Halimova E. M., Karimova N. N.
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
LDLR and LP(a) factors were examined in order to determine the relationship between dyslipidemia and TPKS, and to determine whether this condition is related to TMI. For the study, 105 women diagnosed with recurrent polycystic ovary aged 19-35 years, 27 of reproductive age in the control group. healthy women were studied. When the plasma concentration of LDLR was examined, it was found that obese and non-obese patients were 1.42 (p<0.05) and 1.13 (p>0.05) times lower than the control group, respectively. In general, the prognostic performance of the LDLR marker was found to be very good for obese patients and satisfactory for non-obese patients.
Keywords:
Relapsing polycystic syndrome, Obesity, Molecular markers, Lipoprotein-associated phospholipase (A2Lp-PLA2), LOX-1, LDLR, LP(a), Insulin resistance
Cite this paper: Halimova E. M., Karimova N. N., Results of LDLR and LP(a) Molecular Markers in Patients with Polycystic Ovarian Syndrome, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 743-745. doi: 10.5923/j.ajmms.20241403.43.
1. Introduction
Polycystic ovary syndrome (PCOS) is considered one of the main causes of infertility in modern literature, not as an independent disease, but as a phenomenon that combines a number of symptoms and has a common clinical and biochemical appearance [1,2,6]. It is mainly manifested by ovarian hyperandrogenism, and morphological changes in the ovaries are accompanied by chronic anovulation [3,5]. In 60-70% of cases, hyperandrogenism is combined with metabolic syndrome, which aggravates the woman's condition and requires a special approach to restore the female reproductive function and improve the quality of life [10]. In developed countries, the incidence of metabolic syndrome and related complications reaches 20% among women over the age of 30 [7,8,9]. According to various sources, the incidence of TPS in the female population of developed countries reaches 20%, and hyperandrogenism in women with anovulatory infertility. It is the main cause in 75% of cases [10,11,12].
2. The Purpose of the Study
In order to determine the correlation between dyslipidemia and TPKS, and to determine whether this condition is related to TMI in patients, LDLR (low density lipoprotein receptor) and LP(a) factors were examined.
3. Research Materials and Methods
A total of 132 women were examined in prospective examinations in 2020-2022, they were studied in 3 groups. Group 1 was our primary group, consisting of 57 obese women with relapsed TPS. Our group 2 was a comparison group consisting of 48 women with recurrent TPS without obesity. Our 3rd group consisted of 27 gynecologically healthy women. Hormonal tests in all groups of women were determined in serum samples.
4. Results and Discussion
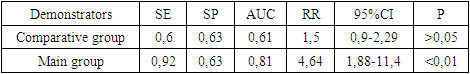
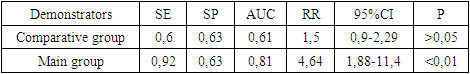
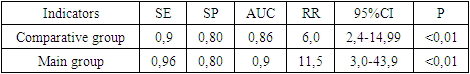
According to the results of various studies, dyslipidemia is one of the characteristic pathophysiological disorders in patients diagnosed with TPKS, and in many patients, it was found that the serum concentration of ZPLP-HC and triacylglycerides increased and the concentration of ZULP-HC decreased.As shown in Figure 1, the concentration of soluble LDLR in blood serum was 246.0 ± 14.46 pg/ml and 195.45 ± 18.4 pg/ml in patients in different comparative and primary TPKS groups, while in the control group, this indicator was 277.5 ± It was equal to 9.38 pg/ml. If patients in the control group were 1.12 times lower than the control group, TPKS was 1.42 (p<0.05) times lower in the group of patients with obesity and 1.26 (p<0.05) times lower than the control group. was preserved. Based on this, the prognostic and pathogenetic significance of the LDLR factor in the development of TPKS in patients with different TMI was investigated (see Table 1).Table 1. The significance of the LDLR factor in predicting TPKS in obesity and independent of it
 |
| |
|
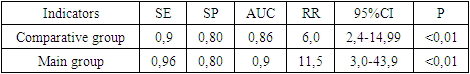
As shown in Table 1, the LDLR factor was found to have a very good prognostic value in different groups of patients, especially obese TPKS patients (AUC=0.81), while this indicator was found to be satisfactory (AUC=0.61) in TPKS patients with normal TMI. Similarly, regarding the relative risk factor, it was found that LDLR factor increased the risk of TPKS observed by obesity by 4.64 times (95%CI: 1.88-11.4), and this indicator was found to be statistically reliable (p<0.01). On the other hand, in TPKS patients without obesity, the relative risk factor was 1.5 (95%CI: 0.9-2.29;), but this indicator was not statistically reliable (p>0.05). Based on the mentioned indicators, it can be concluded that there is a reliable correlation between the LDLR marker and obesity in TPKS patients, but the inducing value of the LDLR marker in the development of TPKS independently of the obesity factor was not determined.Similarly, one of the markers of dyslipidemia - Lp (a), according to the results obtained in different groups, in the main group of obese and non-obese patients, the results were 63±1.21 (p<0.05) mg/dL and 44.81± It was 1.6 (p<0.05) mg/dl, while in the control group it was 18.95±2.4 mg/ml. The obtained results showed that this factor increased by 2.37 (p<0.001) times in the comparative group compared to the control group, while this increase in the blood serum of the main group of patients was 3.33 (p<0.001) compared to the control group, 1.4 (p<0.05) ) was found to have increased several times.Knowing that the amount of Lp(a) was statistically significantly higher in the patient group than in the control group, its pathogenetic significance and prognostic effectiveness in TPKS were calculated (see Table 2). As shown in Table 2, the Lp(a) marker's predictive performance of TPKS was found to be excellent (AUC=0.9) and very good (AUC=0.86) in obese and non-obese TPKS patients, respectively. Thus, it was found that the Lp(a) marker has an independent inducing effect on the TMI factor of patients with pathogenetic significance in the development of TPKS. According to it, the relative risk factor increased by 11.5 (95%CI: 3.0-43.9; p<0.01) times in obese patients, and by 6 (95%CI: 2.4-14) in non-obese patients. .99; p<0.01) times increased. Based on the above results, it can be said that the Lp(a) factor can be considered as a specific marker independently of TMI in the diagnosis of TPKS.Table 2. The significance of Lp(a) factor in predicting TPKS in obesity and independent of it
 |
| |
|
Table 3. Correlation of LDLR and Lp(a) biomarkers with other indicators in patient groups
 |
| |
|
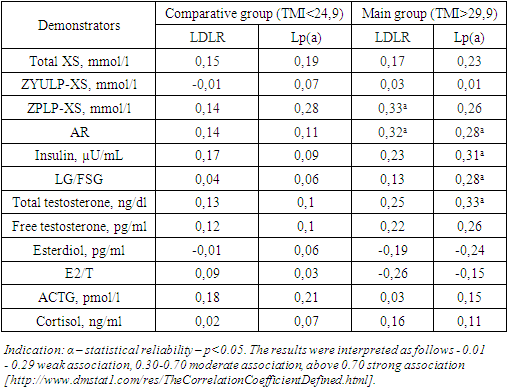
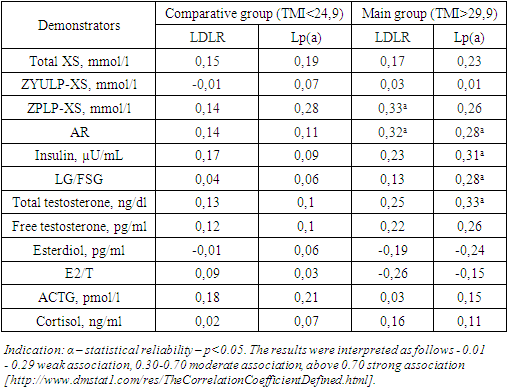
As shown in Table 3, no statistically reliable correlation was found between LDLR and Lp(a) values and other biomarkers in TPKS patients without obesity. On the other hand, in TPKS patients with obesity, there is a moderate positive association between LDLR and ZPLP, AR, Lp(a) and other biomarkers, especially insulin, total testosterone, and AR, LG/FSG ratio. the correct weak link is found to exist. According to the analysis of the results of the mentioned correlation analysis, LDLR and Lp(a) markers were significant only in this group of obese patients.
5. Summary
When the plasma concentration of LDLR was examined, it was found that obese and non-obese patients were 1.42 (p<0.05) and 1.13 (p>0.05) times lower than the control group, respectively. In general, the prognostic performance of the LDLR marker was found to be very good for obese patients and satisfactory for non-obese patients. Thus, according to the result of the relative risk factor, an aberrant decrease in the concentration of the LDLR marker was found to increase the development of TPKS by 4.64 times (p<0.001) in obese patients, and by 1.5 times (p<0.05) in non-obese patients. The mentioned results found that LDLR is important in the development of TPKS only through its syntropic effect with the obesity factor. According to the correlation analysis, in non-obese patients, no statistically reliable relationship was found between LDLR and other tested indicators, on the other hand, in obese patients, there was a statistically significant correlation with ZPLP-XS (r=0.33), AR (r=0.32) indicators. a significant association was found.
References
| [1] | Alieva, F. N. Izuchenie osnovnyx etiopathogeneticheskikh mezhnykhov formirovaniya sindroma polykistoznyx yaichnikov / F. N. Alieva, N. V. Samburova // Young scientific forum: aesthetic and medical science. – 2017. – No. 2(41). - S. 16-25. |
| [2] | Blesmanovich, A. E. Polycystic ovarian syndrome: classic and modern nuances / A. E. Blesmanovich, Yu. A. Petrov, A. G. Alexina // Journal nauchnyx statey Zdorove i obrazovanie v XXI veke. - 2018. - T. 20. – No. 4. – S. 33-37. |
| [3] | Glukhova M. V. Osobennosti klinicheskikh, hormonalnyx i metabolicheskikh narusheniy u bolnyx s syndromem polycystoznyx yichnikov s raznymi tipami ozhireniya i normalnoy massoy tela / M. V. Glukhova, T. V. Draznina, T. V. Karpov [i dr.] // Upravlenie kachestvom meditsinskoy pomoshchi. – 2016. – No. 1-2. - S. 33-37. |
| [4] | Grigoryan, O. R. Syndrome of polycystic ovaries - otdalennye risk / O. R. Grigoryan, E. N. Andreeva // Effektivnaya pharmacoterapiya. – 2015. – No. 5. – S. 20-25. |
| [5] | Nayimova N.S., Karimova N.N. Specificity of changes in hormones and enzymes in premature ovarian failure // New day in medicine. - Tashkent, 2023. - #8(58). - S. 52-56. |
| [6] | Nayimova N.S., Karimova N.N. Innovatsionnye biokhimicheskie markyory reproduktivenogo zapasa u genshchin s predevremennoy dosstatochnostyu yaichnikov // A new day in medicine. - Tashkent, 2023. - #3(53). - S. 170-175. |
| [7] | Nayimova N.S., Karimova N.N. Osobennosti ultazvukovykh izmeneniy u genshchin s predevremennoy dostatochnostyu yaichnikov // Novosti dermatovenerologii i reprodutivnogo zdorovya. - Tashkent, 2023. - #1(101). - S. 28-30. |
| [8] | Nayimova N.S. Osobennosti vzaimosvyazi biokhimichesikh izmeneniy u genshchin c prejdevremennoy dosstatochnostyu yaichnikov s indexom massy tela i drugi zabolevaniyami // Jurnal teoreticheskoi i klinicheskoi meditsiny. - Tashkent, 2023. -#2. - S. 154-157. |
| [9] | Karimova N.N., Naimova N.S., Khalimova E.M., Karimov D.N. Methody korrektsii hormonalnogo disbalansa u genshchin s syndrom prejdevremennoy dostatochnosti yaichnikov // A new day in medicine. - Tashkent, 2021. - No. 3 (35/1). -S. 203-206. |
| [10] | Naуimova, N.S., Karimova, N.N. (2022) Disharmony and its correction in premature ovarian insufficiency. Journal of Pharmaceutical Negative Results, 13, DOI: 10.47750/pnr.2022.13.S08.409. |
| [11] | Yoldoshevich, P. O., & Nabidjanovna, K. N. (2020). Retrospective analysis of the birth histories of women who have suffered bleeding in order to optimize approaches to the prediction and prevention of postpartum bleeding. European Journal of Molecular and Clinical Medicine, 7(2), 6236-6243. Retrieved from www.scopus.com. |
| [12] | Karimova N.N., Ayupova F.M., Rustamov M.U. “Analysis of childbirth stories with postpartum hemorrhage, taking into account rehabilitation measures and future of reproductive system after massive obstetric bleeding” International // Journal of Pharmaceutical Research, / Jan-Mar 2019/Vol 11. Issue 1. -Р. 1690-1695. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML