-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 686-692
doi:10.5923/j.ajmms.20241403.32
Received: Feb. 15, 2024; Accepted: Mar. 2, 2024; Published: Mar. 9, 2024

Efficacy of Anesthesia for Cesarean Section in Pregnant Women with Community-Acquired Pneumonia and First-Degree Respiratory Failure
Akramov B. R., Matlubov M. M., Xolbekov B. K., Sharipov I. L.
Department of Anesthesiology and Reanimation, Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Akramov B. R., Department of Anesthesiology and Reanimation, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study investigates the optimization of anaesthesia strategies for pregnant women with community-acquired pneumonia (CAP) and first-degree respiratory failure undergoing abdominal delivery. Three subgroups were analyzed based on the anesthetic technique: spinal anaesthesia (SA), epidural anaesthesia (EA), and balanced epidural anaesthesia (BEA), all combined with non-invasive ventilation. The study assessed the efficacy of anaesthesia through clinical signs, hemodynamic, stress indices, and the degree of sensory and motor blockade. Results indicated that SA was associated with a more pronounced decrease in blood pressure and a higher level of segmental blockade, while BEA provided a more stable hemodynamic profile with a pronounced sedative effect. The study also revealed that initial preoperative values of central and peripheral hemodynamic were within the hypokinetic mode of blood circulation. The SA subgroup experienced more pronounced hemodynamic disturbances, especially before skin incision and during the most traumatic stages of the operation. The BEA subgroup showed minimal hemodynamic disturbances and better stability in hemodynamic parameters throughout the operation. The findings underscore the importance of careful selection and monitoring of anaesthesia techniques in this patient population to ensure optimal outcomes.
Keywords: Anaesthesia, Caesarean Section, Community-Acquired Pneumonia, Pregnant Women, Respiratory Failure, Spinal Anaesthesia, Epidural Anaesthesia, Balanced Epidural Anaesthesia, Non-Invasive Ventilation
Cite this paper: Akramov B. R., Matlubov M. M., Xolbekov B. K., Sharipov I. L., Efficacy of Anesthesia for Cesarean Section in Pregnant Women with Community-Acquired Pneumonia and First-Degree Respiratory Failure, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 686-692. doi: 10.5923/j.ajmms.20241403.32.
1. Introduction
- Pneumonia has been a significant public health concern for over a century, with its incidence and mortality rates showing a marked decrease since the early 20th century due to advances in medical science and public health measures. However, the World Health Organization (WHO) highlights that pneumonia continues to be a pressing issue, particularly among vulnerable populations, including pregnant women [1-4].Pregnancy is a unique physiological state that increases susceptibility to viral respiratory infections due to alterations in the immune and cardiovascular systems [5-10]. These changes can lead to a higher likelihood of developing severe respiratory viral infections in pregnant women [11,12]. The 2019-2021 pandemic of the novel coronavirus (COVID-19) brought this vulnerability into sharp focus, as the incidence of COVID-19 in pregnant women was higher than that in the general population. Pregnant women infected with SARS-CoV-2, the virus responsible for COVID-19, are at an increased risk of severe disease progression. Numerous studies have reported adverse pregnancy outcomes in COVID-19 patients, with mortality rates among pregnant women infected with SARS-CoV-2 reported to be as high as 25% [13,12].The progression of acute respiratory failure (ARF) in pregnant women with community-acquired pneumonia further complicates the clinical picture. ARF is characterized by pronounced functional disorders of the respiratory system and impaired gas exchange, which negatively impact both the respiratory and cardiovascular systems. The primary cause of ARF in pregnant women with community-acquired pneumonia is often related to ventilation-perfusion mismatches, continued blood flow in non-ventilated lung areas due to infiltration, and compression of the diaphragm by the pregnant uterus.Anesthesiological support for abdominal and vaginal delivery in pregnant women with community-acquired pneumonia presents a significant challenge in modern anesthesiology and obstetrics. This challenge is particularly acute in labouring women with severe forms of community-acquired pneumonia accompanied by respiratory failure. Additionally, complications arising from circulatory failure and severe extragenital diseases further complicate the situation. These women require an individualized approach to anaesthesia care, with the primary goal being the safety of delivery and the stability of essential life support systems throughout labor and the immediate postpartum (or postoperative) period. A comprehensive prenatal assessment of the degree of respiratory insufficiency and the severity of community-acquired pneumonia is crucial for the successful management of these cases.Addressing the complex interplay of factors that contribute to the increased risk of pneumonia in pregnant women requires a multidisciplinary approach. This includes not only advancements in medical treatment and anesthesiological techniques but also a focus on preventive measures, early detection, and tailored management strategies to ensure the health and safety of both the mother and the fetus.The primary aim of this study is to optimize anesthetic strategies for pregnant women with community-acquired pneumonia (CAP) and first-degree respiratory failure undergoing abdominal delivery. This involves developing an evidence-based approach to anaesthesia that minimizes risks, enhances maternal and fetal outcomes, and ensures the stability of vital functions throughout the perioperative period.
2. Materials and Methods
- This prospective study aimed to evaluate the efficacy of different anesthetic techniques in pregnant women with CAP and first-degree respiratory failure undergoing abdominal delivery. The study was conducted from 2018 to 2023 and included 86 pregnant women with a mean age range of 21 to 45 years and a gestational age of 32-41 weeks. All patients were admitted for emergency or planned abdominal delivery, with the timing and method of delivery determined individually based on the clinical condition of the women, gestational age, and fetal condition.The participants were treated at the obstetric department of the multidisciplinary clinic of Samarkand State Medical University (SamSMU), the regional perinatal center, and the city maternity complex №3 of Samarkand. The choice of anesthetic method during surgical delivery was made with careful consideration of the severity of CAP and the degree of respiratory failure. The patients were divided into three subgroups based on the anesthetic technique used:First Subgroup (n=34): Women who underwent spinal anaesthesia (SA) and non-invasive ventilation (NIV) with positive end-expiratory pressure (PEEP) and a fractional inspired oxygen (FiO2) of 60-100%.Second Subgroup (n=28): Women who underwent epidural anaesthesia (EA) and NIV with positive PEEP and FiO2 of 60-100%.Third Subgroup (n=24): Women who underwent balanced epidural anaesthesia (BEA) and NIV with positive PEEP and FiO2 of 60-100%.Blood loss during abdominal delivery ranged from approximately 350 mL to 800 mL. The study adhered to the National Clinical Protocol "Management and Delivery of Pregnant Women with Pneumonia" (2021) approved by the Ministry of Health of the Republic of Uzbekistan and intensive care protocols for COVID-19. The anesthetic tactics for pregnant women with increasing signs of respiratory failure were individualized and determined by a consilium of physicians. The choice of combined anaesthesia with NIV and positive PEEP was based on continuous monitoring of maternal SpO2 (≥ 94%) and fetal condition (cardiotocography) in the absence of contraindications to central neuraxial blockade (CNB).The efficacy of anesthesia was assessed based on clinical signs, hemodynamics, stress indices, and the degree of sensory and motor blockade. Hemodynamic parameters were studied using echocardiography and monitored with a Scillar monitor. The stress index (SI) was evaluated using mathematical analysis of heart rhythm, total cortisol levels in blood plasma, and the rate of excretion of noradrenaline in urine. The study was conducted in four stages: on the operating table, before the skin incision, during the traumatic stage of the operation, and at the end of the operation.All numerical values obtained during the study were processed using the method of variation statistics. The statistical analysis was performed using Student's t-test with the assistance of the Microsoft Excel program. The results are presented as the mean (M) ± standard error (m), where M represents the arithmetic mean and m represents the standard error of the mean.Differences between groups and within groups at different stages of the study were considered statistically significant at a p-value of less than 0.05 (P < 0.05). The statistical analysis aimed to evaluate the differences in hemodynamic parameters, stress indices, and other relevant measures across the different subgroups and at various stages of the study.
3. Results
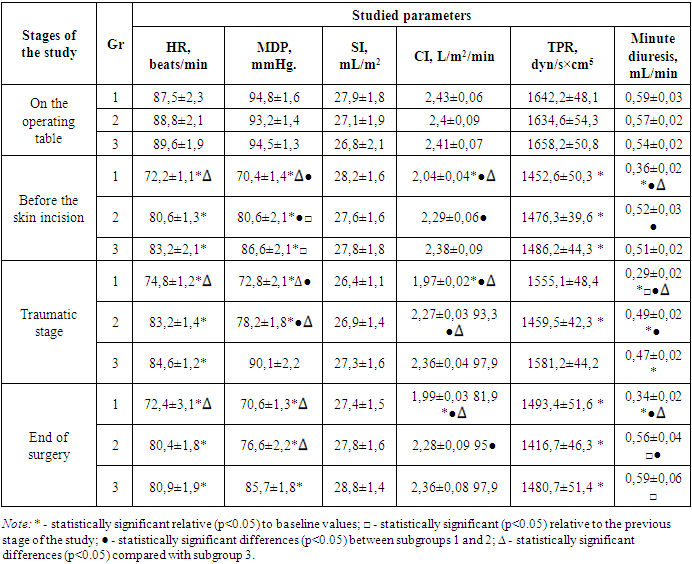
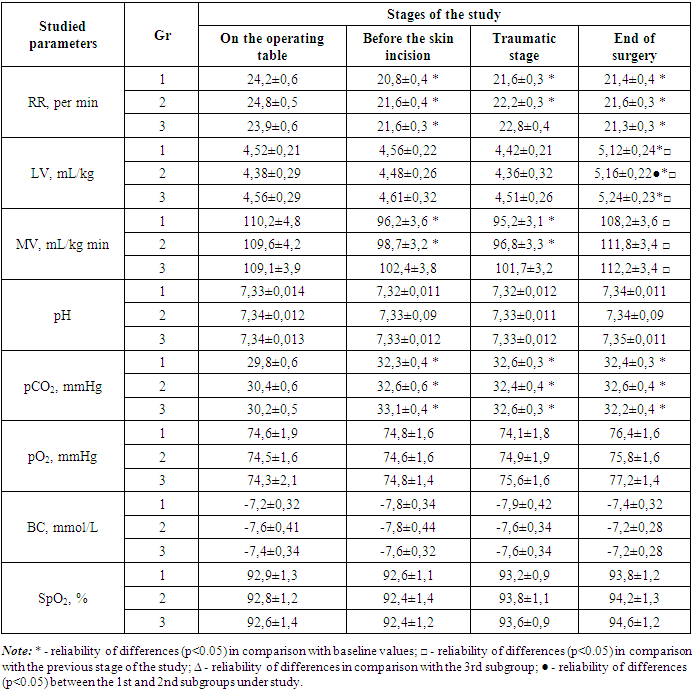
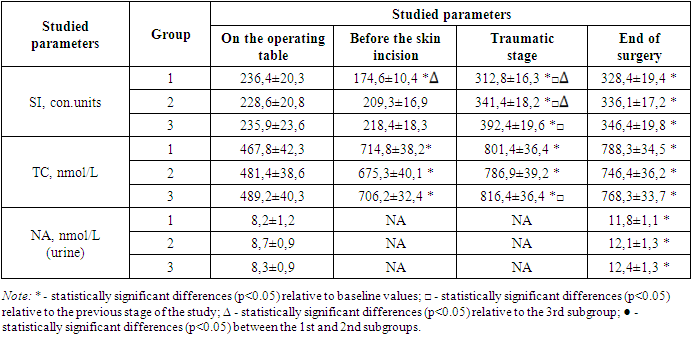
- Clinical Course of AnesthesiaThe clinical course of SA with 0.5% hyperbaric bupivacaine solution and NIV in CPAP mode was observed in pregnant women with CAP and first-degree respiratory failure. The classical signs of complete segmental sensory-motor blockade were formed within 8-10 minutes post-administration, with the level of distribution reaching beyond T6-T7 dermatomes to T4-T5. This elevated distribution level was attributed to the increased intra-abdominal pressure from the pregnant uterus, dyspnea, and respiratory insufficiency. An early and pronounced decrease in BP was noted, necessitating vasopressor support in some cases. However, the timely administration of minimal doses of mesaton allowed for rapid stabilization of arterial hypotension.The clinical course of EA with 0.5% bupivacaine solution was similar in terms of the time required for the development of complete segmental sensory-motor blockade and its level of distribution. However, the degree of BP decrease at the time of EA surgical stage development was more pronounced, requiring intraoperative vasopressor support in some cases. Despite this, BP remained stable throughout the subsequent stages of surgery, with no further correction needed. Postoperative epidural analgesia provided adequate pain relief, early activation, and rapid recovery of motor function and gastrointestinal tract evacuation.BEA with 0.375% bupivacaine solution and continuous infusion of propofol or dexmedetomidine resulted in a pronounced sedative effect within 8-10 minutes post-administration. Clinical signs of segmental sensory-motor blockade began to form, reaching their maximum by the 15th minute, with the surgical stage lasting 1.5-2.0 hours. The administration of sedatives induced drowsiness, indifference to surroundings, and good adaptation to NIV. Blood pressure remained stable throughout the operation, with a slight decrease in heart rate observed. No clinical signs of hypoxia or hypercapnia were detected. At the end of the operation, all patients were alert, responsive, and free from pain for 5-6 hours.In summary, the clinical course of anesthesia in pregnant women with CAP and first-degree respiratory failure varied depending on the type of anesthesia used. SA was associated with a more pronounced decrease in BP and a higher level of segmental blockade, while BEA provided a more stable hemodynamic profile with a pronounced sedative effect.Hemodynamic and Peripheral Circulation ParametersThe study revealed that the initial preoperative values characterizing central and peripheral hemodynamics in all three subgroups were within the hypokinetic mode of blood circulation (table 1). This was characterized by moderately pronounced tachycardia, decreased single and minute cardiac output, elevated mean dynamic pressure (MDP) and total peripheral vascular resistance (TPR), and reduced minute diuresis, fitting into the concept of "oliguria."
|
|
|
4. Conclusions
- The study explored the clinical course of SA, EA, and balanced epidural anesthesia (BEA) in pregnant women with CAP and first-degree respiratory failure. The findings reveal that SA was characterized by a rapid onset of complete segmental sensory-motor blockade, extending to higher dermatomes (T4-T5) due to factors such as increased intra-abdominal pressure and respiratory insufficiency. In contrast, EA and BEA exhibited similar onset times but differed in terms of blood pressure reduction and hemodynamic stability, with BEA providing the most stable profile throughout the operation.Hemodynamic and peripheral circulation parameters indicated a significant decrease in MDP and TRP before skin incision across all subgroups, with the most pronounced changes observed in the SA subgroup. The study further demonstrated that BEA offered the most stable hemodynamic profile throughout the surgical procedure.Respiratory function and gas exchange were adequately maintained in all subgroups despite the presence of CAP and acute respiratory failure, with an improvement in respiratory parameters noted at the end of the surgery. The study highlighted that different variants of CNB have distinct impacts on hemodynamics, respiratory function, and autonomic system parameters in this patient population.The autonomic system parameters showed a significant decrease in the SI in the SA subgroup, indicating a reduction in sympathetic influences. Additionally, an increase in total plasma cortisol and noradrenaline excretion was observed in all subgroups, reflecting the activation of the sympathoadrenal system in response to surgical trauma and hypoxia.In conclusion, the study underscores the importance of careful selection and monitoring of anesthesia techniques in pregnant women with CAP undergoing surgery to ensure optimal outcomes. The distinct impacts of different CNB variants on hemodynamic stability, respiratory function, and autonomic system responses highlight the need for further research to validate these results and explore their implications for clinical practice.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML