-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 755-759
doi:10.5923/j.ajmms.20241403.46
Received: Feb. 29, 2024; Accepted: Mar. 18, 2024; Published: Mar. 29, 2024

Analysis of Characteristics of Immunological Changes in Patients with Vitiligo
Ikhtiyor Ikromovich Latipov
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Ikhtiyor Ikromovich Latipov, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To date, a growing body of evidence strongly suggests that disorders of the immune system are intricately linked to the pathogenesis of vitiligo, a condition marked by the progressive loss of skin pigmentation. The prevailing scientific consensus is that vitiligo is not merely a cosmetic anomaly but a complex autoimmune disorder. This perspective is supported by numerous studies indicating significant anomalies in both cellular and humoral aspects of the immune response in individuals afflicted with this condition. Researchers around the globe have reported alterations in immune markers, signaling a profound disruption in the normal functioning of the body's defense mechanisms in patients with vitiligo. Current investigations into the immunological underpinnings of vitiligo reveal that the disease is associated with a variety of immune system irregularities. Notably, there is an observed increase in the activity of cytotoxic T cells and natural killer cells, which are implicated in the direct destruction of melanocytes, the pigment-producing cells whose loss results in the characteristic white patches of vitiligo. Additionally, abnormalities in the regulatory T cell population, which plays a critical role in maintaining immune tolerance, have been noted, suggesting a failure in the mechanisms that normally prevent autoimmune reactions. Parallel to cellular immunity disturbances, alterations in humoral immunity have also been documented. Elevated levels of certain autoantibodies, particularly those targeting melanocyte-specific antigens, have been identified in the serum of vitiligo patients. These autoantibodies can contribute to melanocyte destruction and pigment loss, further supporting the hypothesis that vitiligo has a strong autoimmune component. To elucidate the complex interactions between the immune system and the onset of vitiligo, a comparative study was conducted to assess the immune status of individuals with vitiligo compared to healthy controls. This study aimed to provide a comprehensive overview of the immunological profile of vitiligo patients, including the analysis of various immune cell populations, the presence of specific autoantibodies, and the levels of cytokines and other inflammatory mediators. By doing so, researchers hoped to uncover specific immunological markers that could not only aid in the understanding of vitiligo's pathogenesis but also serve as potential targets for therapeutic intervention. The findings of this comparative study underscore the multifaceted nature of the immune dysregulation associated with vitiligo. It highlighted significant differences in the immune profiles of vitiligo patients, thereby shedding light on the potential pathways through which the immune system contributes to the disease process. These insights pave the way for the development of targeted immunomodulatory therapies aimed at restoring normal immune function and potentially reversing the pigmentary changes characteristic of vitiligo. Overall, the accumulation of evidence pointing to the role of immune system disorders in vitiligo not only enhances our understanding of the disease but also opens new avenues for research and treatment. As the scientific community delves deeper into the immunological aspects of vitiligo, it is hoped that more effective and personalized treatment strategies will emerge, improving the quality of life for those affected by this challenging condition.
Keywords: Vitiligo, Immune system, Autoantibody, Subpopulation, White spots
Cite this paper: Ikhtiyor Ikromovich Latipov, Analysis of Characteristics of Immunological Changes in Patients with Vitiligo, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 755-759. doi: 10.5923/j.ajmms.20241403.46.
1. Introduction
- Vitiligo is a complex, acquired dermatological condition, the exact etiology of which remains elusive, characterized predominantly by progressive depigmentation of the skin. This depigmentation results from the targeted destruction or malfunction of melanocytes—cells responsible for producing melanin, the pigment that gives color to the skin, hair, and eyes—in specific skin regions. Consequently, vitiligo manifests as acquired hypomelanosis, frequently presenting in a symmetrical pattern and is distinguished by the emergence of white patches on the skin. These patches tend to expand progressively as a result of ongoing dysfunction in the epidermal melanocytes, which also extends to the melanocytes situated in the hair follicles, leading to the possible depigmentation of hair in the affected areas.Globally, the prevalence of vitiligo is notable, with the World Health Organization (WHO) estimating that over 2% of the world's population is affected by the condition. This prevalence is reported to be even higher, between 3-4%, in countries and regions located in the southern hemisphere. Particularly striking is the incidence rate of vitiligo in Central Asia, where it can reach up to 10% in certain localities. The development of vitiligo appears to be indiscriminate, affecting individuals regardless of gender, age, or racial background. Notably, a significant proportion of vitiligo cases, approximately two-thirds, commence between the ages of 10 and 25 years. However, the disease is also seen in younger demographics, including children under the age of 10, newborns, and nursing infants, indicating a broad age range of susceptibility.The pathophysiology of vitiligo involves complex interactions between genetic, immunological, and environmental factors, leading to the selective destruction of melanocytes. Despite extensive research, the precise mechanisms triggering melanocyte destruction in vitiligo remain partially understood. Various hypotheses have been proposed, including autoimmune processes, neural mechanisms, and oxidative stress, among others, highlighting the multifactorial nature of this condition.The impact of vitiligo extends beyond the physical manifestations, affecting the psychological well-being and quality of life of individuals due to the visible and often stigmatized nature of the skin changes. The management of vitiligo is multifaceted, aiming not only to halt the progression of depigmentation but also to achieve repigmentation through medical, surgical, and adjunctive treatments. Despite advancements in therapeutic options, vitiligo remains a challenging condition to manage, underscoring the need for ongoing research and innovation in its treatment. Currently, the role of immunological disorders in the pathogenesis of vitiligo is generally recognized. In recent decades, many scientific studies show that the appearance of depigment foci can be the result of immunological reactions and autoimmune diseases, which help to produce autoantibodies both to melanocytes and to the structures that store melanin within them [5]. Changes in the total amount of T-lymphocytes and their subpopulations have been found to contribute to the further production of pathological cytokines [8]. Activation of the sympathetic nervous system (SNS) under the influence of negative factors (stress) can limit (inhibitor) T-cell reactions, antiviral immunological reactivity and NK (Natural killer) cell activity [9]. A recent scientific study reported increased numbers of T-cells recognizing melanocyte antigens in vitiligo-damaged skin compared with non-damaged skin and serum [10], suggesting a CD8+ melanocyte-specific T-cell-mediated immune response. The first step in the destruction of skin melanocytes by such activated cytotoxic cells is the shift in the balance between immune resistance and protection, which depends on the decrease in the number of regulatory T cells.The cell-mediated immune response has been shown to play an important role in both keratinocyte apoptosis and melanocyte apoptosis. CD8+ T-cell infiltration is an important link in the pathogenesis of vitiligo. CD8+ (cytotoxic, T-killer) T-lymphocytes are responsible for the apoptosis of melanocytes and lead to complete destruction of melanocytes in foci of vitiligo. In addition, it has been shown that CD8+ T-lymphocytes can enhance keratinocyte apoptosis in intact skin by enhancing the disruption of the interaction between melanocytes and keratinocytes [7]. The above effects are mediated by cytotoxic T-lymphocytes, which probably produce inflammatory cytokines such as interferon gamma (IFNg) and tumor necrosis factor alpha (TNF-α). These cytokines enhance the process of apoptosis in keratinocytes, which indicates the role of inflammation in the spread and development of vitiligo [3].Since the etiology and pathogenesis of vitiligo have not yet been fully established, the treatment of this dermatosis in dermatology remains one of the unsolved problems. The fact that highly effective and reliable treatment methods have not been developed indicates the need to constantly search for new pathogenetically proven treatment methods.Thus, despite efforts aimed at identifying the pathogenesis of vitiligo, a widespread dermatosis worldwide, and developing many treatment methods, this disease continues to be on the list of poorly studied diseases.
2. Material and Methods
- Between the years 2020 and 2023, an extensive study was undertaken to delve into the clinical and immunological aspects of vitiligo, focusing on 118 patients who were diagnosed with two distinct clinical forms of this dermatological condition. This endeavor was comparative in nature, including a control group consisting of 20 healthy individuals who served as a benchmark for the immunological studies. The aim was to draw significant conclusions regarding the underlying immunological differences and similarities between those affected by vitiligo and the general healthy population.The demographic composition of the study group was meticulously recorded, encompassing both female and male patients, with a total of 66 women and 52 men participating. The age range of these patients was quite broad, extending from 18 to 75 years, with the mean age being calculated at 38.5 years, plus or minus a standard deviation of 6.8 years. This wide age range allowed for a comprehensive analysis of vitiligo across different stages of life, offering insights into how age might influence the presentation and progression of the disease.Clinical and immunological evaluations were conducted in a controlled and structured environment, utilizing the facilities of the department of dermatovenerology and pediatric dermatovenerology at the Bukhara State Medical Institute. This was done in collaboration with the dermatovenerology dispensary in the Bukhara region, ensuring that the study was grounded in robust clinical practices and methodologies.The examination protocol for the patients included a thorough general blood analysis. This analysis was comprehensive, encompassing a count of erythrocytes (red blood cells), platelets, leukocytes (white blood cells), along with measurements of hemoglobin content and the erythrocyte sedimentation rate—a marker often used to detect inflammation in the body. These parameters are critical for evaluating the overall health and immune status of individuals, providing foundational data for the study.Furthermore, the biochemical analysis added another layer of depth to the study. Blood samples were meticulously collected from the cubital vein, located in the anterior fossa of the elbow joint, ensuring that the procedure was conducted at least 10-12 hours after the last meal to avoid any potential confounders related to food intake. The samples were then prepared through centrifugation at 3000 rpm for 20 minutes, separating the blood plasma for analysis. Key biochemical markers analyzed included total cholesterol, low-density lipoprotein cholesterol (LDL-C), glucose, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total protein levels. These markers are indicative of various metabolic and liver functions, offering insights into the systemic health conditions that could influence or be influenced by vitiligo.In addition to these assessments, patients were also screened for several infectious diseases that could potentially affect immune function, including HIV infection, syphilis (Rapid Plasma Reagin test), and viral hepatitis (with markers such as Anti-HCV and HBsAg). This comprehensive screening ensured that any external factors potentially affecting the immune system were accounted for, allowing for a focused examination of the immunological profile specifically associated with vitiligo.The meticulous approach to patient selection, combined with the rigorous clinical and immunological examination protocols, underscores the depth and breadth of this study. By examining a diverse group of patients with vitiligo and comparing their clinical and immunological parameters with those of healthy controls, the study aimed to uncover pivotal insights into the pathogenesis and progression of vitiligo, contributing valuable knowledge to the field of dermatological research.
3. Results
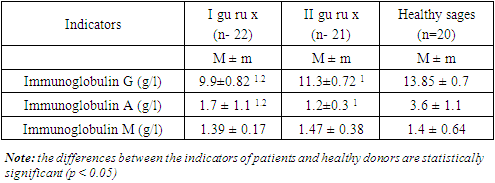
- The indicators of the patients in the examinations before the start of the treatment and after the complex treatment were studied in accordance with the standard generally accepted methods. Determination of the concentration of the three main classes of immunoglobulins in blood serum, immunoglobulin A, M and G, was carried out by the traditional radial immunodiffusion method according to Mancini. The composition of immunoglobulins A, M, G (IgG, IgM, IgA) in blood serum was studied to study the humoral immune status in vitiligo patients. A total of 118 patients in both groups (group I n=60 and group II n=58) serum levels of immunoglobulins A, M, G were determined in 43 patients (22 patients with vitiligo in the first main group and 21 patients in the second comparison group).Table 1 shows the average values of the concentration of immunoglobulins of different classes in patients with vitiligo depending on the clinical form.
|
4. Discussion
- In the comparative analysis of the Dermatological Health Status Index (DHSI) among patients with vitiligo, it was observed that the DHSI values for both experimental groups were significantly elevated in comparison to those recorded in the control group of healthy individuals. This elevation in DHSI values underscores a direct correlation between the severity of dermatological impairment and the detriment to the quality of life experienced by patients with vitiligo. At the outset of the study, before any therapeutic interventions were initiated, the average DHSI values stood at 10.9 ± 3.7 points for patients in Group I and at 10.6 ± 2.0 points for patients in Group II. These figures highlight the considerable negative impact that vitiligo, as a dermatological condition, imposes on the patients' quality of life, as delineated by the assessment criteria employed in this study. Over the course of the treatment, both patient groups were subject to different therapeutic regimes. Group I patients were treated with a combination of narrow-band UVB therapy at a wavelength of 311 nm, excimer laser therapy at a wavelength of 308 nm, and topical applications of 0.1% tacrolimus ointment. Additionally, these patients received systemic treatments including pentoxifylline and dexamethasone. The comprehensive approach in Group I aimed at not only addressing the visible manifestations of vitiligo but also at mitigating the underlying immunological dysfunctions contributing to the disease's progression. The interim analysis, conducted six months into the treatment, revealed significant improvements in the dermatological quality of life indices for both groups. Notably, Group I exhibited a more substantial reduction in the DHSI values, with the mean value dropping to 4.2±1.2 points—a figure that was significantly lower (p<0.05) than the 6.7±0.6 points recorded for Group II. This differential outcome underscores the efficacy of the combined therapeutic modalities utilized in Group I, suggesting a synergistic effect in ameliorating the quality of life for patients undergoing this regimen. One year following the initiation of treatment, both groups manifested a more pronounced decline in DHSI values, indicating a sustained and progressive improvement in the dermatological quality of life. This long-term improvement further validates the therapeutic strategies employed, highlighting the potential for significant restoration of quality of life in patients with vitiligo through targeted treatment approaches. The findings of this study not only illuminate the profound impact that vitiligo has on affected individuals' quality of life but also demonstrate the potential for therapeutic interventions to mitigate these effects. The significant reductions in DHSI values, particularly in the group receiving a multifaceted treatment approach, pave the way for a more optimistic outlook on managing vitiligo. Such insights are invaluable for clinicians and researchers alike, as they continue to explore and refine treatment modalities for this challenging dermatological condition, with the ultimate goal of enhancing patient well-being and quality of life. The study's findings significantly highlight the impact of an innovative, modified immunocorrective treatment regimen on the quality of life among patients suffering from vitiligo. This regimen, which included a combination of narrow-band 311 nm UVB therapy, 308 nm excimer laser therapy, alongside a comprehensive topical treatment regimen incorporating pentoxifylline, dexamethasone, and a local 0.1% tacrolimus ointment, led to a marked improvement in the Dermatological Health Status Index (DHSI) values for patients within group I. Specifically, the average DHSI value in this group experienced a dramatic reduction to 2.1 ± 0.7 points. This reduction is indicative of a significant enhancement in the patients' dermatological quality of life, underscoring the effectiveness of the treatment protocol.Conversely, in group II, where patients were subjected to a similar yet slightly modified treatment regimen, comprising combined phototherapy using both narrow-band UVB and excimer laser therapies along with topical application of 0.1% tacrolimus ointment, the average DHSI values also showed a significant improvement, decreasing to an average of 3.3 ± 0.4 points. Although this decrease represents a considerable improvement in the patients' quality of life, the difference in the DHSI reduction between groups I and II suggests a superior efficacy of the combined treatment approach utilized in group I, particularly with the addition of systemic agents such as pentoxifylline and dexamethasone.It is critical to note that, despite these improvements, the average DHSI values in both groups remained higher than those observed in the healthy control group. This observation implies that while the treatment regimens significantly ameliorated the quality of life for vitiligo patients, complete normalization to the levels seen in individuals without the condition was not achieved. However, the statistical analysis of the DHSI dynamics, yielding positive values (p<0.05) in comparison to the baseline dermatological quality of life index of the vitiligo patients, confirms the beneficial impact of the treatment protocols.These findings advocate for a multifaceted approach to the management of vitiligo, emphasizing the necessity of incorporating both phototherapy and topical treatments, with the potential addition of systemic treatments to achieve optimal outcomes. The differential improvements observed between the two patient groups further suggest that personalized treatment plans, tailored to the specific needs and responses of individual patients, could be key in maximizing the quality of life improvements for those living with vitiligo.This research not only adds to the growing body of evidence supporting the effectiveness of various combinations of therapeutic interventions in treating vitiligo but also highlights the importance of assessing treatment outcomes through the lens of quality-of-life improvements. As vitiligo continues to be a condition with significant psychological and social implications for those affected, the pursuit of treatment modalities that offer not only clinical but also quality-of-life improvements remains a paramount concern in dermatological research and practice.
5. Conclusions
- The intricate process of vitiligo formation, characterized by the emergence of depigmented white spots on the skin, underscores a complex and poorly understood regulatory mechanism within the body's immune system. These manifestations are the result of unregulated immune responses that attack and destroy melanocytes—the cells responsible for pigment production—leading to the characteristic white patches of vitiligo. This aberrant immunological activity suggests an underlying autoimmune etiology, where the body's immune system mistakenly targets and damages its own cells.Given the autoimmune nature of vitiligo, a multifaceted approach to treatment is necessary. Immunologic investigations play a crucial role in unraveling the specific cellular and molecular pathways involved in the onset and progression of vitiligo. Such studies are essential for identifying the immune cells and factors that contribute to the destruction of melanocytes, thereby offering insights into potential targets for therapeutic intervention.Targeted systemic and topical immunocorrective therapies emerge as promising strategies for managing vitiligo. Systemic treatments aim to modulate the overall immune response, potentially preventing the widespread destruction of melanocytes across the body. Topical therapies, on the other hand, are designed to address localized areas of depigmentation, directly influencing the immune environment within the white spots. These treatments seek to reduce the intensity of the tissue-specific autoimmune response, thereby mitigating the progression of depigmentation and promoting the stabilization or reversal of symptoms.The effectiveness of these interventions hinges on a deep understanding of the individual's immune profile and the specific characteristics of their vitiligo, underscoring the importance of personalized medicine in the treatment of this condition. By tailoring therapies to the unique immunological landscape of each patient, clinicians can optimize outcomes, enhancing the potential for repigmentation and the restoration of normal skin appearance.In conclusion, the formation of depigmented white spots in vitiligo represents a complex challenge, involving dysregulated immune reactions that necessitate comprehensive immunologic investigation and carefully chosen immunocorrective therapy. Through targeted interventions that address both systemic and localized immune responses, it is possible to diminish the autoimmune assault on melanocytes, offering hope for individuals affected by this visually and psychologically impactful disease. This integrated approach not only aims to improve the cosmetic appearance of vitiligo patches but also seeks to enhance the quality of life for those living with the condition, marking a significant step forward in the management of autoimmune dermatological disorders.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML