Shukurova Lobar Khusanovna1, Daminova Lola Turgunpulatovna2, Babadjanova Nozima Ravshanbekovna3
1Senior Lecturer, Tashkent State Dental Institute, Tashkent, Uzbekistan
2DSc., Professor, Tashkent State Dental Institute, Tashkent, Uzbekistan
3Associate Professor, Tashkent State Dental Institute, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The purpose of the study: Study of the effect of calcium dobesilate on indicators of the hemostasis system in patients with chronic kidney disease in stages II-III. Materials and methods: 120 patients with II-III stage of chronic kidney disease were taken under observation, 45 of them had diabetic nephropathy. Depending on the therapy, patients were divided into 2 groups. The first group of patients received the standard treatment of chronic kidney disease, and the second group received calcium dobesilate added to the standard treatment. In dynamics (3 months), indicators of the hemostasis system were evaluated: fibrinogen, thrombus test, APPT, platelet aggregation. The results of the study: In patients with non-diabetic nephropathy in the group with the addition of calcium dobesilate, after 3 months of therapy, a significant decrease in platelet aggregation and an increase in APPT (p<0,01) were found compared to group 1 (p<0,001), the same trend was observed in the normalization of platelet aggregation in patients with diabetic nephropathy. Conclusion: Thus, the addition of calcium dobesilate drug to the treatment regimen of patients with CKD of diabetic and non-diabetic etiology significantly improves the parameters of the hemostasis system of the kidneys.
Keywords:
Chronic kidney disease, Platelet aggregation, Diabetic nephropathy, Calcium dobesilate
Cite this paper: Shukurova Lobar Khusanovna, Daminova Lola Turgunpulatovna, Babadjanova Nozima Ravshanbekovna, The Effect of Calcium Dobesilate on Indicators of Hemostasis System in Patients with Chronic Kidney Disease Stage II-III, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 701-704. doi: 10.5923/j.ajmms.20241403.35.
1. Introduction
Chronic kidney disease became a real pandemic in the first quarter of the last century, and it took the fifth place among non-infectious diseases that cause death. Also, CKD is a risk factor for cardiovascular pathologies and death caused by it. At the same time, during this period, the social scope of this disease was expanded, and its control and treatment-prevention measures were not well developed, but it became one of the urgent issues for the health care system of countries with leading economies in the world. [1]According to statistics, in 2010, 2,6 million patients worldwide were treated with extracorporeal detoxification. More than 90% of them are residents of developed and moderately developed countries, that is, with an average or higher economy. On the other hand, based on prevalence estimates, an average of 5 million patients with CKD require renal replacement therapy. About 2,3 million of them do not have access to renal replacement therapy in a timely manner [6]. Of course, it increases the rate of inevitable death in this patient population. Economic and social problems and poverty are the main obstacles to receiving kidney replacement therapy here [3].It is known that from the initial stages of chronic kidney disease, the control of the anti-aggregation state of blood is disturbed, and procoagulation in this system is evident in glomerulopathies. It is stable during the manifestation of chronic kidney disease, especially in the terminal stage [5]. Kidney damage is associated with the activation of blood vessel-platelet interaction. Despite the bright and systematic nature of the facts that have been studied and discovered so far, the complexity of the pathogenetic aspects of this system and the hemostasiological phenomena of chronic kidney diseases require a more in-depth study.
2. Materials and Methods
120 people who were undergoing inpatient treatment in the nephrology department of the multidisciplinary clinic of the Tashkent Medical Academy and were subsequently under outpatient supervision at this institution were taken for the study. The diagnosis and the functional state of the kidneys were formed on the basis of laboratory and instrumental examinations in medical institutions. Markers of kidney damage (urinary syndrome) and functional state of the kidney were studied in patients of the group 1 (1 A (n-35) and 1 B (n-40)), consisting of patients of the II and III A stages of CKD formed on the basis of nephropathies of nondiabetic etiology (n-75) and in patients of the group 2 (2 A (n-20) and 2 B (n-25)) consisting of patients of the II and III A stages of CKD formed on the basis of diabetic nephropathy (n-45). Patients belonging to group A received only traditional therapy according to the recommendations for the treatment of CKD. Patients belonging to group B, in addition to this therapy, received a drug that inhibits ADP receptors – calcium dobesilate drug for three months. All patients were examined for coagulogram indicators and adenosine diphosphate acid inducers of platelet aggregation at the beginning of treatment and at the end of the study. The results were statistically analyzed.
3. Results and Their Discussion
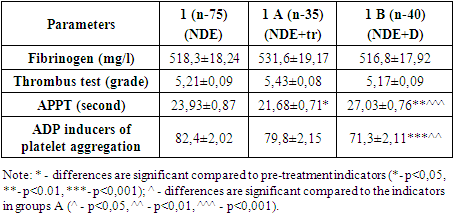
In our study, the dynamics of changes in the indicators of the hemostasis system in patients with CKD, formed on the basis of various genesis nephropathies, against the background of various treatment schemes, manifested the following picture. Fibrinogen at the beginning of the study was 518,3±18,24 mg/l in group 1 of patients with CKD developed on the basis of non-diabetic genesis nephropathies, at the end of the study, it was slightly increased by 531,6±19,17 mg/l in group 1 A, which was limited to traditional treatment only. In the case of group 1 B, which took the calcium dobesilate drug in addition to the traditionalist treatment, it was found that 516,8±17,92 mg/l was attenuated imperceptibly. Although it has been observed that group A has slightly increased indicators and decreased in group B, this does not matter. It was observed that the reason was that all values changed unreliable (p>0,05) when the results were statistically analyzed (Table 1).Table 1. Dynamics of changes in the treatment background of hemostasis system indicators in chronic kidney diseases with non-diabetic genesis
 |
| |
|
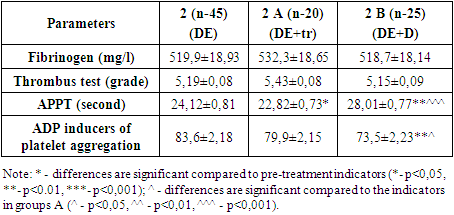
The thrombus test was 5,21±0,09 degrees at the beginning of the study in group 1, and increased to 5,43±0,08 degrees in group 1 A at the end of the study. It was found that it decreased to 5,17±0,09 degrees in group 1 B. The results showed an unreliable (p>0,05) change in all values when statistically analyzed (Table 1). During our studies, this condition in the fibrinogen and thrombus test is explained by the fact that there is no anticoagulant effect of this calcium dobesilate drug.APPT in group 1 was 23,93±0,87 seconds at the beginning of the study and decreased to 21,68±0,71 seconds in group 1 A at the end of the study, in the case of group 1 B, which took the additional calcium dobesilate drug, it increased to 27,03±0,76 seconds and showed normative indicators. Statistical analysis of the results showed a low reliable (p<0,05) decrease in APPT value in group 1 A after treatment compared to the beginning of the study, as well as a reliable (p>0,01) increase in group 1 B. When the results of the study were compared among themselves, it was confirmed in statistical analysis that APPT was reliably (p>0,001) changed in group B compared to group A (Table 1).ADP inducers of platelet aggregation were 82,4±2,02% at the beginning of the study in group 1 and decreased by 79,8±2,15% in group 1 A at the end of the study and in group 1 B, which received additional calcium dobesilate drug, decreased by 71,3±2,11%, showed normative parameters. Statistical analysis of the results showed that the values after the treatment compared to the beginning of the study did not change reliably in group 1 A, while it was observed that they decreased reliably (p>0,001) in group 1 B. When the results of the study were compared with each other, the reliable (p>0,01) change of ADP inducers of platelet aggregation in group B compared to group A was confirmed in statistical analysis (Table 1).In group 2, consisting of patients with CKD developed on the basis of diabetic nephropathy, at the beginning of the study, fibrinogen was 519,9±18,93 mg/l, and at the end of the study, it was found to increase in lower values to 532,3±18,65 mg/l in group 2 A, in group 2 B, which took the calcium dobesilate drug in addition to the treatment, fibrinogen decreased imperceptibly to 518,3±18,14 mg/l. Although it has been observed that group A slightly increases the indicators and group B decreases at small values, these changes do not matter. Because, statistical analysis shows that all values in study groups have changed unreliable (p>0,05) (Table 2).The thrombus test was 5,19±0,08 degrees at the beginning of the study in group 2 and increased to 5,43±0,08 degrees in group 2A at the end of the study. In group 2 B, it decreased to 5,15±0,09 degrees. When the results were statistically analyzed, all values were observed to change unreliably (p>0,05) (Table 2). This is also explained in our study by the fact that this condition in the fibrinogen and thrombus test does not observe an anticoagulant property in the calcium dobesilate drug.APPT was found to be 24,12±0,81 seconds at the beginning of the study in group 2. At the end of the study, it decreased to 22,82±0,73 seconds in group 2 A, and increased to 28,01±0,77 seconds in group 2 B, which received additional calcium dobesilate drug for three months. In the statistical analysis of the results, compared to the beginning of the study, it is important that the APPT value decreased in group 2 A, although it was less reliable (p<0,05), and it increased reliably (p>0,01) in group 1 B. When comparing the results at the end of the study, it was proved on the basis of statistical analysis that the APPT was reliably (p>0,001) changed in group B compared to group A (Table 2).Table 2. Dynamics of changes in the treatment background of the indicators of the hemostasis system in chronic kidney diseases with diabetes genesis
 |
| |
|
ADP inducers of platelet aggregation were 83,6±2,18% at the beginning of the study in group 2, and decreased to 79,9±2,15% in group 2 A, also it decreased to 73,5±2,23% in group 2 B at the end of the study. Statistical analysis of the results showed that the values after the treatment did not change reliably in group 2 A compared to the beginning of the study, and they decreased reliably (p>0,01) in group 2 B. Comparing the results at the end of the study, compared to group A, ADP inducers of platelet aggregation were less reliably (p>0,05) changed in group B (Table 2).Now we will look at the dynamics of changes in the indicators of the hemostasis system in certain study groups against the background of various treatment schemes. According to him, at the end of the three-month follow-up, after the treatment, in the chart based on fibrinogen, although the indicators increased in groups A and decreased in groups B, these changes were not significant. The reason is, the statistical analysis carried out shows that at the end of the study, all values in the groups have changed unreliable (p>0,05).Diagram based on the thrombus test showed the same picture. According to him, after three months of study observations, after treatment, although the indicators increased in groups A and decreased in small amounts in groups B, these changes were not significant. Because, when the results of thrombus tests were statistically analyzed, it was found that all the values in the groups did not change reliably (p>0,05) after the treatment.This condition in our study, that is, the unreliable (p>0,05) change of fibrinogen and thrombus test during observation, indicates that the anticoagulant effect of calcium dobesilate drug is not present. However, there has been significant variation in fibrinogen and thrombus test rates in groups B that take the calcium dobesilate drug compared to groups A that do not take the drug. The reason is, study by Murashko E.Yu. and other co-authors (2017) has noted that dobezelate reduces blood viscosity by lowering fibrinogen levels while reducing calcium platelet aggregation [3].If we look at the diagram formed by the results of APPT, it is important that after treatment, the APPT value decreased in groups A, although it was less reliable (p<0,05), and it increased reliably (p>0,01) in group B. When the results are compared with each other, the reliable (p>0,01) change of APPT in group B compared to group A is explained as the anti-aggregant property of calcium dobesilate drug recommended to patients of group B for three months.It is important to monitor the activity of ADP inducers of platelet aggregation in patients with CKD of any genesis, not only diabetes etiology. It was recognized that hyperaggregation of platelets in any patient causes cardiovascular events, and hypoaggregation causes hemorrhagic complications [4]. In addition, this control becomes even more relevant in case of kidney failure. The reason is that hemostasis disorders in patients with CKD also have their own characteristics. Alternative disorders of hemostasis are observed especially in terminal renal failure. That is, there is a fine balance between bleeding and thrombotic complications in patients, and it is extremely easy for an imbalance to occur in this interval [2].Thus, the antiaggregatory effect of calcium dobesilate drug in patients with CKD developed on the basis of nephropathies of various etiologies showed the same results. It was reflected not only in the adjustment of APPT indicators, but also in the reduction of platelet aggregation inducer activity of ADP in the final results of the treatment in various schemes, which effectively block the ADP P2Y12 receptors on the platelet membrane. At the same time, the drug is an effective inhibitor of VEGF (Vascular Endothelial Growth Factor), which has a positive effect on the proliferation of endothelial cells and improves blood permeability, i.e. blood flow, in diabetes mellitus [3]. Also, this drug has a positive effect on blood rheology, reduces its viscosity by reducing platelet aggregation and reducing fibrinogen levels. This effect is important in macro- and microangiopathies, retinopathy and other microcirculatory disorders, as well as in nephroangiopathy in renal failure. Therefore, it is appropriate to use calcium dobesilate drug in patients with CKD of all genesis.
References
| [1] | Batyushin M.M. Chronic kidney disease: current state of the problem. Rational Pharmacotherapy in Cardiology 2020; 16(6): 938-947. DOI:10.20996/1819-6446-2020-11-06. |
| [2] | Yesayan A.M., Arutyunov G.P., Melikhov O.G. Prevalence of chronic kidney disease among patients presenting to primary care. Results of a prospective observational study in 12 regions of Russia // Nephrology (vol. 13) No. 3. 2021. pp. 6 - 16. DOI: https://dx.doi.org/10.18565/nephrology.2021.3.6-16. |
| [3] | Murashko E.Yu. Calcium dobesilate as an early angioprotector in diabetic microangiopathies. 2017; 22: 1629-1634. https://www.rmj.ru/articles/endokrinologiya/Dobezilat_kalyciya_kak_ranniy_angioprotektor_pri_ diabeticheskih_mikroangiopatiyah/#ixzz8J0vZW1jO. |
| [4] | Obrezan A.G., Zemchenkov A.Yu. Chronic kidney disease as the basis for an increased risk of hemorrhagic and thrombotic complications in patients with atrial fibrillation: the place of oral anticoagulants. // Cardiology. 2018; 58(4): 60–70. |
| [5] | Huang MJ, Wei RB, Wang ZC, et al. Mechanisms of hypercoagulability in nephrotic syndrome associated with membranous nephropathy as assessed by thromboelastography. Thrombosis Research. 2015; 136(3): 663-668. https://doi.org/10.1016/j.thromres.2015.06.031. |
| [6] | NCD Risk Factor Collaboration Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017; 389: 37–55. |
| [7] | NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016; 387: 1513–30 NCD Risk-2017, Xie Yan-2018. |
| [8] | In the same time Adams M.J. et al. Adams M.J. et al. // Thrombosis Research 2008. V. 123. Issue 2. P. 374-380. |
| [9] | SardarP. ChatterjeeS., HerzogE., etal. Novel oral anticoagulants in patients with renal insufficiency: a meta-analysis of randomized trials. CanJCardiol 2014; 30(8): 888-97. |
| [10] | Barnoyev Khabib Bobomurodovich, Shukurova Lobar Khusanovna, Khusankhodjaeva Feruza Tulkunovna ASSESSMENT OF RENAL FUNCTIONAL RESERVE AGAINST THE BACKGROUND OF ANTIPLATELET THERAPY IN THE II-III STAGE OF CHRONIC KIDNEY DISEASE // ORIENSS. 2021. No. 3. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML