-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 572-574
doi:10.5923/j.ajmms.20241403.07
Received: Feb. 12, 2024; Accepted: Feb. 28, 2024; Published: Mar. 2, 2024

Immunological Markers of Viral-Associated Glomerulonephritis in Children
Ergasheva Mukharram Uktamovna
Bukhara State Medical Institute, Uzbekistan
Correspondence to: Ergasheva Mukharram Uktamovna, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Inflammatory and destructive processes of renal parenchyma occur long before the clinical manifestation of glomerulonephritis. In our study, the levels of proinflammatory cytokines, chemokines in blood serum and urine were used as diagnostic and prognostic indicators for kidney diseases. Autor conducted a new method of urocytokinodiagnostics as a non-invasive method for determining cytokines most effectively reflects the immune response of the kidneys, regardless of distorting factors that may occur during blood analysis. Timely detection of urine cytokines in patients with glomerulonephritis contributes to early prognosis of renal failure, prolongation of the remission period with improvement of GFR indicators and correct determination of therapeutic tactics.
Keywords: Immunity, Cytokines, Glomerulonephritis, Chronic kidney disease, Children, Virus
Cite this paper: Ergasheva Mukharram Uktamovna, Immunological Markers of Viral-Associated Glomerulonephritis in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 572-574. doi: 10.5923/j.ajmms.20241403.07.
1. Introduction
- Glomerulonephritis remains the most important problem of pediatric nephrology. According to many researchers, chronic glomerulonephritis (CGN) is one of the main causes of chronic renal failure among acquired diseases in children. A number of researchers believe that hypertension and proteinuria are the most important independent risk factors for the progression of kidney disease. Other factors contributing to the progression of renal dysfunction include dyslipidemia, anemia and impaired lipid metabolism emphasize the role of genetic risk factors in the progression of chronic kidney disease. At the same time, questions about the role of individual risk factors in the chronization of glomerulonephritis in children remain not fully clarified [1,4,8].CGN occurs against the background of slowly progressive destruction of the glomeruli of the kidney with progressive functional loss of the kidneys. In some cases, the cause is a specific attack on the body's immune system, but in most cases the cause is unknown. It is generally believed that an unidentified abnormality of the immune system is to blame [2,5]. One of the promising directions in this sense is the study of immuno-inflammatory mechanisms of kidney damage, in particular, the determination of the role of proinflammatory and profibrogenic molecular mediators of tissue damage in the processes of cell proliferation and pathogenesis of fibrosclerotic changes in renal tissue [6,10].The most common immunopathogenetic mechanism for the development of glomerulonephritis is immunocomplex, which occurs in 70-80% of the total number of patients with glomerulonephritis [7].Currently, herpesvirus infections are one of the most pressing medical and social problems worldwide. There are 8 antigenic serotypes of viruses pathogenic to humans belonging to this family: herpes simplex viruses of the 1st, 2nd type, varicella zoster, cytomegalovirus, Epstein-Barr virus, human herpes viruses of the 6th, 7th and 8th types. According to seroepidemiological studies, antibodies to HSV-1,2 are detected in 70-100% of the adult population of the globe, to EBV — in 95%, CMV — in 60%, HCV6 — in 80-100% [3]. A characteristic feature of all herpetic infections is lifelong persistence in the body of an infected person, pantropism to organs and tissues and the ability to cause diverse manifest forms of the disease, especially in conditions of immunodeficiency [9].The purpose of the study: The use of urocytokinodiagnostics to assess the immune response in children with glomerulonephritis.
2. Materials and Methods of Research
- In order to study the state of cytokine synthesis in children with CGN, in order to develop informative indicators of the severity of the course and outcome, we selected sick children taking into account the association of the underlying disease with CMV infection. For the convenience of comparing the main indicators of the severity of the sick children, they were divided into 2 groups depending on the association with CMV infection:1-the main group consists of 35 sick children with CGN nephrotic form;The 2-comparison group consists of 35 sick children with CMV-associated HCG nephrotic form;The control group consisted of 31 healthy children of the appropriate age.
3. Results
- As a result of the assessment of the state of synthesis of proinflammatory cytokines in children, an increase of IL-18 by 2.0 times was found in children of group 2 against the control -30.2±4.6 pg/ml (p<0.05), a decrease by 1.2 times against the indicators of group 1 - 78.2±7.1 pg/ml (p<0.05) (fig. 1).
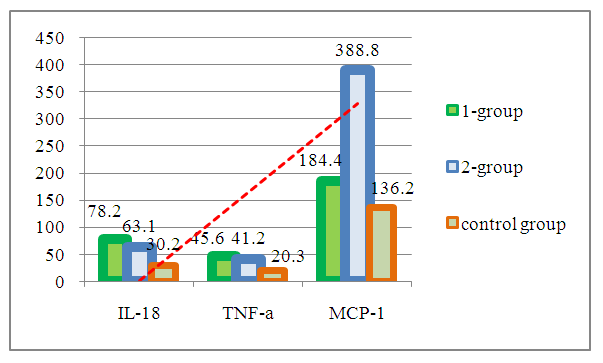 | Figure 1. Serum cytokines in chronic glomerulonephritis in children |
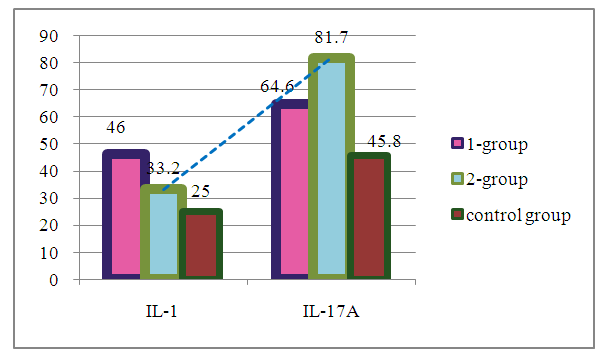 | Figure 2. Urine cytokines in chronic glomerulonephritis in children |
4. Conclusions
- An increase in the concentration of IL-18 in serum and IL-1β in urine relative to the control group in CGN was an indicator of the severity of an autoimmune reaction, and a relatively low concentration of cytokines in both blood and urine in CGN with CMV indicated suppression of specific antiviral immunity of CMVI.It was found that an increase in serum MCP-1 by 1.4 times in group 1 and 2.9 times in group 2 of HCG with CMV is an indicator of viral kidney damage. A significantly high concentration of IL-17A in urine in CGN with CMV indicated local cytokine production in the kidneys and acted as an indicator of the prognosis of the outcome of CGN.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML