-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(3): 568-571
doi:10.5923/j.ajmms.20241403.06
Received: Feb. 10, 2024; Accepted: Feb. 26, 2024; Published: Mar. 2, 2024

Immunological Parameters of Urgent Conditions in Respiratory Diseases in Children
Rajabov Shukhrat Juraboyevich, Navruzova Shakar Istamovna
Bukhara State Medical Institute, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Reducing the incidence of acute infectious respiratory diseases in children and mortality is currently considered as a strategic direction for the development of pediatric care in modern healthcare. According to modern concepts, innate immunity plays an important role in the implementation of the body's immune response in the early stages of infectious diseases. The authors conducted a study of indicators of humoral and cellular immunity in children to predict the development of emergency conditions in respiratory diseases in children. IgG control in dynamics determines the prognosis of the development of critical conditions in respiratory diseases in children. As an indicator of humoral immunity, IgG plays a complex role in the process of protecting against the re-entry of foreign antigen into the body, which prevents reinfection.
Keywords: Cellular immunity, Cytokines, Children, Respiratory diseases, Immune response, Urgent conditions
Cite this paper: Rajabov Shukhrat Juraboyevich, Navruzova Shakar Istamovna, Immunological Parameters of Urgent Conditions in Respiratory Diseases in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 3, 2024, pp. 568-571. doi: 10.5923/j.ajmms.20241403.06.
1. Introduction
- According to the World Health Organization (WHO), in the global structure of pathologies of children, the incidence of infectious diseases is more than 90%. Infectious agents are the cause of 35% of deaths among children [3].Over the past 4 years, there has been an increase in the number of children's intensive care units (ICU) by 17.8%, while deaths have decreased by 38% of the total number of cases. Infants, toddlers, and high school age children predominate among all pediatric ICU patients. More than 60% of the total mortality of patients in children's intensive care units is due to unfavorable outcomes of critical conditions in children of the first three years of life.In Switzerland and Italy, almost 50% of the total number of pediatrician consultations are conducted for acute respiratory diseases (ARI), in the USA acute respiratory infections are one of the main causes of hospitalizations, in the Russian Federation – 90% of outpatient visits and home visits are for respiratory diseases [1].Common clinical manifestations are general malaise, increased body temperature, fatigue, general weakness, decreased appetite, refusal of breast milk or difficulty sucking in infants, unreasonable anxiety, headaches, sore throat, difficulty nasal breathing, runny nose (rhinorrhea), hoarseness of voice, cough (dry and wet), lymphadenopathy, abdominal syndrome (with adenovirus infection). In the severe course of certain diseases, the appearance of inspiratory and expiratory odors is possible. In severe cases of certain forms of respiratory tract diseases, severe cephalgia, repeated vomiting, convulsive syndrome and loss of consciousness (symptoms of damage to the meninges and cerebral edema) may also appear. It is also possible to have complaints such as nausea, sometimes vomiting, a feeling of palpitations or interruptions in the heart area, which is a manifestation of the general intoxication syndrome [2,4,10].Among patients of this category, complaints of acute rhinitis and/or cough and/or conjunctival hyperemia (catarrhal conjunctivitis) in combination with rhinitis and pharyngitis are more common. The disease usually begins acutely, often accompanied by an increase in body temperature to subfebrile figures. Febrile fever is more typical for influenza, adenovirus infection, and enterovirus infections. Fever in 82% of patients passes on the second and third days of the disease; it lasts for a long time (up to 5-7 days), the febrile temperature persists with influenza and adenovirus infection [9].An increase in body temperature during the course of the disease, a symptom of pronounced intoxication in a child should be alert to the addition of a bacterial infection. Recurrent fever after a short-term improvement in the condition is often observed with the development of acute otitis media on the background of prolonged rhinorrhea [7].The purpose of the research: The study and analyzing of immunological parameters of urgent conditions in respiratory diseases in children.
2. Materials and Methods of Research
- The analysis of the structure of urgent conditions in children with respiratory diseases hospitalized in the pediatric intensive care unit of the Vabkent district Medical Association of the Bukhara region in the period 2019-2021 was carried out.In total, 361 sick children with urgent conditions who were hospitalized for respiratory diseases during the studied period were transferred to the intensive care unit. During their stay in the hospital, all patients were subjected to general clinical, laboratory, functional, biochemical, immunological and X-ray examinations.
3. Results
- To study the state of immunity, blood tests were performed on the parameters of cellular and humoral immunity.As a result of the assessment of the parameters of cellular immunity in the blood of children, it was found that the relative content of CD3 lymphocytes in group 1 exceeded the upper limit of the concentration range of these indicators in comparison group 2.At the same time, the level of CD3 lymphocytes in patients of the comparison group (33.34±2.52%) was significantly reduced against the control and indicators of the main group: 41.65±1.41% and 42.14±1.38%, respectively (p <0.05). A statistically significant increase in the level of CD4+, CD8+, CD16+, CD25+ and CD95+lymphocytes was found in patients of the main group in relation to the indicators of the control group and the comparison group (p <0.05).Cytotoxic T lymphocytes with the CD3+CD8+ phenotype are known to play a leading role in protecting against intracellular pathogens and their own altered cells [10].The necessary completion of an effective immune response is the programmed death (apoptosis) of activated cells, the induction of which involves signals leading to the activation of specialized "death receptors" [8]. Consequently, the urgent condition in children with respiratory diseases is accompanied by activation of helper, suppressor and killer activity and the processes of early cell proliferation and apoptosis (Fig. 1).
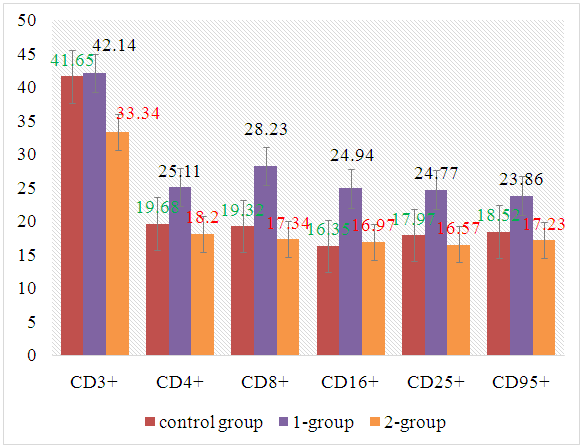 | Figure 1. Indicators of cellular immunity in respiratory diseases in children |
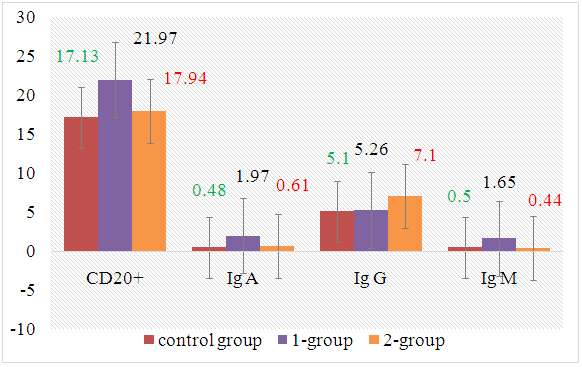 | Figure 2. Indicators of humoral immunity in children with respiratory diseases |
4. Conclusions
- The urgent condition in children with respiratory diseases is accompanied by activation of helper, suppressor and killer activity and processes of early cell proliferation and apoptosis. Immunoglobulin G is an indicator of the severity and prognosis of the development of urgent conditions in respiratory diseases in children. The introduction of the definition of immunoglobulin G in the medical practice of general practitioners, pediatricians, pediatric intensive care specialists in district medical associations and in the intensive care unit of emergency medical centers allows reducing the frequency of urgent conditions in respiratory diseases in children, and also contributes to saving the state budget in the hospital.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML