonitis in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 786-789. doi: 10.5923/j.ajmms.20241403.52.
Article Outline
1. Introduction
- Hydatid echinococcosis of the liver is a widespread parasitic disease in humans, which is much more severe in childhood than in adults [1]. During the course of the disease, the development of various complications is possible, among which an important place is occupied by rupture of the wall of the liver cyst with the development of peritonitis and anaphylactic shock, which determine the severity of the patients’ condition [2,3]. The developed serious complication requires adherence to rational treatment tactics aimed at preparation, gentle surgical treatment, postoperative management and prevention of disease relapse [4,5].The primary objective of this study is to explore and recommend strategies aimed at broadening the scope of indications for laparoscopic liver echinococcectomy in pediatric patients. Furthermore, the research seeks to enhance the efficacy and overall outcomes of surgical interventions for complex cases of liver echinococcosis in children through the implementation of innovative approaches and refined surgical techniques. By identifying and implementing these advancements, the study aims to contribute significantly to the improvement of treatment outcomes and the overall quality of care provided to pediatric patients with complicated liver echinococcosis.
2. Material and Research Methods
- From 2009 to 2023, we performed laparoscopic echinococcectomy for complicated peritonitis of hydatid liver disease (ELD) in 16 patients at the Republican Scientific Center for Medical and Epidemiology. 13 (81.2%) boys and 3 (18.8%) girls aged 6 to 18 years. The time of admission of patients was 6.5 ± 3.5 hours after the appearance of the first clinical symptoms of peritonitis. In 10 (62.5%) patients, the development of peritonitis was preceded by trauma, after which abdominal pain and repeated vomiting were noted. The clinic was characterized by signs of anaphylactic reaction and peritonitis. During the clinical examination, in addition to the serious condition and characteristic peritoneal symptoms, attention was drawn to the appearance of urticaria in the form of a polymorphic rash on the face, trunk and limbs. Blood tests revealed neutrophilic leukocytosis within 17.6 ± 0.6 109/l, eosinophilia up to 9.2 ± 0.8%. Ultrasound made it possible not only to detect free fluid in the abdominal cavity, but also to establish the cause of peritonitis - the presence of cystic formations in the liver. Preoperative preparation was aimed at correcting disturbances in homeostasis and included detoxification, desensitization and anti-shock therapy.Surgical treatment in all cases began with diagnostic laparoscopy. After the installation of laparoscopic optics, an inspection of the abdominal cavity was performed, the extent of the process was determined, and intraoperative tactics were outlined. At the diagnostic stage, a cloudy effusion was visualized in the abdominal cavity, with perforation of the cyst with fragments of the chitinous membrane (Fig. 1-2). After the introduction of an additional trocar, an inspection of the abdominal cavity was performed, the cause and extent of the process were determined. The accumulated effusion and fragments of the chitinous membrane were evacuated with an electric suction, and the abdominal cavity was sanitized with antiseptic solutions (ozonated water, decosan) to “clean waters.”
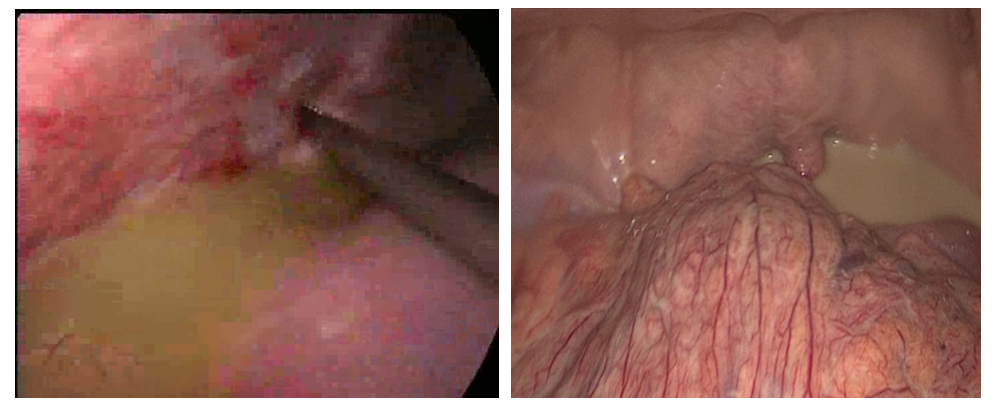 | Figure 1-2. Visualization of free fluid (pus) in the abdominal cavity during perforation of a liver cyst |
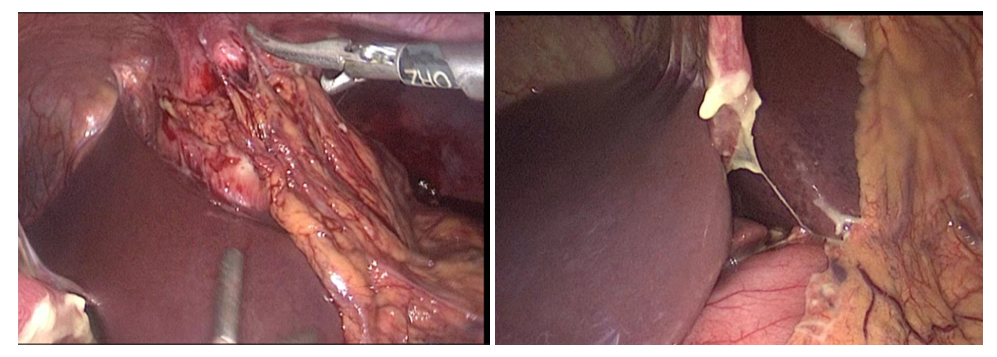 | Figure 3-4. Multiple adhesions between the Glissonian capsule and the diaphragm, as well as between the fibrous membrane of the cyst and the greater omentum |
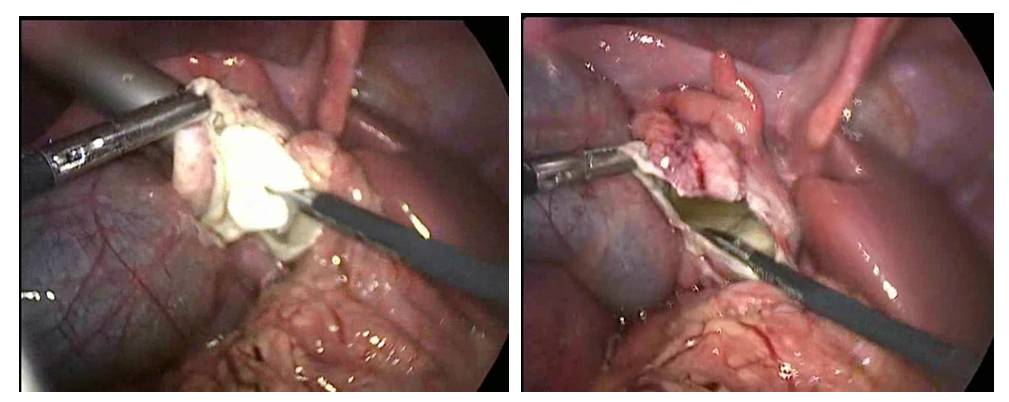 | Figure 5-6. Dissection of the fibrous membrane of the cyst, aspiration and antiparasitic treatment of the inner surface of the cyst |
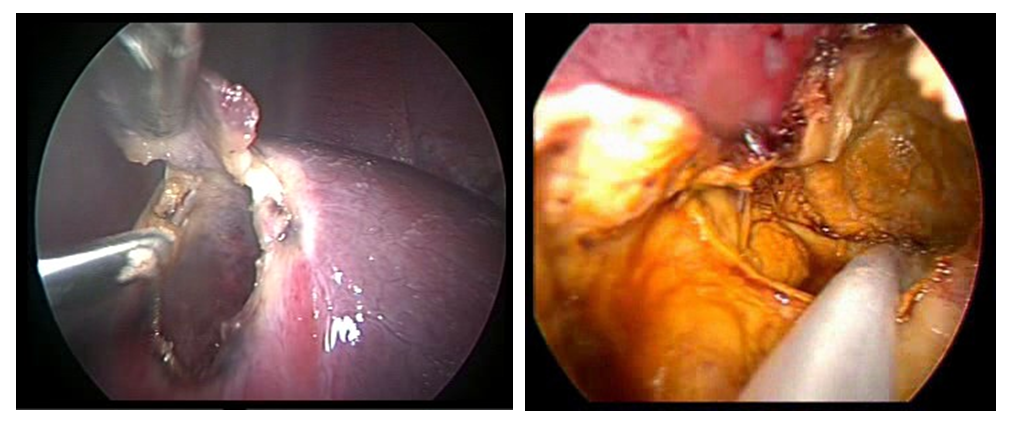 | Figure 7-8. Antiparasitic treatment and drainage of the residual cyst cavity |
3. Results and Discussion
- When analyzing the results of examination of patients who underwent laparoscopic echinococcectomy, sanitation, and drainage of the abdominal cavity for liver cysts complicated by peritonitis, a more favorable course of the postoperative period was noted. Body temperature returned to normal at 2.5±0.15 days. As a result of the minimal invasiveness of laparoscopic surgery, pain was relieved in patients earlier (1.8±0.2 days), and intestinal motility was restored faster (by 1.7±0.16 days). Analysis of the motor activity of patients in the postoperative period showed that earlier activation of patients, at 3.5±0.17 days, occurred after endovideosurgical intervention. A decrease in leukocytosis and a decrease in neutrophilia to normal levels in peripheral blood tests of patients after laparoscopic surgery occurred on days 2.5±0.2. The drains were removed on 3.6±0.2 days (due to the cessation of discharge), the duration of their treatment in the hospital was 14.5±0.2 days. The obtained treatment results allow us to recommend endovideosurgical intervention as the method of choice in the treatment of patients with liver echinococcosis complicated by peritonitis.
4. Conclusions
- Thus, the implementation of minimally invasive techniques, such as laparoscopic echinococcectomy, which aim to reduce trauma to surrounding tissues and organs, coupled with ensuring an optimal extent of surgical intervention tailored to the specific needs of the patient, and the meticulous sanitation of the abdominal cavity to address liver echinococcosis complicated by peritonitis, collectively play a pivotal role in enhancing the overall postoperative recovery trajectory. This approach is observed to yield superior outcomes and a more favorable clinical course in comparison to traditional surgical modalities, underscoring the importance of precision, minimization of trauma, and thoroughness in the management of such complex cases.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML