-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 657-662
doi:10.5923/j.ajmms.20241403.25
Received: Feb. 17, 2024; Accepted: Mar. 4, 2024; Published: Mar. 7, 2024

A New Method of Providing Aerostasis in Lung Surgery
Abdullajanov B. R., Isakov P. M.
Andijan State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Postoperative air leakage - alveolo-pleural fistula, is one of the most frequent and insidious complications in thoracic surgery and the main limiting factor in early discharge of patients from the hospital. The aim of this study was to increase the efficiency and reliability of aero- and hemostasis in traumatic or surgical damage to the lung parenchyma. In the proposed method, after performing the main stage of the operation, intraparenchymal puncturing with a gel substance is performed to achieve local aero- and hemostasis in the area of damaged or sutured lung tissue. The new technology of introducing a biological implant into the area of damaged lung parenchyma provides increased tightness of sutures, which is justified by a reduction in the frequency of postoperative significant air leakage from 5.6% to 0.8% and parenchymal bleeding from 4.9% to 0.8%.
Keywords: Aerostasis in lung surgery, Alveolo-pleural fistula, Postoperative complications, Lung surgery
Cite this paper: Abdullajanov B. R., Isakov P. M., A New Method of Providing Aerostasis in Lung Surgery, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 657-662. doi: 10.5923/j.ajmms.20241403.25.
Article Outline
1. The Relevance of the Problem
- Despite the frequency of aerostasis disorders, there is still no standard approach to the treatment of air leakage in lung surgery, including cases with prolonged discharge through the alveolo-pleural fistula [1,2].Due to the lack of a unified approach to the tactical aspects of the treatment of postoperative air leakage, most surgeons pay attention to intraoperative prevention [3,4].Choosing the best sealing agent is also a highly debatable issue. According to the consensus of thoracic surgeons, the "ideal sealant" should be safe, absorbable, have plasticity so that it can be applied to a partially inflated lung, ensure adequate adhesion to the surface of the lungs and its application should not take more than five minutes [5,6].Substances used in clinical practice for local strengthening of the damaged lung area are often characterized by insufficient effectiveness and unidirectional effects. Many of these coatings are made of biological materials (animal or plant origin), which causes their high antigenicity, as well as destruction during thermal sterilization.Some meta-analytical reviews have shown that further large-scale studies are needed to clearly determine the effect of surgical sealants on the results of prevention and treatment of air leakage, as well as the safety of their use, since some agents increase the risk of developing pleural cavity infection [7,8].Currently, there are no local hermetic agents in lung surgery that could be used intraparenchymatically in the area of tissue defect. Thus, the designated purpose of this study was to increase the efficiency and reliability of aero- and hemostasis in case of traumatic or surgical damage to the lung parenchyma.
2. Research Material and Methods
- The proposed method has no analogues, since the biological implant is not applied superficially on top of the damaged lung tissue, but is injected directly into the lung parenchyma in the area of damage. A total of 275 patients with various lung pathologies requiring surgical treatment were included in the study. All patients were divided into two groups. In the main group, 131 patients in 2022-2023 had a new method of sealing sutures after performing the main stage of lung surgery. The comparison group included 144 patients with lung pathology comparable to the main group, operated on from 2019 to 2021, in whom additional measures were taken during intraoperative verification to eliminate the insolvency of aero- and (or) hemostasis by traditional methods.More than 90% of patients in both groups were between the ages of 21 and 60, men in the groups were 52.8% and 55.7%, women 47.2% and 44.3%.The largest number of operations were performed for echinococcosis of the lungs, in the comparison group 60 (41.7%), in the main group 73 (55.7%). Next in number were patients with pulmonary bullous emphysema – 43 (29.9%) and 26 (19.8%) patients, respectively. Pancyric pleurisy was verified in 16 (11.1%) and 6 (4.6%) patients. In other cases, patients with focal lesions such as tuberculosis, hamartoma, fibrochondroma, lung abscess, cases of complicated residual cavities after echinococcectomy (EE) (hemoptysis, bronchial fistula, suppuration), as well as patients who underwent lobectomy for cystic hypoplasia of the lung lobe or bronchiectasis complicated by pneumofibrosis, were operated on.All cases of benign oncopathologies were confirmed after surgery by histological examination. According to the localization of the pathological process, the distribution was as follows: in the comparison group, pathology in the left lung was in 64 (44.4%) patients, in the right in 80 (55.6%), in the main group – 62 (47.3%) and 69 (52.7%) patients, respectively. The incidence of lobe lesions was approximately the same for the upper and lower lobes, while pathology was localized on the right in the middle lobe in only 3 (2.1%) and 4 (3.1%) patients, respectively.Taking into account the fact that the developed method can be used for both open and video thoracoscopy operations, these two types of intervention were included in the study groups and for a more objective analysis in the chapters with the results of their own research, the analysis was also distributed according to this factor. Open surgeries were performed in 93 (64.6%) patients in the comparison group and in 87 (66.4%) patients in the main group. Videothoracoscopy interventions were performed in 51 (35.4%) and 44 (33.6%) patients, respectively. Among the range of open operations, EE, excision and suturing of the lung bull(s), marginal resection, lobectomy were performed. During videothoracoscopy interventions, EE from the lungs, excision and suturing of the lung bull(s), marginal resection and lobectomy also took place.In the main group, seam sealing was performed according to the proposed method, which is characterized by the following technical features: the main stage of the operation is performed, then a gel is prepared - 1.0 g of Hemoben powder is mixed with 30 ml of saline solution with continuous stirring for 1 minute and immediately typed into a syringe with an injection needle with a diameter of 25-30 G. To achieve local aero- and hemostasis in damaged or sutured lung tissue, a needle injection is performed at a distance of 5 mm from the edge of the damaged lung parenchyma and then the needle is moved superficially at a depth of 5 mm at an angle of 30° from the periphery (injection site) towards the center of the wound surface, while 0.5-1.0 ml of Hemoben gel is injected. This procedure is repeated 3-4 times depending on the volume of the wound surface until the gel completely imbibes the entire wound defect (Fig. 1).
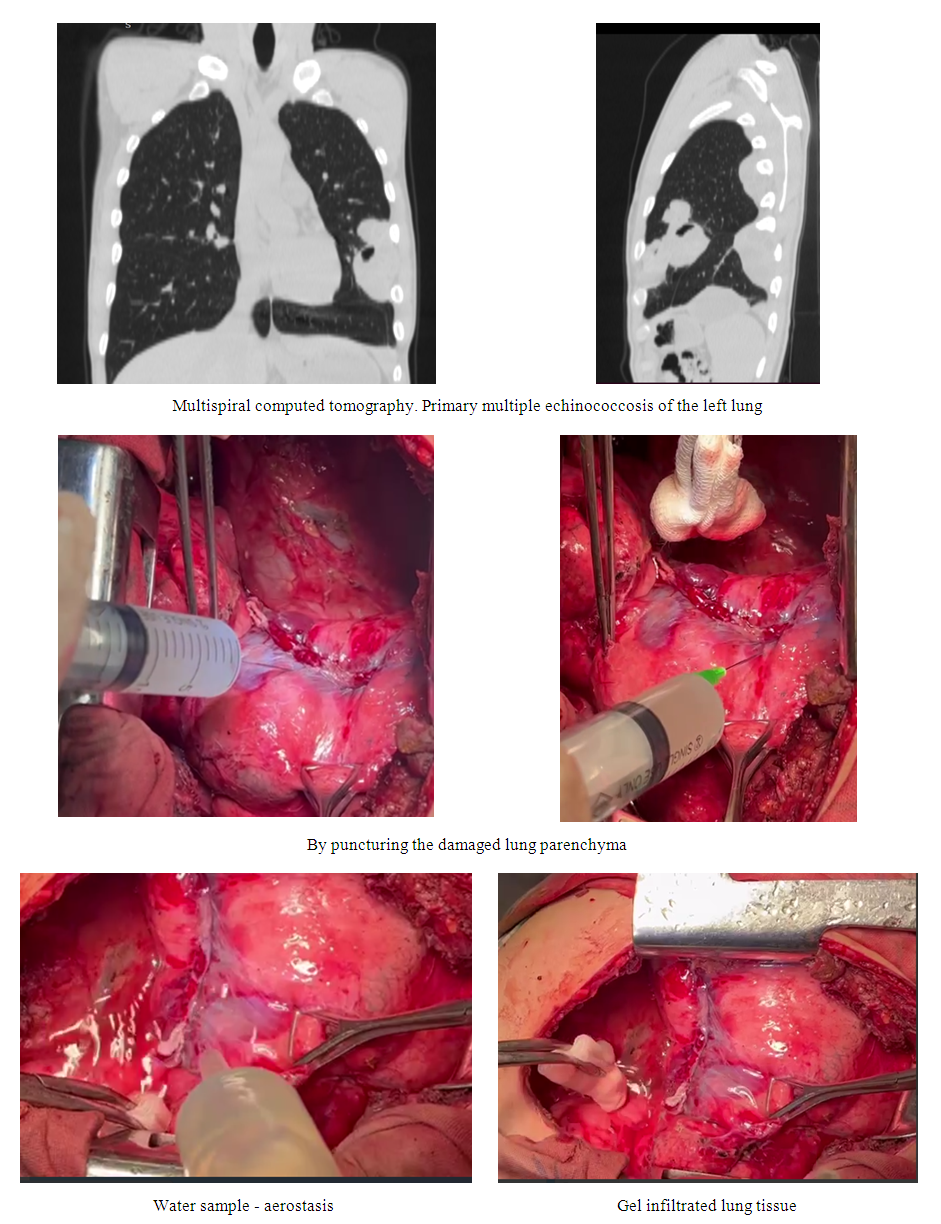 | Figure 1. Sealing of the hardware suture line after marginal resection of the lingual segments of the left lung using a new technique for the purpose of aero and hemostasis |
3. Results and Discussion
- In the early postoperative period, all variants of the manifestation of insolvency in aero- and hemostasis were taken into account. In our observations, we attributed cases when pneumorrhea stopped on its own during the first 3 days to a slight air discharge through drainage, and no additional measures were taken in these cases. Long-term air leakage included cases with a discharge of 5 days or more. In the compared groups, a slight leakage was noted in 14 (9.7%) in the comparison group and in 4 (3.1%) in the main group. Prolonged air leakage was detected in 8 (5.6%) and 1 (0.8%) patients, respectively.Another complication was the presence of hemorrhagic discharge through drains, and if the intensity of hemorrhage was insignificant (more intensely colored discharge with clots), then conservative hemostatic therapy and regular monitoring in dynamics were prescribed to these patients. The fact of intrapleural bleeding was characterized by intensive heme intake through drains, and with a volume of 100 ml or more per hour, patients underwent repeated video thoracoscopy intervention or thoracotomy. Minor hemorrhagic drainage discharge occurred in 7 (4.9%) patients of the comparison group and 1 (0.8%) in the main group. Bleeding in the early period developed in 3 (3.2%) and 1 (1.1%) patients, respectively. In the comparison group, there were 2 bleeds after open surgeries and 1 after videothoracoscopy of the operation, these patients underwent repeated intervention with rehabilitation and stopping of bleeding – videothoracoscopy and retoracotomy after open surgeries and revideothoracoscopy after minimally invasive intervention. In the main group, 1 patient with bleeding after open intervention underwent videothoracoscopy, rehabilitation with stopping bleeding from the trocar puncture area. The frequency of prolonged air leakage with subsequent development of pleural empyema in the comparison group was 3 (2.1%) cases, there were no such complications in the main group. Occluded pleurisy occurred in 4 (2.8%) and 1 (0.8%) patients.Depending on the type of operation, the following pattern is noted. The frequency of complicated course of the early postoperative period after open interventions in the comparison group was 20.4% (in 19 of 93 patients), in the main group – 5.7% (in 5 of 87 patients; -2=8,386; df=1; p=0.004). In their structure, insignificant air leakage was noted in 8 (8.6%) and 2 (2.3%) patients, respectively, prolonged air leakage – 4 (4.3%) and 0%.After videothoracoscopy operations, the frequency of complicated course of the early postoperative period in the comparison group was 23.5% (in 12 of 51 patients), in their structure half of the cases (11.8%) were due to minor air leakage, but the frequency of videothoracoscopy was slightly higher than in open operations – 7.8% (4 patients), which, apparently, this is due to the reset between the joints of the hardware seams. In the main group, the proportion of minor air leakage was 2.3% (in 2 out of 44 patients), videothoracoscopy in 1 (2.3%) patient. In total, there were 3 (6.8%) patients with complications in this group, which also significantly differed from the comparison group (χ2= 4,961; df=1; p=0.026).According to the classification of the severity of postoperative complications (Clavien-Dindo, 2004), in this study, the distribution was carried out according to the following type: complications from the wound, as well as minor pneumorrhea, were attributed to the first degree; to the second degree – all complications that did not require invasive interventions, but led to an elongation of the hospital period and the appointment of additional conservative measures (prolonged air leakage, empyema, minor hemorrhages); to the third degree – the need for minimally invasive interventions (IIIa) or repeated operations (IIIb); also in the comparison group, 1 patient had a grade V complication that led to a fatal outcome.The proportion of significant (II-V degree) complications in the comparison group was 13.2% (in 19 out of 144 patients), in the main group – 3.1% (4 out of 131 patients), respectively, 86.8% and 96.9% of patients were without these complications (χ2=9.205; df=1; p=0.003).After open surgeries, the overall incidence of significant complications was 13 (14%) cases in the comparison group and 3 (3.4%) patients in the main group (respectively, 86% and 96.6% were without these complications; -2=6,154; df=1; p=0.014).After videothoracoscopy of operations, the overall incidence of significant complications (grade II-V according to Clavien-Dindo) was 6 (11.8%) cases in the comparison group and 1 (2.3%) patient in the main group (respectively, 88.2% and 97.7% were without these complications). There was no significant difference in this subgroup due to the small sample of patients (χ2=3,118; df=1; p=0.078).The development of significant complications (grade II and higher according to Clavien-Dindo) required additional measures. In general, in the comparison group, complications were eliminated by conservative methods in 5 (3.5%) patients. Chemical pleurodesis for prolonged pneumonia was performed in 8 (5.6%) patients, the technique consisted in injecting an iodinol solution into the drainage for 20 minutes 1 time a day, up to 3 times a day. Minimally invasive treatment by percutaneous drainage of obstructed pleurisy was performed in 3 (2.1%), videothoracoscopy was performed in 2 (1.4%) cases and 1 (0.7%) retoracotomy was performed. In the main group, 4 patients underwent 1 case (0.8%) – conservative treatment, chemical pleurodesis, pleurisy drainage and videothoracoscopy rehabilitation.In the subgroups, after open interventions, conservative measures eliminated 5 (5.4%) complications in the comparison group and 1 (1.1%) in the main group. Chemical pleurodesis was performed in 4 (4.3%) in the comparison group, also in this group, 2 (2.2%) had drainage of obstructed pleurisy and in 1 (1.1%) case, video thoracoscopy of sanitation and retoracotomy, 80 (86%) patients were without significant complications. In the main group, drainage and videothoracoscopy were performed in 1 (1.1%) case, 84 (96.6%) patients were without significant complications.After videothoracoscopy of operations in the comparison group, chemical pleurodesis was performed in 4 (7.8%), drainage in 1 (2%) and eye in 1 (2%) patient, video thoracoscopy was performed, rehabilitation for bleeding, 45 (88.2%) patients were without significant complications. In the main group, only 1 (3.3%) patient underwent pleurodesis with iodinol, 43 (97.7%) patients were without significant complications.According to the course of the early postoperative period, different drainage periods were obtained in the study groups. Only 6 patients in the comparison group and 7 in the main group had one drainage into the pleural cavity. All other patients had 2 drains installed. Also, in the comparison group, 1 case of death was not taken into account in this analysis.The removal of the first drainage within 3 days after surgery in the comparison group was noted in 99 (68.8%) cases, in turn, during these periods, the removal of the second drainage was carried out in 40 (27.8%). On day 4-5, the first drainage was removed in 25 (17.4%), and the second drainage was removed in 64 (44.4%) patients during these periods. Further, in terms of 6-7 days, the first drainage was removed in 8 (5.6%), and in terms of more than 7 days in 11 (7.6%) patients. The second drainage was extracted on 6-7 days in 14 (9.7%) and later in 19 (13.2%), which was primarily due to the development of prolonged air leakage. In turn, in the main group, the first drainage was removed in 111 (84.7%) within 3 days after surgery, on 4-5 days in 16 more (12.2%), on 6-7 days in 3 (2.3%) and only one (0.8%) on day 9 (relative to the group comparisons χ2=12.766; df=3; p=0.006). The second drainage in the main group was removed up to 3 days in 51 (38.9%) patients, on 4-5 days in 66 (50.4%), on 6-7 days in 5 (3.8%) and in 2 (1.5%) patients on days 9 and 11 (relative to the comparison group χ2=18.785; df=3; p<0.001).The average drainage time in the comparison group was 5.0±2.1 days, in the main group – 3.8±1.4 days (t=4.63; p<0.05), while the first drainage was removed on average after 3.6±2.3 and 2.7±1.2 days (t=4.08; p<0.05), and the second after 5.1±2.5 and 3.9±1.4 days (t=4.69; p<0.05). The duration of the postoperative hospital period was 7.3±2.4 and 6.4±1.4 days (t=3.91; p<0.05) (Fig. 2). In the groups as a whole and in the videothoracoscopy subgroup of operations, the average drainage time slightly differed from the time of removal of the second drainage, since only 1 drainage was installed in 6 and 7 patients.
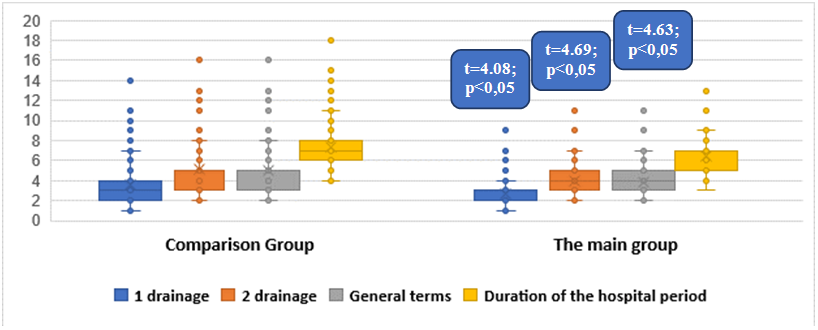 | Figure 2. Average duration of drainage and postoperative hospital period (day; M±σ) |
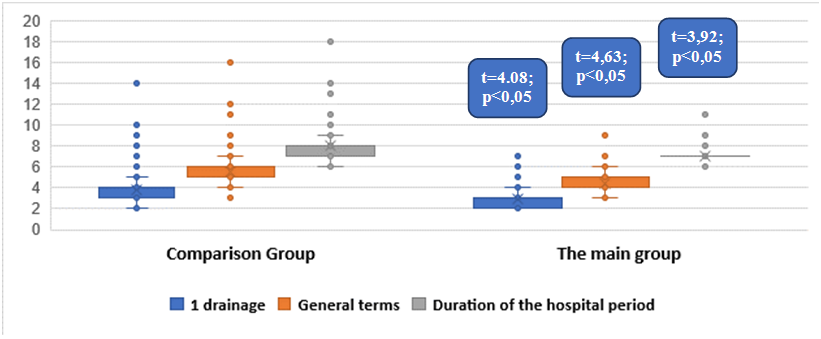 | Figure 3. Average duration of drainage and hospital stay after open surgeries (day; M±σ) |
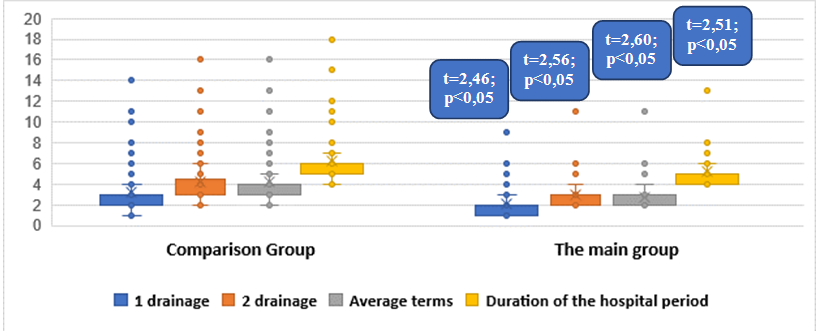 | Figure 4. Average duration of drainage and hospital period after videothoracoscopy of operations (day; M±σ) |
4. Conclusions
- The new technology of introducing a biological implant into the area of damaged lung parenchyma provides increased tightness of sutures, which is justified by a reduction in the frequency of postoperative significant air leakage from 5.6% to 0.8% and parenchymal bleeding from 4.9% to 0.8% (significant bleeding is usually not a consequence of parenchymal, but vascular genesis, the use of wound coatings in these situations is ineffective). At the same time, a significant advantage is a reduction in the risk of developing empyema against the background of aerostasis failure (2.1% in the comparison group), while the incidence of complications decreased from 21.5% to 6.1% (χ2=13.403; df=1; p<0.001).The introduction of a new technique for strengthening the tightness of sutures on the lungs allowed to reduce the overall incidence of early clinically significant postoperative complications (grade II-V according to Clavien-Dindo) in general groups from 13.2% to 3.1% (χ2=9.205; df=1; p=0.003), including open interventions – from 14% to 3.4% (χ2=6,154; df=1; p=0.014) and videothoracoscopy operations – from 11.8% to 2.3%, in turn, in the structure of these complications, severity II accounted for 9% in the comparison group and 1.5% in the main group, and grade III-V was 4.2% versus 1.5% (χ2=14.241; df=5; p<0.05), while it is the development of prolonged air leakage that is the main risk factor for the formation of menacing specific purulent-inflammatory complications.In the early period after surgical treatment of focal lung pathology, especially after resection interventions, the development of aero- and (or) hemostasis failure are the main factors of prolonged postoperative rehabilitation, while the probability of their elimination by conservative measures was only 3.5%, chemical pleurodesis was performed in 5.6% (out of 13.2% of complications in the comparison group), In the remaining (4.2%) cases, it became necessary to carry out invasive methods, including drainage (2.1%), videothoracoscopy, sanitation (1.4%) and retoracotomy (0.7%). In turn, the use of a new sealing method made it possible to change both the frequency of these complications and the need for additional therapeutic manipulations (3.1%), which were limited to conservative measures, pleurodesis, drainage or video thoracoscopy intervention.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML