-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 682-685
doi:10.5923/j.ajmms.20241403.31
Received: Feb. 13, 2024; Accepted: Feb. 28, 2024; Published: Mar. 9, 2024

Factors Provoking Severe Behcet's Disease in Adolescent Patients
Munisa A. Mirsaidova, Khilola Kh. Fayziyeva
Republican Specialized Scientific and Practical Medical Center for Dermatovenereology and Cosmetology, Tashkent, Uzbekistan
Correspondence to: Munisa A. Mirsaidova, Republican Specialized Scientific and Practical Medical Center for Dermatovenereology and Cosmetology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Our study aimed to conduct a comparative analysis of factors leading to further aggravation of Behcet's disease in patients of adolescence and young adulthood. Methods: We examined and treated eight pre-adolescent and young adults diagnosed with Behçet's disease. Simultaneously with clinical and anamnestic observation, a thorough examination of the mucous membranes of the urogenital tract was carried out for the presence of urogenital infections of a bacterial-viral nature, a study of autoimmune antibodies (Anti-double-stranded DNA, IgG, and Anti-single-stranded DNA, IgG) in the blood serum of patients, consultations with related specialists. Results: It has been established that among the features of the clinical course of Behcet's disease in adolescents and young adults, the prevailing symptoms are aphthous stomatitis, erosive and ulcerative lesions of the oral mucosa, and eye lesions. Among infections of the genital mucosa, herpesvirus, papillomavirus, ureaplasma, and candidiasis, infections are detected with increased frequency. A 1.5-fold increase in the content of autoimmune antibodies (Anti-double-stranded DNA, IgG and Anti-single-stranded DNA, IgG) was noted, which indicates the beginning of the formation of an autoimmune component in the development of the disease. Conclusion: Incorporating appropriate antiviral and antibacterial drugs into therapy significantly speeds up the recovery time and lengthens the intervals between relapses.
Keywords: Behçet's disease, Causative factors, Adolescents and young adults
Cite this paper: Munisa A. Mirsaidova, Khilola Kh. Fayziyeva, Factors Provoking Severe Behcet's Disease in Adolescent Patients, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 682-685. doi: 10.5923/j.ajmms.20241403.31.
1. Introduction
- Behcet's disease is a multisystem recurrent chronic vasculitis of unknown etiology, accompanied by damage to the mucous membranes, which explains the variety of clinical symptoms: recurrent erosive and ulcerative lesions of the mucous membrane of the mouth and genital organs, involvement of the joints, central nervous system, and gastrointestinal organs in the pathological process. The disease is widespread but is more common in the countries of the ancient Silk Road. [2,6]. There are some differences in the clinical characteristics of the disease between ethnic groups living in different geographical regions. If the prevalence of Behcet's disease in Turkey is very high and ranges from 80/100,000, then in the USA, the disease is quite rare, amounting to 1/300,000 [2]. Both men and women are susceptible to the disease. But in different geographical locations of the world, the prevalence of the disease in representatives of one or the other sex has been described. That is, a higher prevalence of Behçet's disease occurs in adult women in Korea [4], Israel [6], and Singapore [8], while BD in men more often observed in the West Indies [2], Spain [9], Japan [10], Jordan [1], Iran and Turkey [7]. Recent studies have shown that the male gender and early onset of the disease are associated with more severe manifestations of Behçet's disease, for example, vascular damage (thrombosis, etc.), eyes, gastrointestinal tract, and central nervous system [1,3].The peak onset of Behçet's disease usually occurs in the third decade of life [30], although the diagnosis is finally verified more often in the fourth decade of life [5,8].Behçet's disease is less common in children, even in high-risk countries.There are few epidemiological studies on Behçet's disease. In the work of Albuquerque P. et al. [2] stated that the prevalence of Behçet's disease in children is 1:20,000. Most data are based on retrospective analysis. Among patients with Behçet's disease (meeting the International Behçet's Disease Study Group criteria [10]), approximately 2–3% are under 16 years of age. However, it should be noted that in a significant number of adult patients, the first symptoms of the disease appear in childhood, but only years later the full type of the disease develops. This, of course, is of great importance for the prognosis of the disease, since there are reports that adult patients whose first symptoms of the disease appeared at a young age have a worse prognosis than patients with onset of the disease after 40 years of age [7]. The influence of age on the course and prognosis of the disease still remains one of the pressing problems in the study of BD.The multisystem nature of clinical manifestations, relatively rare occurrence, especially in childhood, low identification of the disease in adolescence, determines the difficulty of early verification of the disease. Diagnosis of Behçet's disease is based on a set of classification signs/symptoms, the formation of which takes 5–8 or more years. The diagnosis of Behçet's disease is especially difficult in cases where ocular or skin symptoms present as an isolated or predominant manifestation of the disease, and they are often mistakenly regarded as common dermatoses or separate eye diseases. The absence of a leading etiological agent in the development of Behçet's disease leads to a lack of clarity in matters of therapy and a long, progressive, relapsing course of the process, with the subsequent development of serious complications in adolescents.Purpose (purpose)Characteristics of factors leading to a more severe course of Behcet's disease in adolescents and young adults.
2. Patients and Methods
- The work is based on clinical, anamnestic and laboratory observation of 8 patients of adolescence and youth with various clinical manifestations of Behcet's disease, who were examined in the department of sexually transmitted infections and reproductive disorders of the Republican Specialized Scientific and Practical Medical Center of Dermatovenerology and Cosmetology of the Republic of Uzbekistan from 2021 to 2023 Their age ranged from 15 to 18 years. Before starting treatment, all patients, with their voluntary consent and, if necessary, the consent of their parents, underwent the following research methods: clinical and laboratory examination of patients, including bacteriological examination of genitourinary tract discharge, polymerase chain reaction for diagnosing infections of the urogenital tract, immunological studies for the presence of autoimmune antibodies (Anti-double-stranded DNA, IgG and Anti-single-stranded DNA, IgG), histological examination of material from lesions, as well as consultation of related specialists.
3. Results and Discussion
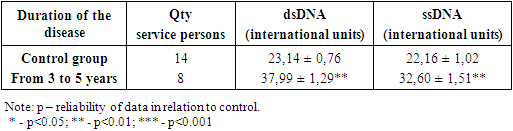
- The time interval from the onset of the disease to admission to the Center’s clinic and establishment of a clinical diagnosis ranged from 3 to 5 years. In all patients, the primary symptom was most often aphthous stomatitis and accompanying fever. Of the 8 patients, 6 had erosive and ulcerative lesions of the genitals within 2 years after the onset of aphthous stomatitis. 3 patients had skin manifestations in the form of papulopustular rashes, 4 patients had erythema nodosum, and 1 patient had a combination of erythema nodosum and acne-like rash. Subsequently, other organs and systems were involved in the pathological process. In the advanced stage of the disease, there was already a clinical symptom complex, including aphthous stomatitis, ulcerative process on the genitals, damage to the skin, eyes, gastrointestinal tract and, less often, the central nervous system in the form of headaches. Before contacting the clinic of our Center, almost all 100% of patients received various therapy for one or another symptom of the disease with a temporary effect or without effect. Previously, patients turned mainly to ophthalmologists, dentists, pediatricians, pediatric gynecologists, and rheumatologists. Among the prescribed drugs, corticosteroid hormones, vitamin therapy, and antibiotics predominated.When studying the factors that provoke a more severe course of Behçet's disease in adolescents and young adults, one can note, first of all, a burdened anamnesis: 6 patients on the mother's side had episodes of recurrent aphthous stomatitis and conjunctivitis, occurring with periodic exacerbations. Studies have shown that among the examined patients, the bacterioscopic method of examining discharge from the lesions revealed Candida albicans in 8 (100%) and Gardnerella vaginalis in 5 (62.5%). In addition, cultural diagnostics of discharge from lesions showed that other bacterial pathogens are also detected in patients with Behçet's disease. Thus, in 4 (50.0%) patients Staphylococcus epidermidis was cultured, in 3 (37.5%) - Enterobacter, in 2 (25.0%) - Streptococcus haemolyticus. A study of discharge from lesions using polymerase chain reaction showed that with this research method, 5 (62.5%) of the 8 people examined with Behçet's disease had a positive result for the presence of Ureaplasma Urealyticum. When examining blood serum during PCR diagnostics for the presence of viruses, it was revealed that in 8 patients with this pathology, herpes simplex virus type I (HSV I) was detected in 5 (62.5%) cases, in 1 (11.1%) Herpes simplex virus type II (HSV II) was detected in 2 patients (25.0%), cytomegalovirus (CMV) was detected in 2 (25.0%) and human papillomavirus (HPV) was detected in 2 (25.0%). Also in this group of patients, diseases of the genitourinary system were identified: urethritis in 8, vulvitis in 4, cystitis in 3 and pyelonephritis in one patient.In most patients, the simultaneous presence of three or more infectious agents was noted, which in turn was characterized by a more protracted course of the process in the form of often recurrent aphthae of the oral and pharyngeal mucosa and erosive and ulcerative lesions of the genitals. These studies indicate the important role of viral-microbial associations in the development of protracted clinical symptoms and long-term healing of pathological elements. Detection of cytomegalovirus infection, herpes simplex virus and human papillomavirus may also become a risk factor for malignant degeneration of erosions and ulcers in the future.A study was also carried out on the indicators of autoimmune antibodies of class G (Anti-double-stranded DNA, IgG and Anti-single-stranded DNA, IgG), since the diagnosis of these antibodies also leads to a more severe course of the disease, and early diagnosis allows the choice of the correct treatment tactics.Thus, in patients of the study group there was a statistically significant increase in the content of Anti-double-stranded DNA (37.99 ± 1.29 IU) and Anti-single-stranded DNA (32.60 ± 1.51 IU, p<0.01) compared with the data from the control group (23.14 ± 0.76 IU and 22.16 ± 1.02 IU, respectively).
|
4. Conclusions
- 1. Modern features of Behcet's disease in adolescents and young adults include the predominance of aphthous stomatitis, erosive and ulcerative lesions of the oral mucosa and eye damage. Among infections of the genital mucosa, herpesvirus, papillomavirus, ureaplasma and candidal infections are detected with increased frequency, which must be taken into account in the treatment of the disease.2. Studying the content of autoimmune antibodies (Anti-double-stranded DNA, IgG and Anti-single-stranded DNA, IgG) can become an early prognostic criterion for the development of the autoimmune component of the disease and the basis for appropriate immune-oriented therapy.3. Connection to therapy with drugs effective against herpes simplex viruses, human papillomavirus and accompanying microflora, which may have an impact on the severity, progression of the disease, and the severity of clinical manifestations, led to accelerated healing of erosive and ulcerative processes and a decrease in the number of relapses of the disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML