-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 771-777
doi:10.5923/j.ajmms.20241403.49
Received: Feb. 29, 2024; Accepted: Mar. 15, 2024; Published: Mar. 29, 2024

The Effect of Various Treatments on the Clinical Condition of Patients with Chronic Heart Failure
Abdigaffar G. Gadaev1, Guzel B. Shamsutdinova2, Nilufar A. Gadaeva1
1Tashkent Medical Academy, Uzbekistan
2Fergana Public Health Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In predicting the course of chronic heart failure, the effect of treatment on indicators such as the number of visits to the family polyclinic, the number of emergency medical services, the number of hospitalizations, and the reduction of death are important. The article examines the impact of various medical treatments on the clinical condition of patients and indicators of quality of life. Quality of life was assessed using the Kansas Questionnaire. The results showed a reliable positive change in the number of family clinic visits, emergency calls, and hospital admissions in patients receiving sacubitril+valsartan and dapagliflozin. It was also found that the quality of life was significantly improved in this group of patients.
Keywords: Chronic heart failure, Succubitril+valsartan, Dapagliflozin, Kansas survey
Cite this paper: Abdigaffar G. Gadaev, Guzel B. Shamsutdinova, Nilufar A. Gadaeva, The Effect of Various Treatments on the Clinical Condition of Patients with Chronic Heart Failure, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 771-777. doi: 10.5923/j.ajmms.20241403.49.
Article Outline
1. Introduction
- Chronic heart failure (CHF) is one of the urgent medical and social problems of modern medicine [18,21]. This is due to its prevalence, severe consequences, and high cost of treatment [20,4,12].Mortality due to CHF is 4-8 times higher than in the general population, and half of patients die within 5 years of diagnosis. Its IV functional class (FS) has a half-year mortality rate of 44% [1,11,17].According to epidemiological data, in the Russian Federation and European countries, in most cases, CHF develops as a result of arterial hypertension (95%) and ischemic heart disease (IHD) (69.7%). In our republic, the main cause of this serious complication is often the two diseases listed above [2]. Due to the increase in the life expectancy of the population, the positive results achieved in the treatment of cardiovascular diseases and the prevalence of the risk factors that cause the main diseases that cause CHF, IHD and hypertension diseases (HD), this serious complication is more and more common among the world’s population [3,6]. Despite the progress made in recent years, CHF confirms that health remains a heavy financial burden on the economy of all countries around the world.Systemic changes are observed in all organs of CHF, and remodeling processes in the heart are of particular importance [9]. It is known that a number of examination methods are used in the diagnosis and evaluation of the effectiveness of treatment of CHF. Among them, natriuretic hormones are of particular importance as a biological marker. Currently, there are a number of its representatives, among which brain and N-pro brain sodium uretic peptides are widely used in the diagnosis and assessment of CHF.According to P. Bettencont and co-authors, N-pro brain sodium uretic peptide can be used to predict the course of the disease in CHF. The increase of this marker in the blood of patients with CHF is a clear sign of decompensation. It is also noted that the number of deaths and hospitalizations is high in patients with high levels [5].A.M. Richards was one of the first to use the concentration of N-prosodium uretic peptide in the blood to control the effect of treatment in patients with CHF. It observed titration of the dose of angiotensin-converting enzyme inhibitors (ACEIs) in patients diagnosed with CHF II–III FC under hormonal control and demonstrated the appropriateness of such an approach [19].In the IMPRESS trial, which included 573 patients receiving lisinopril and omapatrilat, those with CHF and left ventricular ejection fraction less than 40% had reliable reductions in neurohormone 1-2 years after initiation of treatment in a randomized trial [7].It is known that a reliable measure of the effectiveness of CHF treatment is the number of visits to the doctor, the number of hospitalizations, and the decrease in mortality [16,13]. It has been suggested that this process is under the control of N pro brain sodium uretic hormone.In recent years, studies have shown that GNKT2i dapagliflozin has a positive effect on the quality of life of patients with CHF. They provide information on the positive effect of dapagliflozin on the stability of the clinical condition of this group of patients, the number of re-hospitalizations and their duration [14,8].The effect of different combinations of recommended standard drugs for CHF on indicators such as predicting the course of CHF and detecting them in the early stages under the control of the above-mentioned markers, as well as on indicators such as referrals to family polyclinics, calls for emergency medical care, number of hospitalizations, and mortality have not been studied. Taking this into account, we set the following goals and tasks.
2. The Purpose of the Study
- Studying the effect of various treatments in chronic heart failure on the number of visits to the family polyclinic, the number of emergency medical calls and hospitalizations, as well as their quality of life.
3. Research Materials and Methods
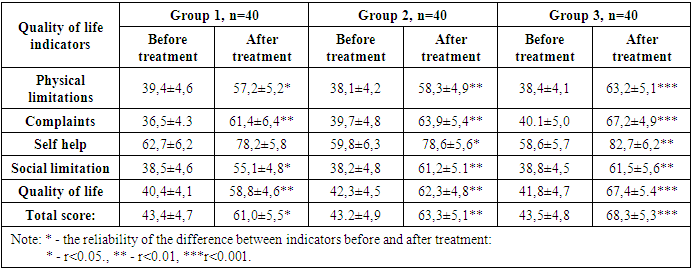
- This scientific research work was conducted in 2022 and 2023 in Fergana Public Health Medical Institute and private clinic “Farovon” in 120 patients with developed CHF on the basis of IHD and arterial hypertension (AH). They, in turn, were divided into three groups based on the treatment procedures. Each group consisted of 40 patients, 20 of which consisted of CHF II and III FC. The average age of the first group of patients was 66.1±1.8, men were 21 (52.5%) and women were 19 (47.5%). In the 1st group of patients under observation, the number of those who underwent myocardial infarction (MI) - 28 (70%), those who underwent aortic coronary bypass surgery (CBS) or stenting - 11 (27.5%), rhythm disorders and blockades were recorded - 12 (30%), AH there were 31 (77.5%), those with different degrees of obesity - 17 (42.5%), those with anemia - 21 (52.5%). This group was prescribed β-blockers + AAFIs or angiotensin receptor blockers (ARBs) + mineralocorticoid receptor antagonists (MRKA)-veroshpirone as the standard treatment for CHF. The average age of the second group of patients was 65.9±1.5, men were 24 (60%) and women were 16 (40%). In this group, the number of those who underwent MI - 25 (62.5%), those who underwent ACS or stenting - 13 (32.5%), those who had rhythm disorders and blockades - 15 (37.5%), those who had AD 27 (67.5%), those who were obese in various degrees - 16 (40%), anemia was observed - 19 (47.5%) people. They received a standard treatment consisting of β-blockers + succubitril-valsartan (yuperio) + MRKA-veroshpirone. The average age of the third group of patients was 64.7±1.3, 21 (52.5%) of them were men and 19 (47.5%) were women. In this group, the number of those who underwent MI - 27 (67.5%), those who underwent aortic coronary bypass surgery or stenting - 16 (40%), those who had rhythm disorders and blockades - 17 (42.5%), those who had AH 25 (62.5%), of various degrees 15 (37.5%) were diagnosed with obesity, 19 (47.5%) were anemic. β-blockers + succubitril-valsartan (yuperio) + MRKA-veroshpiron + glucose-sodium co-transporter type 2 inhibitors (dapagliflozin/forsiga) were recommended to these patients.Particular attention was paid to the same number of patients in II and III FC in each group and their representativeness.The effect on the number of patients’ referrals to the family polyclinic, calls to emergency medical services, and hospital admissions was studied before and 6 months after the start of the treatment in all subjects included in the study. Their quality of life indicators were assessed using the Kansas Questionnaire.The Kansas questionnaire recommended by Green C.P. and Porter C.B. in 2000 was used to assess patients' quality of life [10]. The patient fills out this questionnaire based on his general condition during the last month.Analysis and discussion of research results. We studied the clinical status of the patients involved in our study, including the number of visits to the polyclinic, the number of emergency medical calls, the number of re-hospitalizations, and the observed mortality after various treatment procedures. Table 1 below presents the results obtained during a careful prospective follow-up.
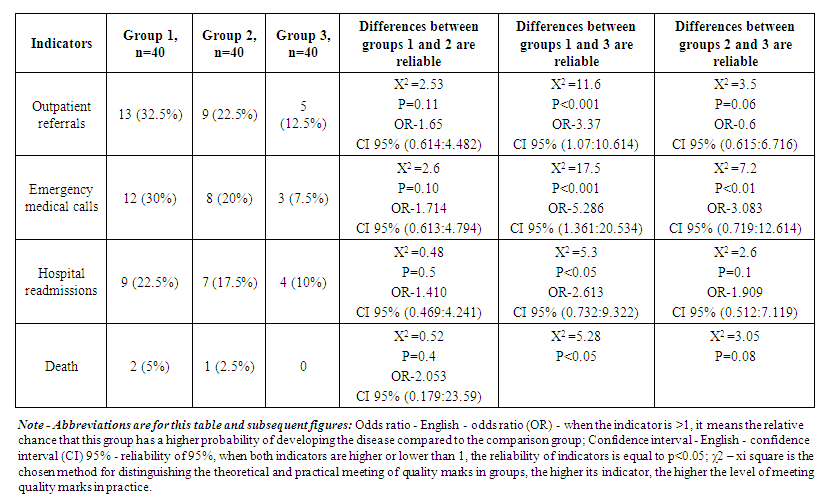 | Table 1. The effect of various treatments on the clinical condition of patients with chronic heart failure |
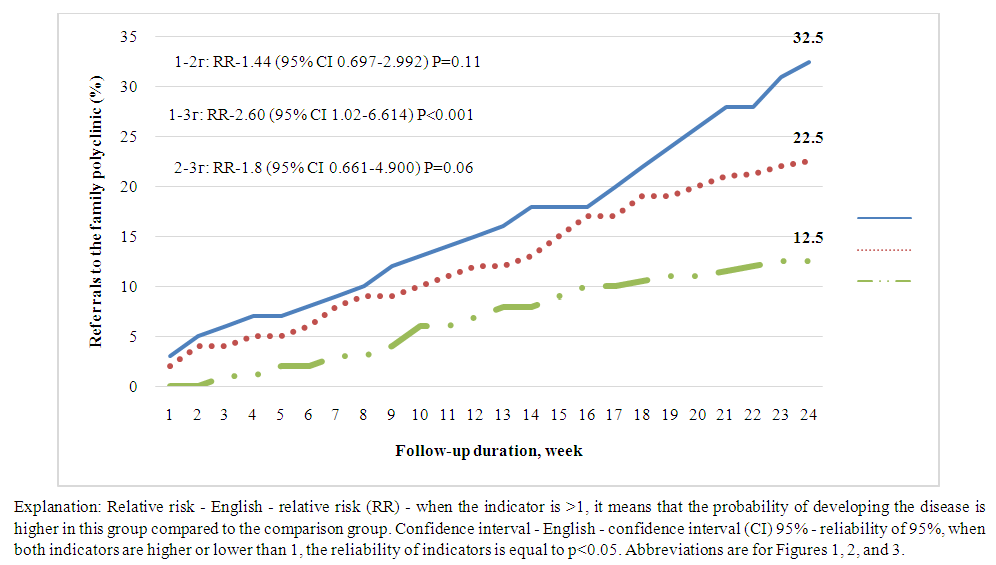 | Figure 1. The number of referrals to family polyclinics of all groups of patients during follow-up |
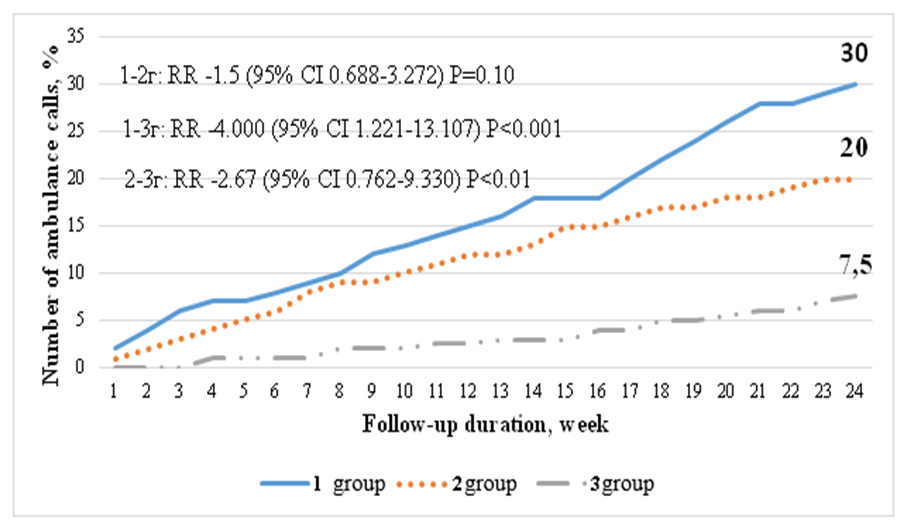 | Figure 2. The number of emergency medical calls during the follow-up of patients of all groups |
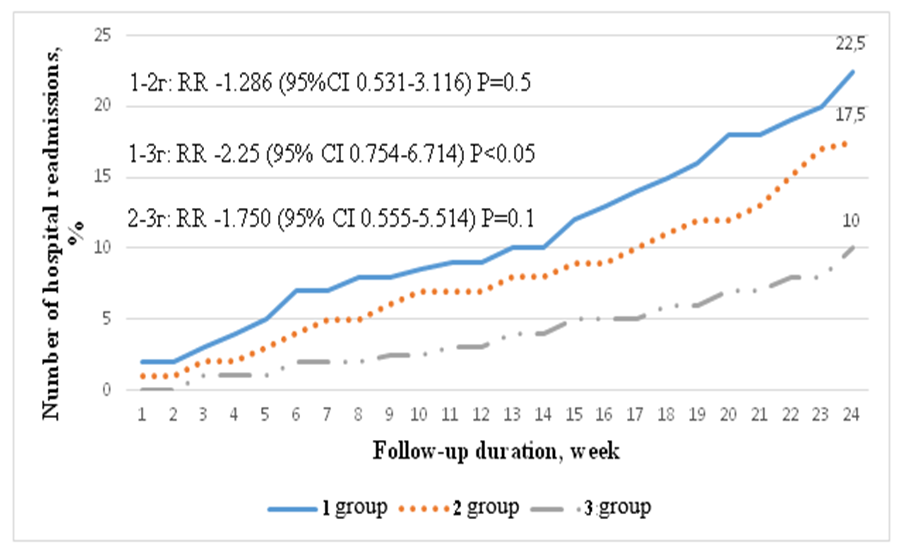 | Figure 3. The number of hospital readmissions of all group patients during follow-up |
|
4. Conclusions
- Based on our analysis, we can come to the following conclusions: 1. When complex treatment is prescribed to patients with chronic heart failure, the number of visits to the polyclinic, the need for emergency medical care, and the number of hospitalizations are reliably reduced;2. Standard complex treatment of patients with chronic heart failure has a reliable positive effect on the quality of life of patients. Determining it using the Kansas questionnaire ensures the objectivity of the obtained results.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML