Kh. A. Akilov, J. Kh. Ibragimov
Andijan State Medical Institute, Andijan, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The aim of the study was to improve the treatment results of children with congenital hydronephrosis through the differentiated use of surgical methods. Background. Currently, against the background of the rapid development and introduction of modern high-tech methods, the problem of congenital hydronephrosis remains relevant and is a relatively common disease of the urinary system. Actually, laparoscopic pyeloplasty is becoming the preferred method as an alternative to the classical approach and is gaining wide popularity. Material and methods. The study was based on an analysis of the results of treatment of 691 children with congenital hydronephrosis aged 3 to 15 years in the period from 2013 to 2022. In accordance with the goal of the study, the patients were divided into two groups: the comparison group - 337 (48.8%) children and the main group - 354 (51.2%) patients. Results. The average duration of open pyeloplasty using traditional access in the lumbar region (according to Fedorov) was 91 ± 12 minutes (p <0.05). The average duration of the surgery using laparoscopic access was 120 ± 11 minutes (p <0.05). Conclusion. The introduction of the developed methods (modified mini-access, drainage method, improved ureteropyelastomosis) in congenital hydronephrosis, regardless of the complications degree and the age of the child, allowed us to reduce the period of postoperative rehabilitation from 20.8±3.2 to 6±0.42 days, the need for injection of narcotic and non-narcotic analgesics decreased from 3.9±0.6 bed days to 1.0±0.2 bed-days (p <0.05).
Keywords:
Congenital hydronephrosis, Pyeloplasty, Mini-access, Advanced ureteropyelonastomosis
Cite this paper: Kh. A. Akilov, J. Kh. Ibragimov, Differentiated Approach in the Choice of Surgical Tactics for Congenital Hydronephrosis in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 602-606. doi: 10.5923/j.ajmms.20241403.13.
1. Introduction
Malformations of the urinary system organs in children rank first in terms of number and variety and make up 36% of the developmental anomalies of all organs and systems [1-5]. One of the most common (from 35 to 40%) of all registered malformations of the urinary system is congenital hydronephrosis (CH) and occurs with a frequency of 1:500 - 1:800 newborns, therefore, it is no coincidence that surgeries for this disease occupy first place among surgical interventions for malformations of the upper urinary tract [1,6-9,3].Ultrasound is most often used to diagnose malformations of the urinary system and their complications. However, despite the possibilities of modern ultrasound, it is possible to assess the degree of hydronephrosis, the functional state of the parenchyma only with a comprehensive examination [1,10-14].The first priority in the treatment of hydronephrosis is to restore urine passage from the kidney. It can only be accomplished through the use of surgical techniques. For this purpose, urologists perform open ureteroplasty at the site of narrowing; laparoscopic surgeries to repair defects; ureteral stenting without incisions (through natural openings of the urinary tract). Currently, against the background of the rapid development and introduction of modern high-tech methods, the problem of congenital hydronephrosis remains relevant and is a relatively common disease of the urinary system [1,6-9,3]. In the arsenal of surgical methods for the treatment of congenital hydronephrosis (CH), as an alternative to the classical approach, laparoscopic pyeloplasty is becoming a more preferable method and is gaining wide popularity [10,15,11]. However, the surgical treatment results of CH are not completely satisfactory, which is associated with a relatively high incidence of postoperative complications and mortality [16,2,10,17].The significant proportion and ambiguity of the treatment results of patients with hydronephrosis requires systematization in tactics and treatment accumulated in recent years. It will allow to justify the choice of surgical or conservative types of treatment.The aim of the study was to improve the treatment results of children with congenital hydronephrosis through the differentiated use of surgical methods.
2. Material and Methods
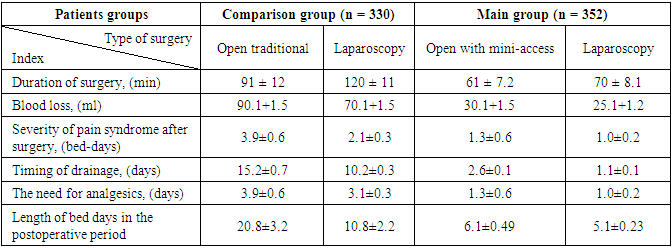
The study was based on an analysis of the treatment results of 691 children with congenital hydronephrosis aged 3 to 15 years on the basis of urological departments of three medical institutions in the Fergana Valley: Andijan Regional Children's Multidisciplinary Medical Center, Namangan Regional Children's Multidisciplinary Medical Center and Fegrana Regional Children's Multidisciplinary Medical Center of Urology in the period from 2013 to 2022. In accordance with the purpose of the study, the patients were divided into two groups: Comparison group - 337 (48.8%) children treated according to accepted standards for the management of patients with CH during the period from 2013 to 2017; Main group - 354 (51.2%) children treated in 2018-2022 on the basis of a developed tactical treatment and diagnostic algorithm and a modified pyeloplasty method, taking into account the timing of the development of CH, the possibilities of minimally invasive surgery (laparoscopy). Among the children included in the study, boys predominated (72.9%) compared to girls (27.1%). The overwhelming number of patients (45.1%), were more than 8-15 years old (school age) due to the late treatment of patients and their parents, despite the introduction of renal and urinary tract ultrasound in the mandatory protocol of antenatal and postnatal screening. Most children were admitted with pronounced clinical symptoms, when the kidney reaches enormous sizes and existing disorders in the urinary system (Fig. 1).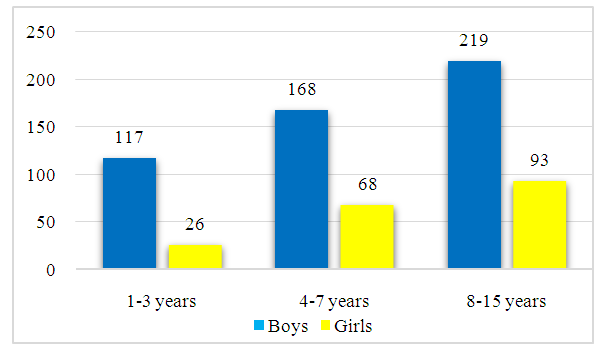 | Figure 1. Distribution of patients depending on age and gender |
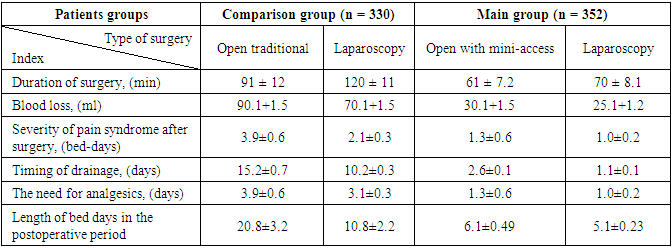
When determining the severity of obstruction of the pyelourethral segment, we used the classification proposed by the Society of Fetal Urology modified by Onen A. (2007)): hydronephrosis grade I – dilation of the renal pelvis; hydronephrosis grade II – expansion of the renal pelvis and calyces; hydronephrosis grade III – expansion of the pelvis, calyces and thinning of the parenchyma to ½; hydronephrosis grade IV – dilation of the pelvis and calyces with thinning of the parenchyma by more than ½. The maximum number of children were admitted to urology departments with stage III HC, which made up 75.3% of the total number of hospitalized patients (Fig. 2).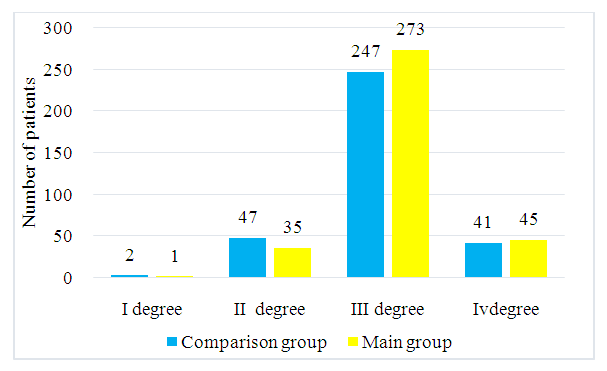 | Figure 2. Distribution of patients depending on the degree of hydronephrosis |
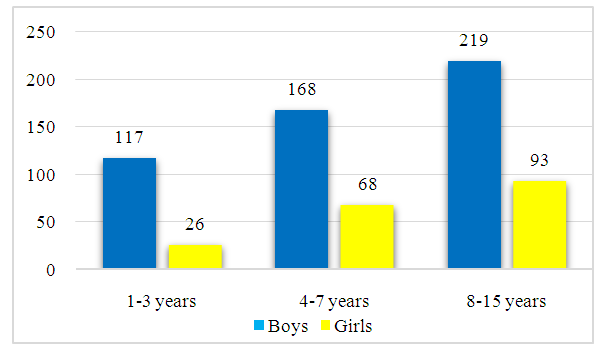
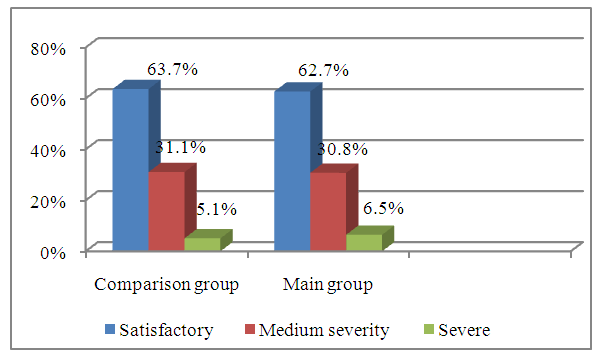
215 (63.7%) out of 337 children of the Comparison group were admitted in satisfactory condition; 105 (31.1%) children were in moderate condition and 17 (5.1%) - in severe condition. In the Main group, these indices were 222 (62,7%), 109 (30,8%) and 23 (6.5%), respectively (Fig. 3).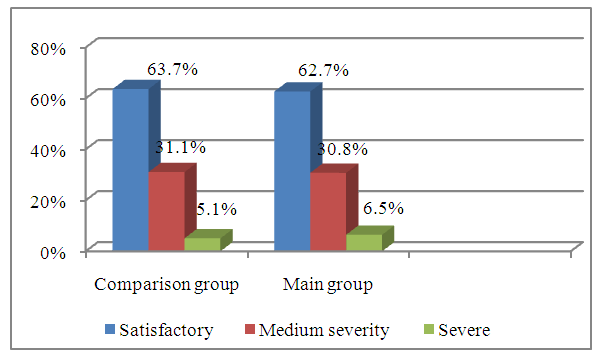 | Figure 3. Distribution of children by the condition severity at the time of admission |
Thus, in the vast majority of cases, clinical signs of CH were absent and the diagnosis was established by ultrasound, and most patients had changes in urine tests. Analysis of the degree of dysplastic changes in renal parenchyma and function, its differentiation and timely diagnosis are important for predicting possible outcomes of surgery. The following studies were carried out to assess the general somatic status of the patient: general blood test, assessment of biochemical blood parameters (urea, creatinine, electrolyte levels), state of the blood coagulation system, determination of blood group and Rh factor, testing for HIV infection, hepatitis and RW, performing a general clinical urine test, urine culture for microflora and sensitivity to antibiotics. All patients were performed electrocardiography and chest x-ray. Mandatory studies were performed in all patients to make a diagnosis, which included: ultrasound examination of the kidneys and urinary tract with color Doppler scanning, excretory urography, dynamic or static nephroscintigraphy. In the Main group of patients, the above research methods were used for differentiated diagnosis of complex cases. Instead of routine numerous instrumental studies, we carried out a combination of ultrasound, excretory urography with MSCT, which saved time and radiation load on the child.
3. Results
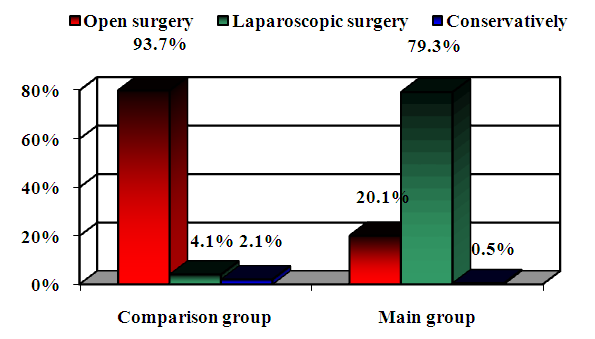
Surgical intervention was performed in 330 (97.9%) patients of the Comparison group and in 352 (99.4%) patients from the Main group. However, it should be noted that the main surgical intervention in patients of the comparison group was open surgery (93.7%), whereas in patients of the main group the proportion of open intervention made up only 20.1% (71 patients), laparoscopic intervention was used in 281 (79.3%) children (Fig. 4).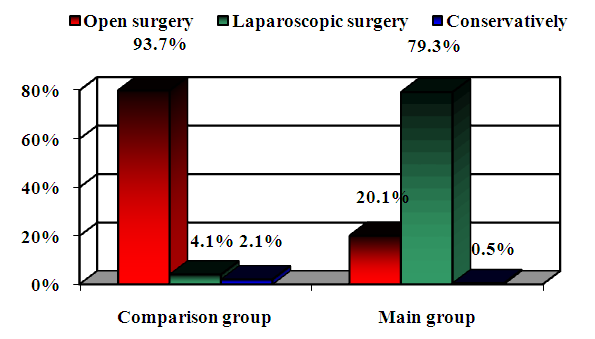 | Figure 4. Analysis of performed surgical interventions |
Thus, the comparative analysis of CH treatment results showed that in the Main group of patients there was an increase in the proportion (from 20.1% to 79.3%, p=0.001) of laparoscopic technique of surgeries, replacing open surgical interventions with the possibility of laparoscopic technologies (93.7% and 4.1% in the Comparison group).In the Comparison group, classic lateral lumbotomy with a wide incision according to Fedorov up to 10 cm prevailed - in 316 (93.7%) children, especially in young children (18.3%), which subsequently led to the occurrence of postoperative hernias and cicatricial deformities of skin in the younger generation of children. There were 242 (71,8%) boys and 83 (26,1%) girls among them.Laparoscopic approaches were used in the initial period of introduction of minimally invasive techniques, which was used only in 14 (4.1%) children, with conversion to traditional access in 6 (42.8%) out of them. There were attempts to perform laparoscopic retroperitoneal access in children aged 1-3 years (1.2%), due to the fact that at this age the tissue structure is thin and the retroperitoneal space is undeveloped, various complications developed during surgery and in the postoperative period. Laparoscopic transperitoneal access was used in 8 (2.4%) children.Conservative measures were performed in 5 (1.5%) children with hydronephrosis grade I and II and in 2 (0.6%) children with hydronephrosis grade IV with comorbidities (chronic renal failure). It was decided to perform dynamic follow-up in these patients.The average duration of open pyeloplasty using a traditional approach in the lumbar region (according to Fedorov) was 91 ± 12 minutes (р<0.05). The average duration of surgery using laparoscopic access was 120 ± 11 min (р<0.05). This low percentage of laparoscopic accesses was attributed to inadequate experience, lack of specialists, and equipment limitations in general. Retrospective analysis of the surgical treatment results in the Comparison group showed that a number of tactical and technical omissions were made. They were as follows:• the use of wide laparotomy according to Fedorov with the intersection of a large array of muscles (transverse intersection of the fascia 12-14 cm long and the vastus dorsi muscle, external and internal oblique and transverse abdominal muscles, as well as partially the posteroinferior scalene and quadratus lumborum muscles), was often the cause of postoperative lumbar hernia, damage to the XII intercostal nerve during tissue dissection or its capture in the suture with a needle while suturing the edges of the wound, which in the postoperative period leads to relaxation, paresis of the muscles innervated by it, postoperative pain in the incision area; • the nature of changes in the pelvic-ureteric segment, localization and diameter of obstruction were not taken into account when determining surgical tactics and choosing the method of surgery in a comprehensive manner;• pyeloplasty was performed at diagnosis of pyelonephritis without preliminary correction of inflammatory processes and concomitant pathologies;• the desire for a low-traumatic approach during laparoscopy was a frequent reason for conversion. Thus, a retrospective analysis of the surgical treatment results showed that in a number of cases, tactical and technical omissions were made: the use of excessively large unnecessary routine preoperative diagnostic complexes, which did not always provide fundamentally new information. At the same time, the use of excessive preoperative diagnostic methods led to fatigue of children and sometimes were the motive for the refusal of patients and their parents from urgently needed surgical treatment, which led to an aggravation of existing complications of CH. When draining the ureteropelvic segment, long-term drainage up to 20-23 days sometimes led to ascending infection and prolonged hospitalization of the child.In the Main group, open pyeloplasty was performed using an improved posterolateral lumbotomy by mini-access with an incision of no more than 5 cm in 71 (20.1%) children, especially in young children (9.8%). There were 48 (13.5%) boys and 23 (6.5%) girls.
4. Discussion
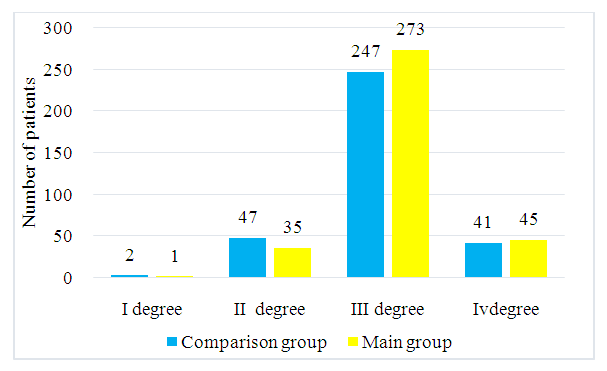
The experience of laparoscopic surgeries has shown that in minimally invasive interventions there is a need to use such incisions, which, being not so traumatic, would create a wide and convenient for the surgeon access to all parts of the ureteropelvic segment.Based on the shortcomings and omissions in the Comparison group and the accumulation of experience with minimally invasive methods of kidney surgery (laparoscopy) led to an increase in the number of laparoscopic accesses - in 281 (79.3%) children, with conversion to a modified posterior-lateral mini-access in only 1 (0.3% of 281) of them. There were 208 (58,7%) boys and 73 (20,6%) girls.It should be noted that in 1 (0.28%) child with hydronephrosis grade I and in 1 (0.8%) child with hydronephrosis grade IV, conservative measures were performed due to parental refusal of surgery due to the severity of the child's condition. It was decided to perform dynamic follow-up in these patients.The average duration of open pyeloplasty using a modified mini-access in the posterolateral lumbar surface (according to the clinic method) was 61 ± 7 min, 30 ± 5 min shorter than in the Сomparison group (91 ± 12 min) (р<0.05). The average duration of surgery using laparoscopic access was 70 ± 8 min, i.e. 50 ± 3 min shorter than in the Сomparison group (120 ± 11 min) (р<0.05).To assess the immediate surgical treatment results of congenital hydronephrosis, the following clinical parameters were taken into account (Tab. 1): - Duration of the intervention. - Duration of anesthesia.- The amount of blood loss.- The severity of pain syndrome in the postoperative period. - Timing of drainage. - The need for analgesics in days.- Duration of bed-days in the postoperative period.Table 1. Comparison of clinical efficacy of surgical treatment in the groups
 |
| |
|
As it can be seen, when comparing the immediate treatment results by parameters, the duration of surgery differed significantly between the groups. The duration of the surgery using the open method with the classic access in the Comparison group was 91 ± 12 min, in the Main group with the use of a mini-access - 61 ± 7.2 min. In the initial period of development and implementation of laparoscopic interventions, the duration of surgery using laparoscopic access in the Comparison group was 120 ± 11 minutes. Subsequently, with the accumulation of experience, in the Main group the duration of the surgery made up 70 ± 8.1 minutes. The duration of anesthesia using the open method with mini-access was 68.3 + 1.5 minutes, with laparoscopic access - 80 ± 3.1 minutes.One of the important criteria for the invasiveness of surgery is blood loss. In the Main group, all surgeries with open minilumbotomy and laparoscopic ureteropyeloanastomy were accompanied by minimal blood loss. At the same time, the volume of blood loss with the open method in the Main group made up 30.1 +1.5 ml vs blood loss in the Comparison group with a volume of 90.1 + 1.5 ml. Laparoscopic surgeries in the Main group were also marked by low blood loss of 25.1+1.2 ml vs blood loss in the comparison group of 70.1+1.5 ml.At the same time, depending on the pain severity, the need for injection of narcotic and non-narcotic analgesics in the Comparison group after classical open surgery was 3.9± 0.6 bed days. In the Main group, after modified posterolateral mini-access, they were needed for 1.3±0.6 bed days, after laparoscopic ureteropyeloanastomosis – for 1.0±0.2 bed days.The drainage time after laparoscopic pyeloplasty in the Main group averaged 1.1± 0.1 days. In patients after open surgery with mini-access, the drainage time was comparable to patients with laparoscopic ureterpyeloanastomosis and averaged 2.6± 0.1 days, whereas in the Comparison group, the drainage time after traditional open surgery averaged 15.2±0.7 days, after laparoscopic surgery - 10.2± 0.3 days.
5. Conclusions
The introduction of the developed methods (modified mini-access, drainage method, improved ureteropyelonastomosis) for congenital hydronephrosis, regardless of the complications degree and the age of the child, allowed to reduce the period of postoperative rehabilitation from 20.8±3.2 to 6±0.42 days, the need for injection of narcotic and non-narcotic analgesics from 3.9±0.6 bed days to 1.0±0.2 bed days (p<0.05).At the same time, drainage-free postoperative management of patients with improved ureteropyeloanastomosis is effective and safe in most children with congenital hydronephrosis, allowing to reduce the trauma of the surgery, postoperative psychological trauma of patients and practically eliminate urinary tract infection (the duration of drainage was reduced from 15.2 ± 0.7 days to 2 .6±0.1 days).
Conflict of Interests
The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
ACKNOWLEDGEMENTS
The authors express their gratitude to the management of the mentioned medical institutions for the material provided for our study.
References
| [1] | Ageeva N.A. Comparative analysis of various methods for diagnosing an aberrant renal vessel in hydronephrosis in children. / Kovarsky S.L., Zakharov A.I., Ageeva N.A., et al. // Materials of the V Forum of Pediatric Surgeons of Russia. - Ufa. - 2019. -P. 82-83. |
| [2] | Struyansky K.A. Comparative assessment of endovideosurgical approaches in congenital hydronephrosis in children: abstract. diss. ...candidate of Medical Sciences. - Moscow, 2020. - P.22. |
| [3] | Futurov N.F. Tactics of management of patients with hydronephrosis / N.F. Futurov H.G. Salimov, Sh.M. Tusmatov // Mat. annual scientific and practical conference of young scientists and students of Abuali ibni Sino TSMU with international participation "Topical issues and problems of medical science". - Dushanbe, 2013. - P.160. |
| [4] | Onen A. An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis // J Pediatr Urol. - 2007. - Vol. 3. - P. 200-205. |
| [5] | Rickard, M. Lorenzo A.J., Braga L.H. Renal parenchyma to hydronephrosis area ratio (PHAR) as a predictor of future surgical intervention for infants with high-grade prenatal hydronephrosis // Urology. - 2017. - V. 101. - Р. 85-89. doi: 10.1016/j.urology.2016.09.029. |
| [6] | Agzamkhodzhaev S.T. The current state of the problem of treatment of congenital hydronephrosis in children // Pediatrics. - Tashkent. - No.3. - 2017. - pp. 121-125. (14.00.00, No. 16). |
| [7] | Beknazarov J.B., Agzamkhodjaev S.T., Abdullaev Z.B. and others. Results of surgical correction of congenital hydronephrosis in young children // Russian Bulletin of Pediatric Surgery, Anesthesiology and Intensive Care. - Moscow. - 2018. - No. 1. - P.9-12. (14.00.00, № 121). |
| [8] | Zorkin S.N., Gubarev V.I., Salnikov V.Yu., Filinov I.V., Petrov E.I., Malikov Sh.G., Ponomarchuk I.N. Endoscopic balloon dilation of high pressure as a method of treatment of pelvic ureteral segment obstruction in children. Bulletin of Urology. 2017; 2: 5-11. |
| [9] | Mavlyanov F.Sh., Mavlyanov Sh.Kh. A clinical case of a good result of surgical treatment of congenital bilateral hydronephrosis of the III degree // Urology. - Uzbek journal of case reports. 2021. Vol.1, No.1. - pp. 22-25. |
| [10] | Sultanov S.R. Features of the tactics of surgical treatment of congenital hydronephrosis caused by an aberrant vessel / Sh.R Sultonov, A.M. Sattorov, D.M. Makhmajonov // Bulletin of Avicenna. -2015. -No.2. - pp. 69-72. |
| [11] | Aulbert, W. Severe antenatally diagnosed renal disorders: background, prognosis and practical approach / W. Aulbert, M.J. Kemper // Pediatr Nephrol. - 2016. - V.31 (4). - Р. 563-574. |
| [12] | den Bakker E. Endogenous markers for kidney function in children: a review / E. den Bakker, R.J.B.J. Gemke, A. Bökenkamp // Crit Rev Clin Lab Sci. - 2018. - V. 55. - Р. 163-183. |
| [13] | Dias C.S., Silva J.M., Pereira A.K. et al Diagnostic accuracy of renal pelvic dilatation for detecting surgically managed ureteropelvic junction // J. Urol. - 2013. - Vol. 190, (Suppl. 2). - P. 661-666. |
| [14] | Vasconcelos M.A., Oliveira E.A., A.C. Simões e Silva, Dias C.S., Mak R.H., Fonseca C.C., Campos A.P.M., Steyerberg E.W., Vergouwe Y. A Predictive Model of Postnatal Surgical Intervention in Children With Prenatally Detected Congenital Anomalies of the Kidney and Urinary Tract // Front. Pediatr. - 2019. - V. 7. - Р. 120. doi: 10.3389/fped.2019.00120. |
| [15] | Kharmish O.S., Smirnova Ya.V., Fomchenko K.A., et al. Nephroprotection in operative urology // Medicine of the nevidkladnih staniv. - 2018. - vol. 92. - No. 5. - pp. 119-122. |
| [16] | Vrublevsky S.G., Shmyrov O.S., Vrublevskaya E.N., Lazishvili M.N., Kulaev A.V., Korochkin M.V., Vrublevsky A.S. Laparoscopic pyeloplasty in children: technique, drainage, complications. Pediatric surgery.2017; 6: 299-302. |
| [17] | De Bessa, Jr. Diagnostic accuracy of Onen's Alternative Grading System combined with Doppler evaluation of ureteral jets as an alternative in the diagnosis of obstructive hydronephrosis in children / Jr. De Bessa et al. // PeerJ. - 2018. - 6:e4791; DOI 10.7717/peerj.4791. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML