-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 719-725
doi:10.5923/j.ajmms.20241403.39
Received: Feb. 15, 2024; Accepted: Mar. 12, 2024; Published: Mar. 16, 2024

Role of the Peroneal Artery in Limb Salvage in Patients with Chronic Limb – Threating Ischemia and Diabetes Mellitus
Bakhtiyor Tursunov, Surat Temirov, Hoshim Usmanov
Central Hospital of the Ministry of Internal Affairs, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of this study was to assess the efficacy of peroneal artery endovascular revascularization in LS in patients with peripheral artery disease and DM complicated with Chronic Limb-Threatening Ischemia. Background: The primary treatment for Chronic Limb-Threatening Ischemia is limb salvage through aggressive management and early revascularization. However, in patients with diabetes mellitus, it is technically not feasible to restore pulsating arterial blood flow to the pedal arch through the tibial arteries due to extensive lesions along the entire length of these arteries. The significance of peroneal revascularization in these cases is still a matter of debate. Material and methods: This study is a retrospective analysis of patients who had treatment in the department of specialized surgery of the Central Hospital of the Ministry of Internal Affairs of the Republic of Uzbekistan from 2012 to 2022. The study included patients with Chronic Limb-Threatening Ischemia and DM. All patients were exhibited either chronic ischemic rest pain within the past two weeks or ulceration/gangrene caused by peripheral artery disease. The patients were divided into two cohorts: the first cohort consisted of 23/24 patients/extremities who underwent peroneal revascularization, while the second cohort comprised 95 individuals/extremities who underwent revascularization of one of the tibial arteries. Results: The treatment outcomes of 117 individuals with CLTI were analyzed. The mean preprocedural ankle-brachial index (ABI) was 0.42±0.1 in the PR group and 0.44±0.09 in the TR. After the procedure, the ABI in the PR group increased to 0.81±0.07, and in the TR group to 0.86±0.05. At the 6-month following revascularization, the ABI in the groups was measured to be 0.76±0.13 and 0.77±0.14, respectively. One year later, the ABI values were recorded as 0.66±0.15 and 0.68±0.14, respectively. Conclusions: Although the follow-up results PR is not comparable with the TR, it is essential for endovascular surgeons to always consider using PR as a treatment option. This is particularly important for patients with DM, since they commonly have extensive calcification of the tibial arteries across their whole length.
Keywords: Chronic Limb-Threatening Ischemia, Peroneal artery, Revascularizarion, Endovascular
Cite this paper: Bakhtiyor Tursunov, Surat Temirov, Hoshim Usmanov, Role of the Peroneal Artery in Limb Salvage in Patients with Chronic Limb – Threating Ischemia and Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 719-725. doi: 10.5923/j.ajmms.20241403.39.
1. Introduction
- Chronic Limb-Threatening Ischemia (CLTI) is the most severe manifestation of peripheral arterial disease (PAD), characterized by a significant risk of major amputation, cardiovascular events, and mortality [1]. Individuals diagnosed with diabetes mellitus (DM) face a substantially higher risk, ranging from 2 to 7 times greater, of developing peripheral artery disease (PAD) [2]. The advancement of atherosclerosis and the likelihood of negative consequences are more frequently observed in diabetic patients with PAD, likely due to the aberrant metabolic condition and heightened arterial inflammation [3]. Limb salvage (LS) is the first line treatment for CLTI in eligible patients, involving early revascularization. However, in patients with DM, it is technically impossible to restore pulsatile arterial blood flow to the pedal arch through the tibial arteries due to extensive lesions along their entire length. The significance of peroneal revascularization (PR) is still a matter of debate, particularly in patients with severe tissue loss. It is believed that restoring pulsatile arterial blood flow to the pedal arteries is crucial for wound healing, making the role of PR yet to be determined. Simultaneously, the peroneal artery (PA) is less affected by severe atherosclerotic lesions [4], and its branches that directly link the peroneal artery (PA) to the dorsal pedis artery or/and plantar arteries may have a crucial impact when no other revascularization alternative is available. The aim of this study was to assess the efficacy of peroneal artery endovascular revascularization in LS in patients with PAD and DM complicated with CLTI.
2. Material and Methods
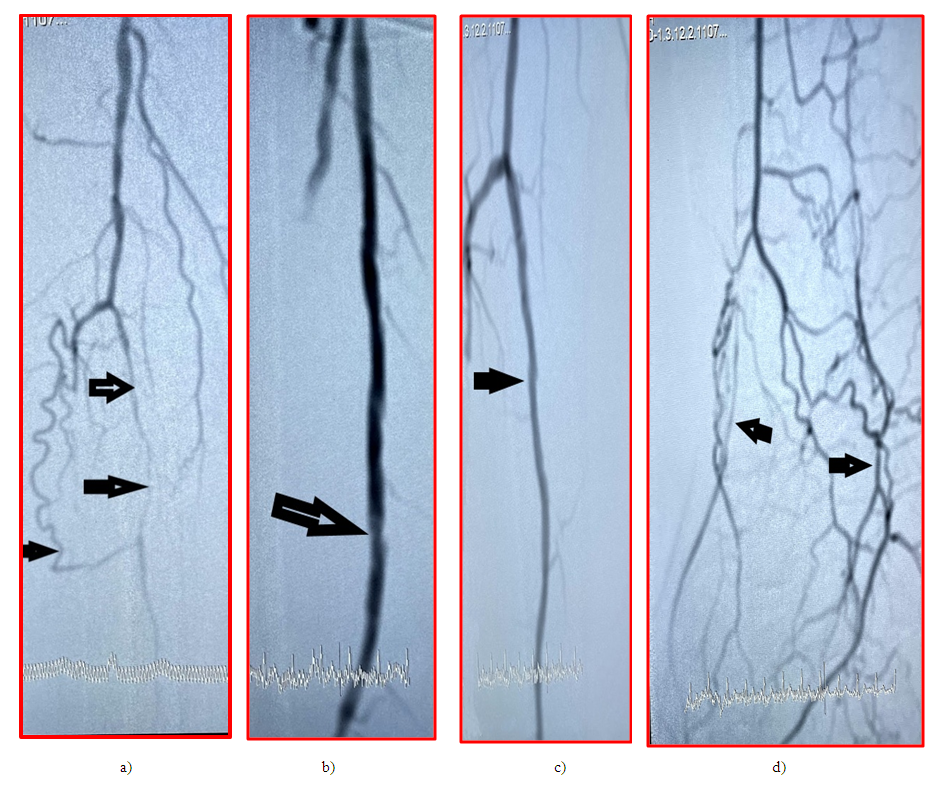
- This study presents a retrospective analysis of patients who received treatment in the department of specialized surgery of the Central Hospital of the Ministry of Internal Affairs of the Republic of Uzbekistan from 2012 to 2022. The study included patients with CLTI and DM. All patients were with either ischemic rest pain over the past two weeks or ulceration/gangrene caused by PAD.The patients were categorized into two cohorts: the first cohort consisted of patients with PR, while the second cohort consisted of patients with revascularization of one of the tibial arteries (TR). The study excluded patients who had undergone revascularization of more than one artery. The statistical study of demographic data for comparison encompassed variables such as age, gender, heart diseases, arterial hypertension, chronic cerebrovascular insufficiency, and chronic kidney illness. Furthermore, an examination was conducted to assess the biochemical blood parameters and hemodynamic characteristics of the affected foot. The instrumental examinations comprised echocardiography, ABI evaluation, CT angiography, and MR angiography.The affected limb underwent preoperative examination based on the WIFi classification. All procedures were carried out under local anesthesia. The ipsilateral femoral antegrade access was predominantly selected, with a few exceptions where an ipsilateral retrograde tibial approach was used due to the impossibility to perform antegrade recanalization of the tibial arteries. Following the installation of a 6 French sheath, a dosage of unfractionated heparin at a rate of 70 units per kilogram was delivered. Prior to attempting recanalization, all patients underwent diagnostic angiography intraoperatively. A revascularization plan was then formulated based on the following criteria: if both tibial arteries are completely occluded over their whole length and the distal part of the PA remains open, the target for revascularization is identified as the PA. If the distal portion of the tibial arteries remains open and enables blood flow to the arterial arch of the foot, a tibial revascularization procedure is performed. The angiographic pictures taken before and after procedure were examined retrospectively to assess the consistency of the pedal arterial arch and the existence of functional branches of the PA that connect PA with the pedal arterial arch.Hydrophilic 0,014–300,0 cm guidewires were used to recanalize all of the tibial arteries, and balloons with a diameter of 2-4 mm were used for angioplasty. Before the procedure, the patients received aspirin and clopidogrel 75 mg, 1 tablet once a day for at least one week, or a loading dose of clopidogrel was prescribed before or on the day of the procedure at a dosage of 300 mg/day. After successful recanalization, patients received a combination of aspirin and clopidogrel 75 mg/day for at least a year.The restoration of pulsative flow to the pedal arch with no more than 30% residual stenosis was accepted as a technical success. The criteria for clinical success were: pedal palpable pulse with warming of the foot and relief of the rest pain, when restoring the PA - warming of the foot and relief of the rest pain with the presence of biphasic blood flow on the PA on an ultrasound scan.Complications of the procedure are divided into major and minor. Thrombosis or hematoma of a punctured artery necessitating surgical intervention, postoperative infarction, stroke was regarded as major perioperative complications. Hemostasis in the puncture site that did not necessitate surgery was regarded as a minor complication.After the procedure, patients were observed at one-month intervals until the wound was completely healed. Every six months, clinical follow-up appointments were made once the wound had fully healed. ABI measurements on the recanalized artery were routinely performed at hospital discharge, 6 and 12 months after the procedure or recurrence of symptoms of CLTI.Primary endpoints were rest pain relief, healing time and rate after the endovascular revascularization. Wound healing was defined as complete epithelialization of all wounds.Secondary endpoints included major amputation-free survival and freedom from major adverse limb ischemic event (MALE) at 5 years.Statistics: IBM SPSS, version 20.0, was used to conduct statistical analysis. P<0.05 was designated as the level of statistical significance. Lesion characteristics were summarized per lesion, while baseline demographics and clinical features were summarized per participant. For baseline characteristics, dichotomous and categorical variables were represented as counts and proportions, and the Fisher exact test was used to compare them; continuous variables were described as mean ± SD. Subject-level outcome analyses were carried out. Over the course of the 60-month follow-up period, time to event data for freedom from amputation and freedom from MALE were assessed using the Kaplan-Meier approach. The log-rank test was used to evaluate the variation in survival curves between treatment groups.
3. Results
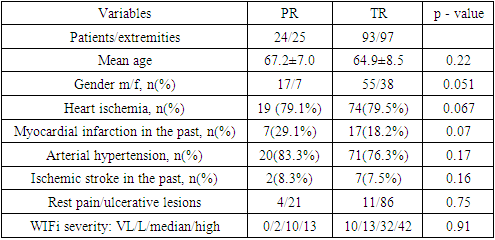
- The treatment results of 117 patients with 122 extremities with CLTI were analyzed; the patients' average age was 65.1±8.2 years, and 77 (65.8%) of them were men. Every patient had diabetes. The patients were divided into two groups of patients: the first group with PR had 24 patients with 25 extremities with a mean age of 67.2±7.0 years; 19 men (79,1%) made up this group. The TR group had 93 patients with 97 extremities and a mean age of 64.69±8.5 years; 58 men (62.3%) made up this group. The antiplatelet medication regimen, comorbidities, and demographic factors were comparable. Based on the WIFi categorization, the majority of patients in all groups were with ulcerative/gangrene lesions (Table 1).
|
|
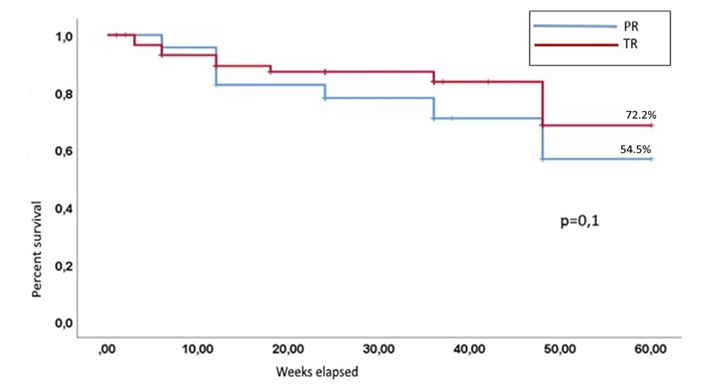 | Figure 1. Amputation free survival for 5 years |
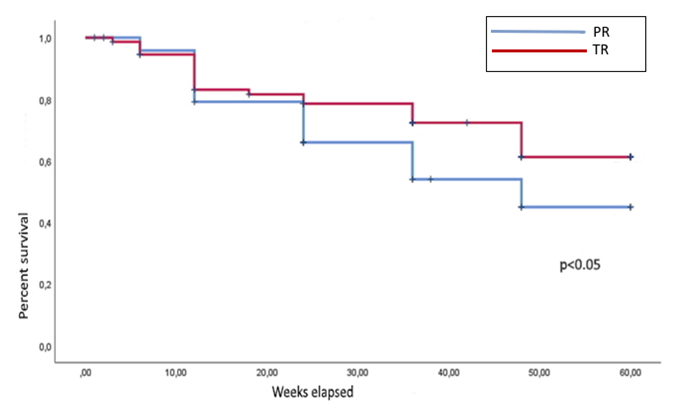 | Figure 2. 5 years’ freedom from MALE |
4. Discussion
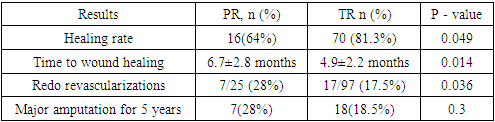
- For a while, it was accepted that PR alone was insufficient to treat severe ischemic ulcerative-necrotic lesions. Faglia E et al., who concluded that recanalization and restoration of the peroneal artery will not always be adequate to save the limb in a comparative assessment of direct and indirect revascularization of the foot [5], were among those who supported this theory. Nevertheless, the outcomes of open surgical interventions contradict this theory. As a result, Raftery KB et al.'s work [6] showed that the outcomes of shunts placed in the peroneal arteries are comparable to those of anterior and posterior tibial bypasses. Subsequently, other studies have been released that further support the PA's efficacy, but they also touch on the outcomes of open surgical procedures [7,8]. This means that the outcomes of revascularization of the foot using the tibial arteries and endovascular revascularization of the peroneal artery should not be too dissimilar from one another. Even so, published works occasionally contradict one another. In terms of amputation-free survival, PR performed worse in the study conducted by Ghoneim B et al. [9] than single-vessel tibial revascularization. In terms of frequency and wound healing duration, further research has demonstrated that PR can produce results comparable to those of single-vessel tibial revascularization [10]. Similar findings were reported by Dosluoglu et al. [2008], who discovered no appreciable variations between PR and TR with regard to preservation of patency and amputation survival one year following surgery [8]. Our findings further demonstrate that, in terms of wound healing rate and duration, TR outcomes are better comparable to those of PR. All authors agree that revascularization of the lower limb using the peroneal artery is sufficient to treat the symptoms of critical ischemia in cases of critical ischemia without an ulcerative/gangrene process [8,9,10]. We also observed that following PR, patients get a reduction in rest pain and are able to walk 200–300 meters pain-free. The target arterial pathway's preservation for a year, as determined by the GLASS classification, is another indicator: the patency of the restored artery following surgery [12]. Additionally, it mentions that when the findings of the TR group were compared with those of the PR group, amputation-free survival was significantly higher; however, this data was not statistically significant, and the same conclusions were reported in the work of Dosluoglu et al [8]. To evaluate the patency of the restored artery, we examined the frequency of follow-up revascularization procedures. At the same time, compared to the group that underwent TR, the rate of repeat interventions following the PR procedure was significantly higher (23% versus 39%).If you carefully analyze the graph of 5-year amputation free survival and MALE free survival (Figures 1 and 2), in the early postoperative period the frequency of amputation is approximately the same in both groups, but over time the probability of losing of target arterial pathway in the group with PR increases and, accordingly, the difference amputation and MALE indicators increase at the end of the follow up period. Moreover, most repeated interventions are also performed after a year from the first procedure.The issue of which factors impact PR outcomes is frequently subject to discussion. According to numerous authors, the determining factor in achieving a long-lasting favorable outcome is the condition of the terminal branches of the PA. In theory, this assumption is accurate, as it is the efferent vessels that determine whether it is a shunt, a prosthesis, or an endovascularly reconstructed artery. Furthermore, the fate of the restored PA depends on the patency status of the posterolateral malleolar and connecting artery. Obtaining a favorable outcome relies on achieving adequate blood flow from at least one of these arteries to the plantar arteries or foot dorsal arteries. This viewpoint is shared by other authors. In the study conducted by Ricco JB et al (2017), it was demonstrated that the outcome of foot revascularization using PA is influenced not only by the condition of the smaller arteries in the foot, but also by the condition of the main arterial structure in the foot [11]. Our investigation revealed that when both terminal branches of the PA are patent, the rate of wound healing can reach up to 86%. However, in cases where the terminal branches are not patent, only 35% of patients achieve recovery.
5. Conclusions
- Although the follow-up results are unsatisfactory, it is essential for endovascular surgeons to always consider using PR as a treatment option. This is particularly important for patients with DM, since they commonly have extensive calcification of the tibial arteries across their whole length. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML