-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 705-707
doi:10.5923/j.ajmms.20241403.36
Received: Feb. 12, 2024; Accepted: Mar. 3, 2024; Published: Mar. 9, 2024

Study of Dyslipidemia in Women with Polycystic Ovarian Disease with Infertility and Obesity
Shokirova S. M., Zufarova Sh. A., Israilov R. I.
Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Women with polycystic ovary syndrome (PCOS) and obesity have sex hormone disorders and insulin resistance (IR) compared to patients with normal body weight [4]. In addition, it is assumed that a number of metabolic disorders are also associated with obesity and 70% of obese women have at least one abnormal lipid profile [5]. Under conditions of IR and excess free fatty acids, lipid metabolism is also disrupted and atherogenic dyslipidemia develops. Due to the slowdown in the catabolism of triglycerides and triglyceride-rich lipoproteins, increased accumulation of very low-density lipoproteins, cholesterol accumulates in macrophages, increases the level of modified low-density lipoproteins, which have a high ability to oxidize and penetrate into the subendothelial space of the vascular wall, and have a high affinity for LDL receptors. All these properties contribute to the active inclusion of small dense LDL particles in the process of atherogenesis [1]. Polycystic ovary syndrome is widely recognized as the most common endocrine abnormality in women of childbearing age and may be associated with dyslipidemia, hyperandrogenism, oxidative stress, and infertility. It is now known that dyslipidemia plays an important role in the development of PCOS. Lipid abnormalities, including increased levels of low-density lipoprotein and triglycerides and decreased levels of high-density lipoprotein, are often found in women with PCOS and play an important role in PCOS. [6].
Keywords: PCOS, Dyslipidemia, Obesity, Infertility
Cite this paper: Shokirova S. M., Zufarova Sh. A., Israilov R. I., Study of Dyslipidemia in Women with Polycystic Ovarian Disease with Infertility and Obesity, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 705-707. doi: 10.5923/j.ajmms.20241403.36.
1. Introduction
- The study examined 60 women with polycystic ovary syndrome and infertility, 56 women with polycystic ovary syndrome (PCOS) and obesity, and 46 women with PCOS, infertility and obesity. In the blood of the examined women, indicators of total cholesterol, triglycerides, high-density lipoproteins (HDL) and low-density lipoproteins (LDL) were studied using a biochemical method, using standard sets of Vector-Best reagents produced in Russia.
2. Results
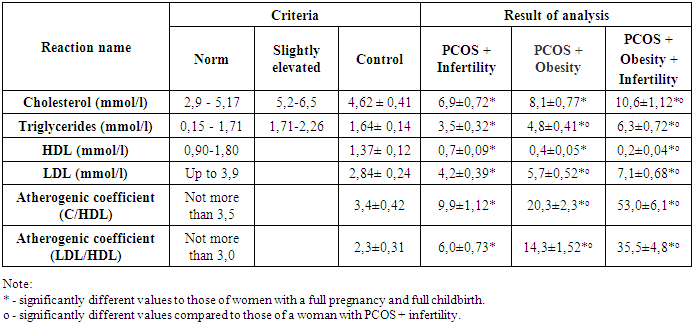
- From the research results, it was revealed that in women with full-fledged pregnancy and full-fledged childbirth (control), the total cholesterol level in the blood was 4.62 ± 0.41 mmol/l (Table 1). The same indicator in women with PCOS and infertility was 6.9±0.72 mmol/l, which was significantly (R<0.05) 1.5 times higher than that of women with a full-fledged pregnancy. At the same time, the result of total cholesterol in women with PCOS and obesity was 8.1±0.77 mmol/l, which was significantly (R<0.001) 1.8 times higher than the results of women with full-fledged pregnancy and not significantly 1.2 times higher than women with PCOS and infertility. At the same time, this indicator in women with PCOS, infertility and obesity was significantly (R<0.001) and 2.3 times higher than the same result in women with full-fledged pregnancy and amounted to 10.6±1.12 mmol/l, also significant (R <0.05) is 1.5 times higher than the results of women with PCOS and infertility (Table 1).In addition, it was found that in women with full-fledged pregnancy and full-fledged childbirth, the triglyceride level in the blood was 1.64 ± 0.14 mmol/l. At the same time, in women with PCOS and infertility, the result of triglycerides was 3.5±0.32 mmol/l, which was significantly (R<0.001) 2.1 times higher than that of women with a full-fledged pregnancy. At the same time, the triglyceride indicator in women with PCOS and obesity was 4.8±0.41 mmol/l, and was significantly (R<0.001) 2.9 times higher than the indicators of women with full-fledged pregnancy and also significantly (R<0.05) 1.4 times higher than women with PCOS and infertility. Also, the indicator in women with PCOS, infertility and obesity was significantly (R<0.001) and 3.8 times higher than the same result for women with full-fledged pregnancy and amounted to 6.3±0.71 mmol/l, also significant (R<0.05) 1.5 times higher than the results of women with PCOS and infertility (Table 1).
|
3. The Discussion of the Results
- The presented results showed that in women with PCOS and infertility, the total cholesterol level significantly increased in relation to the results of women with a full-fledged pregnancy. In women with PCOS and obesity, this indicator also increased significantly, but more significantly in relation to the results of women with a full-fledged pregnancy; it also did not significantly increase in women with PCOS and infertility. In women with PCOS, infertility and obesity, the total cholesterol level increased more significantly compared to the results of women with a full-fledged pregnancy and also significantly increased compared to the results of women with PCOS and infertility. A similar trend in changes in triglycerides was observed in women with full-fledged pregnancy and full-fledged childbirth; this indicator in women with PCOS and infertility increased significantly in relation to the results of women with full-fledged pregnancy. In women with PCOS and obesity, the level of triglycerides also significantly and significantly increased compared to the indicators of women with full-fledged pregnancy, and also significantly increased in comparison with women with PCOS and infertility. At the same time, in women with PCOS, infertility and obesity, a more pronounced and significant increase in triglycerides was observed in relation to the results of women with a full-fledged pregnancy and also significantly increased in relation to the results of women with PCOS and infertility. The opposite trend in relation to cholesterol and triglycerides was observed when studying HDL. It was found that in women with a full-fledged pregnancy and full-fledged childbirth, the HDL level significantly decreased in comparison with the results of women with a full-fledged pregnancy. At the same time, in women with PCOS and obesity, this indicator decreased significantly and significantly in relation to the results of women with a full-fledged pregnancy and not significantly in comparison with women with PCOS and infertility. In women with PCOS, infertility and obesity, the HDL result decreased more significantly compared to the same indicator for women with a full-fledged pregnancy and also significantly decreased in relation to the results of women with PCOS and infertility. When studying LDL, a similar trend was noted for both cholesterol and triglycerides, an increase in these indicators in relation to the results of women with full-fledged pregnancy, in women with PCOS and infertility, a more significant increase in women with PCOS and obesity, as well as a more significant increase in women with PCOS, infertility and obesity. There was also an increase in LDL cholesterol compared to women with PCOS and infertility, results in women with PCOS and obesity, and a more significant increase in women with PCOS, infertility and obesity. Against the background of these changes, a similar direction of changes was noted in cholesterol, triglycerides and LDL, atherogenic coefficients C/HDL, LDL/HDL, with an increase in these indicators in women with PCOS and infertility in relation to similar indicators in women with full-fledged pregnancy. Also, a more significant increase in C/HDL and LDL/HDL in women with PCOS and obesity, as well as a more significant increase in women with PCOS, infertility and obesity in relation to similar indicators in women with full-fledged pregnancy. A similar direction of these indicators was noted in comparison to women with PCOS and infertility, results of women with PCOS and obesity, as well as a more significant increase in women with PCOS, infertility and obesity. In general, these changes show the development of dyslipidemia in relation to women with full pregnancy in women with PCOS and infertility, which increased in women with PCOS and obesity. At the same time, dyslipidemia increased more significantly in women with PCOS, infertility and obesity in relation to women with full pregnancy, as well as women with PCOS and infertility. There was also a greater increase in dyslipidemia in women with PCOS, infertility and obesity compared to women with full pregnancy and women with PCOS and infertility.
4. Conclusions
- The data obtained showed that in women, in women with PCOS and infertility, the development of dyslipidemia was noted in relation to women with a full-fledged pregnancy. Dyslipidemia increased in women with PCOS and obesity and increased more significantly in women with PCOS, infertility and obesity in relation to women with full pregnancy, as well as women with PCOS and infertility. At the same time, a more significant increase in dyslipidemia was observed in women with PCOS, infertility and obesity in relation to both women with full-fledged pregnancy, as well as women with PCOS and infertility.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML