Akhmatova Gulrukh Rakhmatovna
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Akhmatova Gulrukh Rakhmatovna, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Papillomavirus infection is one of the most common sexually transmitted infections. Women in the 18-30 age group are most susceptible to infection. The article is devoted to the study of indicators of the prognosis of papillomavirus-associated cervical diseases in women of fertile age, which is of great importance for health authorities in the organization of specialized gynecological and onco-surgical services. The diagnostic markers proposed by the author allow early diagnosis and prevention of cervical cancer in women of fertile age, which is of great practical importance.
Keywords:
Cancer markers, Cervix, Women of fertile age, Human papillomavirus, Cancer
Cite this paper: Akhmatova Gulrukh Rakhmatovna, Diagnostic Markers of Papilloma Virus-Associated Cervical Diseases in Women of Fertile Age, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 698-700. doi: 10.5923/j.ajmms.20241403.34.
1. Introduction
Human papillomavirus (HPV) of the high oncogenic risk group is found in 99.7% of women with a histologically confirmed diagnosis of breast cancer, which, according to WHO, is more than 500,000 women per year [5].Most cases of breast cancer occur in the so-called transformation zone, which is a junction between the proximal single-layered gelatinous epithelium and the distal multilayered squamous epithelium. To date, it is known that in an infected cell, the virus can exist in two forms: episomal (productive) and integrative (transforming) [2].In recent years, there has been a tendency in many countries of the world to increase the incidence of papillomavirus infection (PVI) caused by the HPV. Despite the existing treatment methods, the problem of PVI resistance to ongoing therapy is relevant. Squamous intraepithelial lesions of the cervix occupy a leading position in the structure of gynecological pathology among women of reproductive age. HPV plays a major role in the development of cervical squamous intraepithelial lesions. According to the literature, the peak of HPV infection occurs at the age of 15 to 30 years and is 18.6%, after 30 years, infection with human papillomavirus decreases (9.9%), while the frequency of detection of SIL and cervical cancer increases [1,4].The literature data confirm that recurrent warts serve as a classic marker of immunodeficiency, and according to many scientists, there is no doubt that the risk of PVI incidence is associated with the failure of cell-mediated immunity [3,6].The purpose of the research is the study of diagnostic markers of papillomavirus-associated cervical diseases in women of fertile age.
2. Materials and Methods of Research
135 women were examined. Of these:- 45-patients had papillomavirus-associated cervical diseases (group 1),- 45-women with papillomavirus-associated cervical diseases with transformation into oncopathology (group 2),- 45 healthy women of fertile age (without the presence of oncogenic HPV types, clinical, cytological and colposcopic changes in the cervix), (group 3).The average age of women in the 1st group was 33.9±1.3 years, in the 2nd group-44.1± 1.42 years and in the 3rd group-38.9±1.10 years.All of them underwent general laboratory, biochemical, immunological, virological, colposcopic and functional studies.
3. Results and Discussion
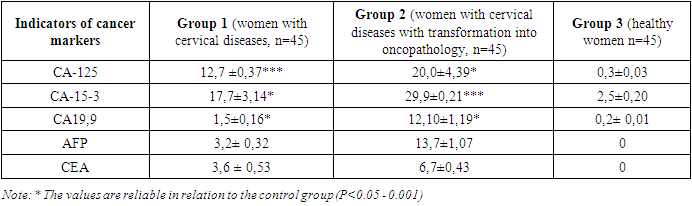
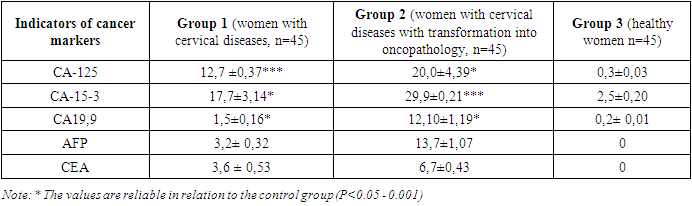
As a result, a statistically significant increase in the studied oncological blood markers was obtained in group 1 patients: CA-125 was increased 42.3 times, CA-15-3 marker was increased 7.1 times, CA-19.9 marker was increased 0.75 times against control values (P<0.05 - 0.001), (Table 1).Table 1. Indicators of oncological markers of blood in uterine leiomyoma
 |
| |
|
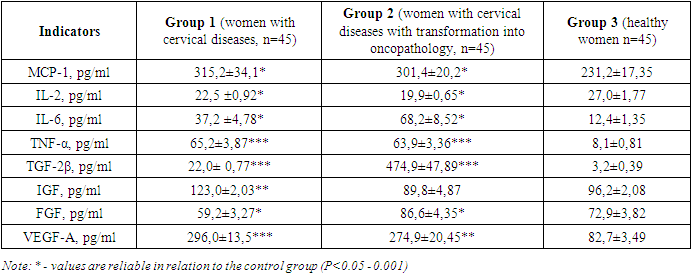
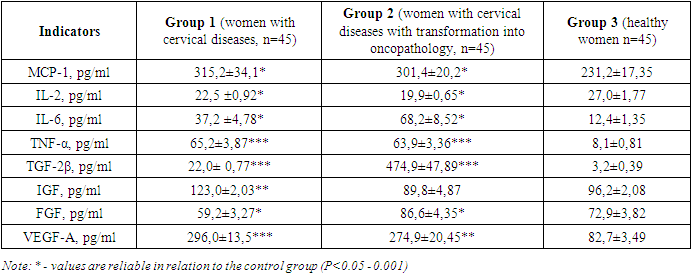
Currently, it is known that the cancer marker CA 125 (Carbohydrate antigen 125) is considered an oncomarker of ovarian cancer. Normally, its concentration is 4.0-8.8×109/l (0-30 IU/ml). When the index increases above 35 U /ml, ovarian cancer is detected in 90% of cases. An elevated level of CA 125, more than 30 IU/ml, may indicate such malignant diseases as cancer of the female genital organs (ovaries – in most cases, less often cancer of the endometrium (inner layer of the uterus), fallopian tubes, cancer of the respiratory organs (less specifically) and organs of the gastrointestinal tract, pancreas.In more rare cases, CA 125 is found in non-oncological processes, for example, with endometriosis, excessive growth of the inner layer of the uterus develops; with adhemomyosis, the inner layer of the uterus grows into muscle tissue; during menstruation and pregnancy; with inflammation of the female genital organs; inflammatory liver diseases. Taking into account the above, it is important to identify CA-125 in combination with other cancer markers.When studying cytokines in the blood serum of patients of the examined groups, an increase in MCP-1, IL-6, TNF-α, TGF-2β and VEGF-A was found in patients with PVAC of the 1st and 2nd groups (Table 2).Table 2. Indicators of cytokine status and markers of inflammation
 |
| |
|
One of the main chemokines for monocytes/macrophages and activated T lymphocytes is monocytic chemotactic protein-1 (MCP-1). MCP-1 was first identified as a product of secretion of monocytic leukemic cells stimulated by lipopolysaccharide, as well as peripheral blood mononuclear cells. MCP-1 belongs to the class of CC chemokines and is a potent chemoattractant of monocytes/macrophages. MCP-1 is not only a chemoattractant that ensures the migration and extravasation of mononuclear cells into the focus of inflammation, but also a mediator of inflammation, activating resident cells at the same time. Human MCP-1 is a protein consisting of 76 amino acids. MCP-1 is produced by many cell types, including mononuclear cells, mast cells, T cells, osteoblasts, fibroblasts, endothelial cells, bone marrow cells, epithelial cells, astrocytes. The synthesis of MCP-1 is induced by IL-1β, α-TNF, γ-INF, IL-6, IL-4. Under the influence of MCP-1, proliferation of vascular smooth muscle cells also occurs with their secretion of proinflammatory cytokines, which contribute to the progression of the disease due to vascular damage. Taking into account the above facts, the assessment of the chemotaxis process in patients selected for the study showed an increase in the level of MCP-1 in patients of group 1 by 1.36 times (315.2±34.1 pg/ml), by 1.3 times in patients of group 2 (301.4±20.2 pg/ml) compared to the control- 231.2±17.35 pg/ml, which confirms the presence of an acute inflammatory process and activation of macrophages. The obtained result indicates activation and/or exacerbation of chronic cervical pathology.There is an increase in the level of IL-6 in group 2 patients by 5.5 times, TNF-a by 7.8 times, an increase in the concentration of TGF-β2 in the blood by 148.4 times, an increase in VEGF by 3.32 times, and there is also a tendency to decrease IGF levels to 89.8±4.87 pg/ml, against control-96.2±2.08 pg/ml.The result obtained allows us to conclude that, in HPV-associated cervical diseases in women with transformation into oncopathology, there is a high increase in the concentration of growth factors that regulate the processes of angiogenesis and hematopoiesis. As a result of apoptosis and cell death, the cervical tissue disintegrates and destructurizes, which is confirmed paraclinically by the level of TNF-α in the blood serum. Studies have shown an increase in its level in patients of both groups: to 65.2±3.87 pg/ml in group 1, and in group 2 to 63.9±3.36 pg/ml versus control-8.1±0.81 pg/ml (p<0.001). The results obtained obviously prove the disintegration of tissue at the level of cervical tissue with transformation into cervical cancer.In our studies in patients of reproductive age, an increase in the concentration of TGF-β2 in the blood was found to 22.0± 0.77 pkg/ml in patients of group 1, to 474.9±47.89 pkg/ml in patients of group 2, against the control -3.2±0.39 pkg/ml (P <0.001).TGF β has been proven to block the activation of lymphocytes and macrophages, as well as initiate apoptosis in most cell types. Consequently, TGF β causes cell apoptosis. Judging by the level of TGF-β2 in the blood, it is possible to predict the state of the body's immune response. The analysis of IGF levels showed a decrease of 1.23 times in patients of group 1 (123.0±2.03 ng/ml), and a tendency to decrease it to 89.8±4.87 ng/ml in patients of group 2, compared with the values of the control group-96.2±2.08 ng/ml (P <0.01).Consequently, the result obtained in the interpretation of the analysis of an increase in the concentration of IGF-I in cervical diseases in group 1 women can be considered as a fact of the growth of reparative protective mechanisms for the restoration of the vascular wall.Analysis of FGF serum levels in women with HPV-associated cervical diseases showed a decrease to 59.2±3.27 pkg/ml in group 1 women and an increase to 86.6±4.35 pkg/ml against the control group - 72.9±3.82 pkg/ml (P <0.05). In the study, we found a tendency to increase VEGF-A to 296.0±13.5pg/ml in patients of group 1 and to 274.9±20.45pg/ml in patients of group 2 in relation to the indicators of the control group-82.7±3.49 pg/ml. Consequently, in HPV-associated cervical diseases, activation of chemotaxis with the participation of endothelial growth factor is noted.This leads to the conclusion that for the diagnosis and prognosis of HPV-associated cervical diseases in women, it is necessary to study the complex of cytokines, growth and damage factors and cancer markers in dynamics.
4. Conclusions
1. In papillomavirus-associated cervical diseases in women of reproductive age, CA-125 increased 42.3 times, CA-15-3 marker increased 7.1 times, CA-19.9 increased 0.75 times.2. An increase in MCP-1, IL-6, TNF-α, TGF-2β and VEGF-A was found in women with papillomavirus-associated cervical diseases.3. In papillomavirus-associated cervical diseases in women with transformation into oncopathology, there is a high increase in the concentration of growth factors that regulate the processes of angiogenesis and hematopoiesis. At the same time, against the background of a decrease in the protective reparative processes of vascular wall restoration, there is a high risk of stimulation of growth and proliferation of cervical tissue.
References
| [1] | Biswas S., Criswell T., Wang C. Inhibition of transforming growth factor-B signaling in human cancer: targeting a tumor suppressor network as a therapeutic strategy. Clin. Cancer Res. 2016; 12 (14): 4142–4146. |
| [2] | Bosch F.X. Human papillomavirus: science and technologies for the elimination of cervical cancer. Expert Opin Pharmacother. 2019; 12(14): 2189–2204. DOI: 10.1517/14656566.2011.596527. |
| [3] | Ciarmela P., Islam Md. S., Reis F.M., Gray P. C., Bloise E., Petraglia F., Vale W., Castellucci M. Growth factors and myometrium: biological effects in uterine fibroid and possible clinical implications. Hum. Reprod. Update, 2015, Vol. 17, no. 6, pp. 772-790. |
| [4] | Consuegra-Sanchez L. Prognostic value of circulating pregnancy-associated plasma protein-A and proform of eosinophil major basic protein levels in patients with chronic stable angina pectoris. Clin Chim Acta 2018; 391: 18-23. |
| [5] | Dolscheid-Pommerich R.C., Manekeller S., Walgenbach-Brunagel G., Kalff J.C., Hartmann G., Wagner B.S. and Holdenrieder S. Clinical Performance of CEA, CA19-9, CA15-3, CA125 and AFP in Gastrointestinal Cancer Using LOCI™-based Assays. Anticancer Research. 2017. vol. 37. P. 353-360. |
| [6] | Feng Y., Li Y., Dai W., Mo S., Li Q., Cai S. Clinicopathologic Features and Prognostic Factors in Alpha-Fetoprotein-Producing Colorectal Cancer: Analysis of 78 Cases. Cellular Physiology and Biochemistry. Cellular Physiology and Biochemistry. 2018. vol. 51. P. 2052–2064. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML