-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 583-585
doi:10.5923/j.ajmms.20241403.09
Received: Feb. 5, 2024; Accepted: Feb. 28, 2024; Published: Mar. 4, 2024

Features of Cytokine Status in Children with Type 1 Diabetes Who have Suffered COVID-19 Infection
Sadirkhodjaeva Azizakhon Alavitdinovna, Ashurova Dilfuza Tashpulatovna
Department of Propaedeutics of Childhood Diseases, Tashkent Pediatric Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To study the features of serum cytokines in children with type 1 diabetes mellitus who have suffered COVID-19 infection. For our study, 140 children with type 1 diabetes who suffered from COVID-19 were treated in the children's department of the RSNPMC endocrinology aged 2 to 18 years. The comparison group was 65 children with type 1 diabetes, a group of 15 practical healthy children matched for age and sex without any signs or symptoms of cardiovascular disease was used as a control. The work uses immunological research methods and statistical research methods. In patients with diabetes mellitus and cardiac complications, there were multidirectional changes in a number of pro-inflammatory cytokines: a decrease in the level of Il-17p, with an increased content of Il 1.10 and TNF-a.
Keywords: Type 1 diabetes mellitus, Children interleukins, COVID-19
Cite this paper: Sadirkhodjaeva Azizakhon Alavitdinovna, Ashurova Dilfuza Tashpulatovna, Features of Cytokine Status in Children with Type 1 Diabetes Who have Suffered COVID-19 Infection, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 583-585. doi: 10.5923/j.ajmms.20241403.09.
Article Outline
1. Relevance
- Currently, SARS-CoV-2 infection is also a potential trigger for the development of type 1 diabetes mellitus in children, which represents the most common chronic metabolic disorder in the pediatric population. There is growing evidence that many patients with COVID-19 may experience a wide range of post-acute consequences, including cardiovascular complications [2]. COVID-19 causes not only viral pneumonia, but also many extrapulmonary complications, such as cardiovascular or cerebrovascular diseases. COVID-19 can excessively stimulate the sympathetic system and cause an inflammatory cytokine storm and a state of hypercoagulopathy. These mechanisms can cause irreversible damage to the cardiovascular or respiratory system even after recovery from COVID-19. [5].Type 1 diabetes mellitus (SD1) is one of the most common chronic diseases affecting children. In this disease, various micro- and macrovascular complications are often observed, which leads to at least a 10-fold increase in cardiovascular morbidity compared to healthy people of the same age [1,3]. Diabetes mellitus is characterized by a variety of cardiovascular complications. Currently, there is strong evidence on the role in the formation of chronic heart failure of cytokines such as interleukin-1 (IL-1), tumor necrosis factor-a (TNFa), interleukin-6 (IL-6), manifested by the gradual destruction of the extracellular collagen myocardial matrix followed by cardiomyocyte hypertrophy and cavity dilation [6].Diabetes mellitus is characterized by various cardiovascular complications including myocarditis. Myocarditis occurs as a result of a COVID-19 infection. Pathogenetically, myocarditis leads to diastolic and systolic dysfunction, and finally to congestive heart failure [2,7].Over the past 10 years, numerous data have been accumulated on the role of the cytokine system in the pathogenesis of cardiovascular disease. Cytokines are a group of polypeptide mediators of intercellular interaction. Cytokine-induced processes promote myocardial remodeling with irreversible cavity dilation and hypertrophy, process activation processes of cardiomyocyte apoptosis [1,3]. Currently, there are strong data on the role in the formation of chronic heart failure of cytokines such as interleukin-1, tumor necrosis factor-a (TNF-a), interleukin-6, manifested by the gradual destruction of the extracellular collagen myocardial matrix followed by cardiomyocyte hypertrophy and cavity dilation [4,5].
2. Purpose of the Study
- To study the features of serum cytokines in children with type 1 diabetes mellitus who have suffered COVID-19 infection.
3. Research Materials and Methods
- For our study, 140 children with type 1 diabetes who suffered from COVID-19 were treated in the children's department of the RSNPMC endocrinology aged 2 to 18 years. The comparison group was 65 children with type 1 diabetes, a group of 15 practical healthy children matched for age and sex without any signs or symptoms of cardiovascular disease was used as a control. The work uses immunological research methods and statistical research methods.
4. Results and Discussion
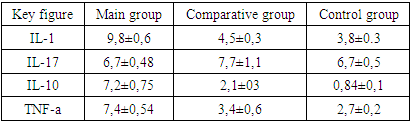
- As can be seen from the data presented in Table 1, in patients with diabetes mellitus who have undergone COVID-19 infection, there was no statistically significant difference in age, duration of diabetes mellitus and gender compared to the group without COVID-19 infection.During the study of cytokine content in children with type 1 diabetes mellitus who underwent COVID-19 infection, multidirectional changes were obtained. Thus, the level of IL-17 in patients with diabetes mellitus who underwent COVID-19 was infectious compared to the comparison group. The concentration of some pro-inflammatory cytokines was higher in patients with diabetes mellitus, especially significant in the presence of transferred COVID-19 Infections. When comparing two groups of patients, we found that in the group with children with diabetes mellitus who had undergone COVID-19, the infection exceeded the level of TNF a. It is noteworthy that the concentration of TNF-a in patients with diabetes mellitus without COVID-19 infection did not differ from the indicator of the control group, on the basis of this we consider it possible to consider the concentration of this cytokine as a specific marker of diabetic myocardial injury.There was a tendency to increase the content of IL-17 in the blood serum of the studied patients, but no statistically significant difference between the groups was detected.In patients with diabetes mellitus, the concentration of anti-inflammatory IL-10 increased depending on the presence of COVID-19 infection. Thus, in this group, its content exceeded the control and comparison groups
|
5. Conclusions
- In patients with diabetes mellitus and cardiac complications, there were multidirectional changes in a number of pro-inflammatory cytokines: a decrease in the level of Il-17p, with an increased content of Il 1.10 and TNF-a. An increase in TNF-a concentration in patients with type 1 diabetes mellitus who underwent COVID-19 infection was accompanied by an increase in the level of anti-inflammatory cytokine Il 1.10.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML