-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 610-615
doi:10.5923/j.ajmms.20241403.15
Received: Feb. 5, 2024; Accepted: Feb. 28, 2024; Published: Mar. 6, 2024

Analysis of Myocardial Structure Changes in Patients with Progressive Arterial Hypertension and Type 2 Diabetes
Tashkenbaeva Eleonora Negmatovna, Ellamonov Sukhrob Numanovich, Abdieva Gulnora Alievna
Department of Internal Diseases and Cardiology No2 of Samarkand State Medical University, Samarkand, Uzbekistan
Correspondence to: Ellamonov Sukhrob Numanovich, Abdieva Gulnora Alievna, Department of Internal Diseases and Cardiology No2 of Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

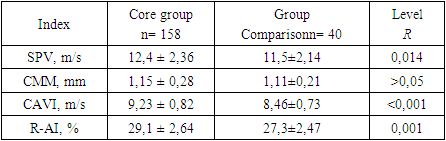
The study of structural and functional changes in the left ventricular (LV) myocardium in patients with diabetes mellitus is associated with the fact that, being in conditions of constant hyperglycemia, metabolic disorders occur in the myocardium, due to which there is a deterioration of systolic and diastolic function. Therefore, these patients with DM require increased attention and alertness in terms of the early development of life-threatening arrhythmias, sudden death and more rapid progression, and decompensation of chronic heart failure (CHF). Regardless of whether CHD and CHF are complications of DM or a competing pathology developing in parallel with carbohydrate metabolism disorders, such patients represent one of the highest risk categories associated with increased mortality. Objective to assess the structural remodeling of the myocardium in patients with advanced hypertension and type 2 diabetes. The object of the studywas The study included 198 patients with hypertension (mean age 57.6±5.48 years, 105 men and 93 women). All patients underwent clinical and laboratory examination, which included screening laboratory tests (clinical blood count, complete urinalysis, plasma creatinine with GFR calculation (calculated using the CKD-EPI formula), lipid profile, plasma glucose level), glycated hemoglobin, and 12-lead electrocardiogram. Body mass index was determined. All patients underwent echocardiography. In patients with hypertension and type 2 diabetes, in comparison with patients without diabetes, not only a higher level of blood pressure (SBP – by 5.6 mm Hg and DBP – by 4.7 mm Hg), but also the most significant increase in arterial vascular stiffness parameters was recorded: PWV – by 0.9 m/s, CAVI – by 0.77 m/s, and R-AI – by 1.8%; (p<0.05). Reduction of arterial vascular wall stiffness and myocardial diastolic dysfunction under the influence of mexidol can serve as a basis for the use of cytoprotective drugs in order to reduce the incidence of cardiovascular events (MI, stroke) in the treatment of patients with hypertension against the background of type 2 diabetes.
Keywords: Myocardial structure, Progressive arterial hypertension, Type 2 diabetes, Blood pressure, Comorbidity
Cite this paper: Tashkenbaeva Eleonora Negmatovna, Ellamonov Sukhrob Numanovich, Abdieva Gulnora Alievna, Analysis of Myocardial Structure Changes in Patients with Progressive Arterial Hypertension and Type 2 Diabetes, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 610-615. doi: 10.5923/j.ajmms.20241403.15.
1. Introduction
- The prevalence of diabetes mellitus (DM) continues to rise worldwide, increasing to 10% of the population in countries such as China and India, which are now adopting Western lifestyles. In 2017, it was estimated that 60 million European adults have type 2 diabetes, which is detected in 50% of cases, and the consequences of this condition for the health of the individual and their children/unborn children create additional public health problems that various organizations are trying to address worldwide. More than 600 million people are projected to have type 2 diabetes worldwide by 2045, and about the same number could be diagnosed with pre-diabetes [1]. At the same time, the majority of patients with type 2 diabetes have arterial hypertension (AH). Diabetic nephropathy, as one of the causes of hypertension, is detected in a third of patients with type 1 diabetes and in 20% of patients with type 2 diabetes. Among the causes of mortality in patients with diabetes, the leading place is occupied by cardiovascular causes. DM and AH are two mutually reinforcing and often unidirectional factors that have a damaging effect on the heart [2]. The risk of coronary heart disease (CHD) in patients with diabetes mellitus increases by more than 2 times, and the incidence of myocardial infarction is 3-5 times higher than in the general population. At the same time, the mortality rate of patients with type 2 diabetes mellitus from coronary artery disease and myocardial infarction is 2-4 times higher than in the general population [3]. The study of structural and functional changes in the left ventricular (LV) myocardium in patients with diabetes mellitus is associated with the fact that, being in conditions of constant hyperglycemia, metabolic disorders in the myocardium occur, due to which there is a deterioration in systolic and diastolic function. Therefore, these patients with diabetes require increased attention and alertness in terms of the early development of life-threatening arrhythmias, sudden death and more rapid progression, and decompensation of chronic heart failure (CHF). Regardless of whether CHD and CHF are complications of DM or a competing pathology developing in parallel with carbohydrate metabolism disorders, such patients represent one of the highest risk categories associated with increased mortality [4]. The above facts testify to the relevance of the chosen topic of this study, its theoretical and practical significance, which served as the basis for this work.Chronically increased left ventricular load in patients with hypertension may lead to LV hypertrophy, impaired LV relaxation, left atrial enlargement, increased risk of arrhythmias, especially atrial fibrillation, and increased risk of heart failure with preserved ejection fraction and heart failure with reduced ejection fraction [10]. Hypertension causes micro- and macroscopic myocardial changes, structural, phenotypic, and functional changes. This includes cardiac fibrosis and remodeling of individual heart chambers and arteries. The disease most often manifests itself as subclinical conditions, but diagnostically and prognostically it is a harbinger of further adverse outcomes or manifests as cardiovascular disease, which is worse in the short term [11]. Structural and functional changes in the left atrium (LP) are another feature of hypertension. Its remodeling is closely related to the geometric and functional changes of the LV but can also occur independently of each other. Left-atrial structural and functional changes are of great importance for the prognosis of clinical cases. In one previous study, the left atrial functional index (a new derived index that combines data on the structure and function of LP) was associated with a higher risk of developing atrial fibrillation and other cardiovascular diseases (CVDs) [12]. Remodeling of the left atrium reflects an adaptive process that can be manifested in persistent hypertension or in high blood pressure, which is superimposed on age-related changes in the LP [13]. Changes in the left atrium can occur alone or in combination with other changes that accompany hypertension. Fibrosis, cellular and molecular profibrotic cascades may occur in the left atrium, which may be in the interstitium or perivascular, but eventually progress to replacement fibrosis [14]. The Frank-Starling law also applies to the left atrium. As the size of the left atrium increases, the systolic pressure produced may initially improve, but as hypertension progresses, deviations from the Frank-Starling norm occur, leading to systolic dysfunction and dilatation of the left atrium [15]. Recent population-based studies have provided new evidence on the effect of high blood pressure on left atrial remodeling over time. In a previous study that looked at changes in left atrium size over the course of a lifetime, higher blood pressure was associated with an increase in the size of the left atrium [16]. In hypertension, there is 12 left atrial myopathy and an increase in size, a decrease in conduction function (under conditions of increased pressure), as well as a compensatory increase in its pumping function to maintain adequate LV filling [17].Purpose of the study:To assess the structural remodeling of the myocardium in patients with advanced hypertension and type 2 diabetes.
2. Materials and Methods of Research
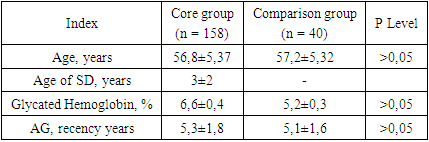
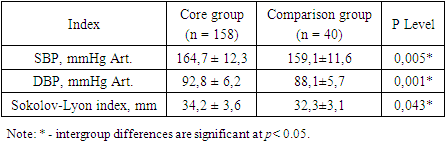
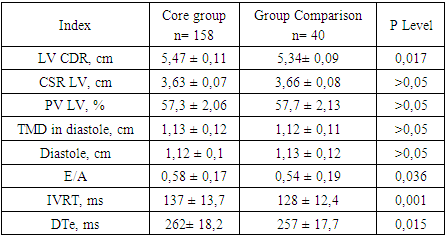
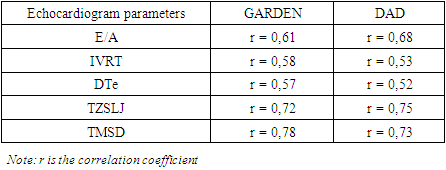
- This study was open-label, randomized, and prospective. All study participants underwent a questionnaire, a standard clinical examination, which included an assessment of complaints, life and disease history, and objective status. Laboratory tests included the determination and evaluation of the indicators of a complete blood count, a biochemical blood test. Instrumental examination included electrocardiography (ECG), ultrasound examination (US), echocardiography (echocardiography), coronary angiography (CAG). Patients were enrolled in the study after familiarization and signing of informed voluntary consent.The study was conducted on the basis of the Emergency Therapy Department of the Samarkand branch of the Republican Scientific Center for Emergency Medical Care for the period from 2020 to 2023 inclusive.The study included 198 patients with hypertension (mean age 57.6±5.48 years, 105 men and 93 women).To study the effect of type 2 diabetes on the clinical and instrumental characteristics of patients with hypertension, 2 groups of patients were formed. The main group consisted of 158 patients with hypertension and type 2 diabetes (84 men, 74 women, mean age 56.8 ± 5.37 years) who had clinical and instrumental signs of hypertension in combination with type 2 diabetes.The comparison group included 40 patients (21 men, 19 women, mean age 57.2±5.32 years) who had hypertension but did not have diagnostic criteria for diabetes.Standard diagnostic methods were carried out, including a general analysis of blood and urine. Blood glucose glucose, alanine aminotransferase, aspartate aminotransferase, blood creatinine, total cholesterol and its fractions were examined in the biochemical blood test, which had no statistical differences.A comprehensive laboratory and clinical-instrumental examination were carried out at baseline, after 1 and 2 months, as well as, if necessary, more often. The follow-up period was 2 months.Statistical data processing. Statistical analysis was performed on a computer using Microsoft Office Excel 2007, Statistica 22.0 for Windows, using parametric and nonparametric criteria. The correspondence of the distribution of the trait to the normal in the sample was checked using the Kolmogorov-Smirnov test. The deviation from the normal distribution was considered significant at p < 0.05. To test hypotheses about the correlation between certain traits and factors, use the ANOVA (Analysis of Variations) multivariate analysis. To determine the probabilistic relationship between two variables, use Spearman's rank correlation coefficient r.Outcomes.The data of the survey of 198 people presented in Table 1 were analyzed.
|
|
|
|
|
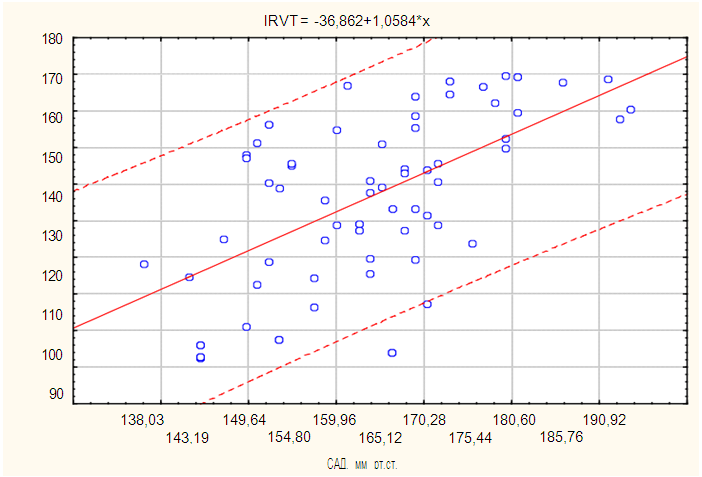 | Figure 1. Linear regression of SBP level and IVRT |
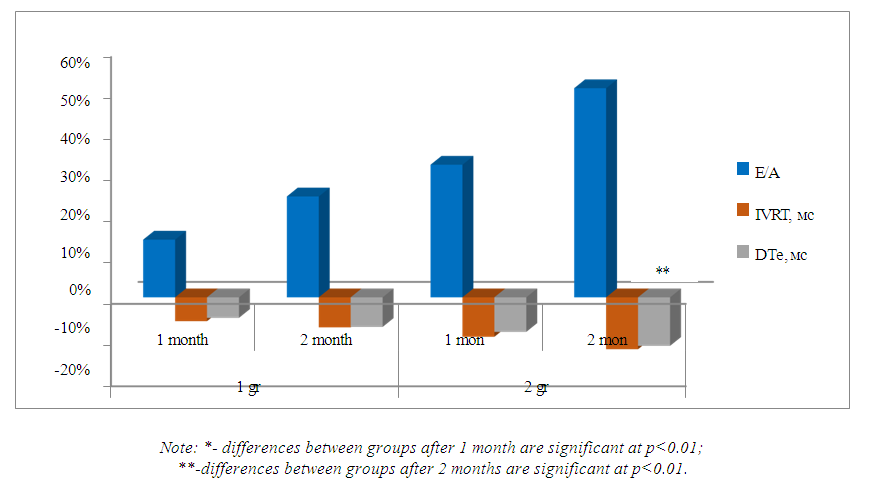 | Figure 2. Changes in left ventricular diastolic function in the compared groups over time |
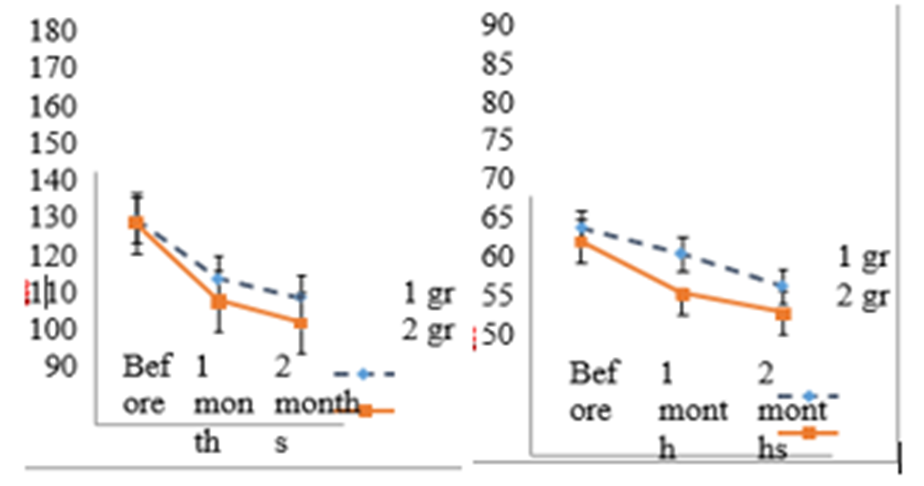 | Figure 3 and 4. Dynamics of SBP and DBP in patients of the first and second groups for 2 months of research |
3. Conclusions
- 1. In patients with hypertension and type 2 diabetes, in comparison with patients without diabetes, not only a higher level of blood pressure (SBP – by 5.6 mm Hg and DBP – by 4.7 mm Hg), but also the most significant increase in arterial vascular stiffness parameters was recorded: PWV – by 0.9 m/s, CAVI – by 0.77 m/s, and R-AI – by 1.8%; (p<0.05).2. According to echocardiography data, patients with hypertension with type 2 diabetes compared to those without diabetes have a more significant impairment of LV diastolic function (LV CDR is 0.13 cm higher, U/A ratio is 0.04 units, IVRT is 9 ms, DTe is 8 ms; (p<0.05)).3. The positive role of mexidol in achieving more effective blood pressure control in patients with hypertension against the background of type 2 diabetes compared to patients who did not receive this drug was determined, after one month it was expressed in a decrease in SBP by 36 vs. 29 mm Hg. DBP – by 12 vs. 9 mmHg. Art.4. A significant positive effect of mexidol supplementation in patients with hypertension and type 2 diabetes on vascular wall stiffness compared to standard antihypertensive therapy was established: a decrease in PWV by 32.9% vs. 7.7%, CAVI by 23.5% vs. 3.9%, R-AI by 36.3% vs. 3.8% (p<0.05).5. The possibility of regression of LV diastolic dysfunction in patients with hypertension and type 2 diabetes treated with mexidol compared to standard antihypertensive therapy was revealed, which was determined by a significant decrease in the U/A indicator by 50.8% vs. 24.5%, IVRT by 12.6% vs. 7.3%, DTe by 11.8% vs. 7.2% (p<0.05).6. Reduction of arterial vascular wall stiffness and myocardial diastolic dysfunction under the influence of mexidol can serve as a basis for the use of cytoprotective drugs in order to reduce the incidence of cardiovascular events (MI, stroke) in the treatment of patients with hypertension against the background of type 2 diabetes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML